Abstract
Purpose
A population-wide study was conducted to determine the association between area-level socioeconomic status and prostate cancer mortality in Taiwan.
Methods
Age–period–cohort analysis was performed to adjust the time-trend variation. The area-level socioeconomic factors included proportion with a higher education, average income tax, population density, and clinical workload.
Results
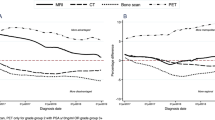
After adjustment for time-trend variations in age, period, and cohort, prostate cancer mortality was significantly lower in the groups with the highest higher education proportion (rate ratio 0.88; 95% Confidence Intervals 0.83–0.93), average income tax (RR 0.90; 95% CIs 0.86–0.94), and population density (RR 0.88; 95% CI 0.83–0.93). When all variables were incorporated into one model, the rate ratio of prostate cancer mortality was 0.92 (95% CIs 0.88–0.97) in the region with the highest average income tax level compared with that with the lowest level, but differences in the other socioeconomic factors were not significant.
Conclusions
This study revealed a significantly lower prostate cancer mortality rate in areas with a high higher education proportion, average income tax level, and population density compared with areas of low socioeconomic status in Taiwan.


Similar content being viewed by others
Data availability
The data that support the findings of this study are not publicly available but can be obtained from the corresponding author.
Code availability
Software SAS 9.4.
Abbreviations
- APC:
-
Age–period–cohort
- ICD:
-
International Classification of Diseases
- LAAs:
-
Local administrative areas
- SEGIS:
-
Socio-Economic Geographic Information System
- WHO:
-
World Health Organization
- PSA:
-
Prostate-specific antigen
References
Center MM, Jemal A, Lortet-Tieulent J et al (2012) International variation in prostate cancer incidence and mortality rates. Eur Urol 61:1079–1092
U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2013 Incidence and Mortality Web-based Report. Atlanta (GA): Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute; 2016. http://www.cdc.gov/uscs
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68:7–30
Malvezzi M, Carioli G, Bertuccio P et al (2016) European cancer mortality predictions for the year 2016 with focus on leukaemias. Ann Oncol 27:725–731
Tomic K, Ventimiglia E, Robinson D, Haggstrom C, Lambe M, Stattin P (2018) Socioeconomic status and diagnosis, treatment, and mortality in men with prostate cancer Nationwide population-based study. Int J Cancer 142:2478–2484
Larsen SB, Brasso K, Christensen J et al (2017) Socioeconomic position and mortality among patients with prostate cancer: influence of mediating factors. Acta Oncol 56:563–568
Klein J, Knesebeck OV (2015) Socioeconomic inequalities in prostate cancer survival: a review of the evidence and explanatory factors. Soc Sci Med 142:9–18
Ministry of Health and Welfare in Taiwan. 2015 statistics of causes of death. https://www.mohw.gov.tw/dl-17928-cf97649e-1ba2-4aad-a61b-de40597df07e.html Accessed 24 Aug 2016
Health Promotion Administration, Ministry of Health and Welfare in Taiwan. Health inequalities in Taiwan. 2016. Available online: https://www.hpa.gov.tw/Pages/ashx/File.ashx?FilePath=~/File/Attach/7192/File_6518.pdf. Accessed 1 May 2016
Wu CC, Lin CH, Chiang HS, Tang MJ (2018) A population-based study of the influence of socioeconomic status on prostate cancer diagnosis in Taiwan. Int J Equity Health 17:79
Chien LH, Tseng TJ, Tsai FY et al (2018) Patterns of age-specific socioeconomic inequalities in net survival for common cancers in Taiwan, a country with universal health coverage. Cancer Epidemiol 53:42–48
Chang CM, Su YC, Lai NS et al (2012) The combined effect of individual and neighborhood socioeconomic status on cancer survival rates. PLoS ONE 7:e44325
Crawford ED (2003) Epidemiology of prostate cancer. Urology 62:3–12
Gronberg H (2003) Prostate cancer epidemiology. Lancet 361:859–864
Holford TR (1983) The estimation of age, period and cohort effects for vital rates. Biometrics 39:311–324
Clayton D, Schifflers E (1987) Models for temporal variation in cancer rates. II: age-period-cohort models. Stat Med 6:469–481
Gray PJ, Lin CC, Cooperberg MR, Jemal A, Efstathiou JA (2017) Temporal trends and the impact of race, insurance, and socioeconomic status in the management of localized prostate cancer. Eur Urol 71:729–737
Coady D, Dizioli A (2018) Income inequality and education revisited: persistence, endogeneity and heterogeneity. Appl Econ 50:2747–2761
Aiyar S, Ebeke C (2020) Inequality of opportunity, inequality of income and economic growth. World Dev 136:105115
