Abstract
Objective
The purpose of this study was to investigate and classify the molecular subtypes of high-grade ductal carcinoma in situ (DCIS) and identify possible high-risk subtypes. The heterogenicity of DCIS with variable clinical and histopathological presentations has been recognized. Nevertheless, only histopathological grading and diameter are currently implemented in clinical decision-making following the diagnosis of DCIS. The molecular subtypes of DCIS and their IHC surrogate markers have not been defined in conventional treatment guidelines and recommendations. We applied the definitions of molecular subtypes according to the IHC surrogate markers defined for IBC and subclassified high-grade DCIS, accordingly.
Methods
Histopathological specimens were collected, revised, and regraded from 494 patients diagnosed with DCIS between 1996 and 2018. Other in situ and papillary lesions observed in breast biopsies were excluded from this study. 357 high-grade DCIS cases were submitted to IHC analysis. The markers investigated were ER, PR, HER2, and Ki67.
Results
45 cases were classified as grade 1, 19 as grade 2, and 430 as grade 3. Sixty patients with high-grade DCIS had an additional invasive component in the surgical specimen. Thirty-three patients were diagnosed with recurrent DCIS or invasive cancer (minimum one year after their primary DCIS diagnosis). The proportions of luminal A and luminal B HER2-negative subtypes varied depending on whether 2011 or 2013 St. Gallen Consensus Conference guidelines were adopted. Luminal A was the most prevalent subtype, according to both classifications. The luminal B HER2-positive subtype was found in 22.1% of cases, HER2-enriched subtype in 21.8%, and TPN subtype in 5.6%. There were strong indications that HER2-enriched subtype was significantly more frequent among DCIS with invasive component (p = 0.0169).
Conclusions
High-grade DCIS exhibits all the molecular subtypes previously identified in IBC, but with a somewhat different distribution in our cohort. HER2-enriched subtype is substantially related to the presence of an invasive component in DCIS; consequently, it is regarded as a high-risk entity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ductal carcinoma in situ (DCIS) of the breast is a heterogeneous disease with a considerable variation in clinical presentations as well as long-term prognosis [1]. Similarly, DCIS has various histopathological presentations. In general, DCIS is defined as a neoplastic proliferation of epithelial cells in the ducts and glands of the mammary gland that do not penetrate the myoepithelium-basement membrane barrier [2]. It is unclear why some DCIS may reach 7–8 cm in size and remain in situ, whereas others become invasive carcinomas at an early stage [3]. Some studies have indicated that poorly differentiated DCIS may gradually evolve from well-differentiated DCIS through genetic defects amplified by p53 mutations [4, 5]. The cellular or nuclear atypia of DCIS varies from discrete to gross and pronounced. The risk of progression to invasive lesions varies according to atypia [6]. DCIS is still mainly treated according to the grade and extent of the lesion, and probably many of these lesions are currently overtreated [7]. The variation in demographic and geographic factors may have an impact in undertreatment of patients [8]. Quantifying the long-term benefits of treating asymptomatic DCIS that may or may not progress to invasive breast carcinoma (IBC) remains challenging. However, there is evidence that only a subfraction of DCIS develops into IBC [9]. A substantial molecular genetic analysis has established a comprehensive molecular subclassification with strong implications for the treatment of IBC which is still lacking for DCIS [10, 11]. In the routine diagnosis of IBC, surrogate markers are used by immunohistochemistry (IHC), such as estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2), and the Ki67 proliferation index, as tools to estimate the risk of micrometastasis and relapse, as well as to stratify for treatment [12]. Individual results for these markers have resulted in the development of complex treatment algorithms [13]. In contrast, all DCIS grade 3 patients are still given the same treatment, according to grade and extent, and generally do not have any additional prognostic markers [14]. Radiological microcalcifications are frequently detected [15, 16], and a large proportion of these are histologically in situ lesions (DCIS). Thus, DCIS has become a relatively common diagnosis after the introduction of screening mammography, representing up to 20 – 25% of all incident breast malignancies in industrialized countries [17]. The mammography program in Norway started in 1996, and DCIS represents approximately 20% of diagnosed premalignant and malignant incidents in the breast [18, 19]. A few studies have shown that the molecular subtypes of IBC are also present in DCIS, albeit not with the same pattern of distribution [20, 21]. Strand et al. [22] have published a molecular genetic classification based on 774 DCIS cases. IHC was not performed; thus, the correlation to the IHC surrogate markers is unknown. In line with the few studies conducted on DCIS thus far, heterogeneity of molecular subtypes has largely been found in high-grade lesions [23, 24]. Thus, our study aimed to investigate the distribution of the molecular subtypes of DCIS grade 3.