Chmielewski AK, Reardon SF (2016) Patterns of cross-national variation in the association between income and academic achievement. Aera Open 2:2332858416649593
Deibert CM, Maliski S, Kwan L, Fink A, Connor SE, Litwin MS (2007) Prostate cancer knowledge among low income minority men. J Urol 177:1851–1855
Penson DF, Stoddard ML, Pasta DJ, Lubeck DP, Flanders SC, Litwin MS (2001) The association between socioeconomic status, health insurance coverage, and quality of life in men with prostate cancer. J Clin Epidemiol 54:350–358
Kane CJ, Lubeck DP, Knight SJ et al (2003) Impact of patient educational level on treatment for patients with prostate cancer: data from CaPSURE. Urology 62:1035–1039
Jemal A, Ward E, Wu XC, Martin HJ, McLaughlin CC, Thun MJ (2005) Geographic patterns of prostate cancer mortality and variations in access to medical care in the United States. Cancer Epidemol Biomark Prev 14:590–595
Ziehr DR, Mahal BA, Aizer AA et al (2015) Income inequality and treatment of African American men with high-risk prostate cancer. Urol Oncol 33(18):e7
Clegg LX, Reichman ME, Miller BA et al (2009) Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 20:417–435
Krupski TL, Kwan L, Afifi AA, Litwin MS (2005) Geographic and socioeconomic variation in the treatment of prostate cancer. J Clin Oncol 23:7881–7888
Directorate General of Budget, Accounting and Statistics, Excutive Yuan, R.O.C. Yearbook of Manpower Survey and Statistics, 2017. https://ebook.dgbas.gov.tw/public/Data/832918040SQKUP4R8.pdf. Accessed Mar 2018
Directorate General of Budget, Accounting and Statistics, Excutive Yuan, R.O.C. Yearbook of Manpower Survey and Statistics, 2012. https://ebook.dgbas.gov.tw/public/Data/422685146GEYI9ZG4.pdf. Accessed Mar 2013
Directorate General of Budget, Accounting and Statistics, Excutive Yuan, R.O.C. Yearbook of Earnings and Productivity Statistics, 2016. https://ebook.dgbas.gov.tw/public/Data/763151558CA7EZUC2.pdf. Accessed May 2017
Construction and Planning Agency, Ministry of the Interior R.O.C. Annual House Price Index. https://pip.moi.gov.tw/Upload/CustomFile/Doc/1070503-106Q4%E4%BD%8F%E5%AE%85%E5%83%B9%E6%A0%BC%E6%8C%87%E6%95%B8%E7%99%BC%E5%B8%83%E5%85%A7%E5%AE%B9(%E5%AE%9A%E7%A8%BF).pdf. Accessed Jan 2018
Kilpelainen TP, Talala K, Raitanen J et al (2016) Prostate cancer and socioeconomic status in the finnish randomized study of screening for prostate cancer. Am J Epidemiol 184:720–731
Islami F, Moreira DM, Boffetta P, Freedland SJ (2014) A systematic review and meta-analysis of tobacco use and prostate cancer mortality and incidence in prospective cohort studies. Eur Urol 66:1054–1064
Health Promotion Administration, Ministry of Health and Welfare. Taiwan Tobacco Control Annual Report 2015. https://www.hpa.gov.tw/file/ContentFile/201605230331066071/Taiwan_Tobacco_Control_Annual_Report_2015.pdf. Accessed 23 Aug 2016
Health Promotion Administration, Ministry of Health and Welfare. Cancer Registry Annual Report 1995. http://tcr.cph.ntu.edu.tw/uploadimages/65_Y98-Table_10.pdf. Accessed 1 Jan 2009
Health Promotion Administration, Ministry of Health and Welfare. Cancer Registry Annual Report 2013. https://www.hpa.gov.tw/Pages/ashx/File.ashx?FilePath=~/File/Attach/5191/File_6166.pdf. Accessed 1 Jan 2017
Schroder FH, Hugosson J, Roobol MJ et al (2009) Screening and prostate-cancer mortality in a randomized European study. N Engl J Med 360:1320–1328
Schroder FH, Hugosson J, Roobol MJ et al (2012) Prostate-cancer mortality at 11 years of follow-up. N Engl J Med 366:981–990
Schroder FH, Hugosson J, Roobol MJ et al (2014) Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 384:2027–2035
Moyer VA, Force USPST (2012) Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 157:120–134
Guessous I, Cullati S, Fedewa SA et al (2016) Prostate cancer screening in Switzerland: 20-year trends and socioeconomic disparities. Prev Med 82:83–91
Drazer MW, Huo D, Eggener SE (2015) National prostate cancer screening rates after the 2012 US Preventive Services Task Force recommendation discouraging prostate-specific antigen-Based screening. J Clin Oncol 33:2416–2423
Acknowledgments
This manuscript was edited by Wallace Academic Editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
SYS conceptualized the study, analyzed the data, prepared the figures and tables, and wrote paper.
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Su, SY. Geographical variations of socioeconomic status and prostate cancer mortality in Taiwan. Cancer Causes Control 32, 203–210 (2021). https://doi.org/10.1007/s10552-020-01374-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-020-01374-1