Materials and methods
Material
Our study included histopathological specimens from 494 patients diagnosed with DCIS of the breast between 1996 and 2018. Cases with a primary biopsy SNOMED code of M85002 (the diagnostic code for DCIS) were searched in the database (Doculive Patologi) of the Department of Pathology, Akershus University Hospital, Norway. We chose this code to ensure that the vast majority of biopsies had been performed because of the detection of microcalcifications on mammography that were suspicious for DCIS and not a mammographic tumor. Other in situ and papillary lesions observed in breast biopsies were excluded. We included microinvasive and small invasive lesions up to 10 mm (pT1b) [25] if the surgical specimen contained these findings. All cases with larger lesions were excluded to ensure that the indication for biopsy was microcalcification and not a radiological tumor with concurrent microcalcifications. All living patients received an information letter in which the purpose of the project was described. The text of the information letter was approved by the Regional Committee for Medical and Health Research Ethics (REK). A prepaid returning envelope was enclosed in the letters patients received, in addition to a sheet to sign and return if they objected. If they agree, they would not need to undertake any actions. We received reservations from ten patients (eight were as grade 3, one was as grade 2 and one was as grade 1); as a consequence, their cases were excluded from further examinations. The remaining 484 cases were subjected to our analysis. Materials from deceased patients could be used without any consent or information from their relatives. We are aware of the challenges regarding the grading of DCIS [7], mainly due to the different classification systems and interobserver evaluations between pathologists. Hence, two experienced breast pathologists revised and regraded all cases. If they disagreed, a third experienced breast pathologist evaluated each case. The final grade was set as simple majority. The extent of the DCIS was recorded when this information was available. In the case of multifocal lesions, separate foci were added and the total extent was noted. Any DCIS or invasive tumor in the ipsilateral or contralateral breast diagnosed at least one year after the primary DCIS diagnosis, as well as metastases and non-breast tumors discovered in the department database, were recorded.
Methods
In Norway, DCIS is graded using the Van Nuys classification [26] (Supplementary Table 1). It does not take into account growth patterns but is based on the nuclear size, which is compared to the size of RBC (≶ 2X) and the presence or absence of comedo-type necrosis (Fig. 1a–c). Given the nuclear size, this is essentially a two-tier classification. In contrast to most other grading systems for DCIS, which are three-tiered systems. The practical result was that a large majority of DCIS cases in our study were diagnosed as high-grade. Thus, this group was selected for the present study. Contrary to other studies [23], we excluded all other in situ lesions, which account for approximately 20% of the precancerous lesions in the mammary gland [27, 28]. If we had included these, the proportion of high-grade DCIS in our study would have been 72%. The molecular subtypes of DCIS and their IHC surrogate markers have not been defined in any guidelines or treatment recommendations. Thus, we implemented definitions and classifications of molecular subtypes according to the IHC surrogate markers defined for IBC at St. Gallen International Expert Consensus Conferences in 2011 and 2013 (Supplementary Table 2).
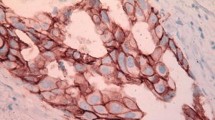
a Hematoxylin phloxine saffron (HPS) stain of DCIS grade 1, with small and monotonous epithelial nuclei. 20X magnification. b HPS stain of DCIS grade 2, small and monotonous epithelial nuclei with comedo-type necrosis. 20X magnification. c HPS staining of DCIS grade 3 enlarged and pleomorphic epithelial nuclei. 20X magnification. d IHC staining of DCIS showing strong nuclear estrogen receptor (ER) expression. 20X magnification. e IHC stain of DCIS showing strong nuclear progesterone receptor (PR) expression. 20X magnification. f IHC staining of DCIS showing strong and complete membranous expression (3+) of human epidermal growth factor receptor 2 (HER2). 20X magnification. g IHC staining of DCIS showing nuclear Ki67 expression. 20X magnification
Immunohistochemistry
IHC analysis of 357 DCIS grade 3 cases stained for ER, PR, HER2, and Ki67 were subjected to our further study. ER and PR receptor positivity was defined as ≥ 1% positive tumor cells, according to the updated guidelines of the American Society of Clinical Oncology (ASCO) and the College of American Pathologists (CAP). Ki67 IHC was evaluated by counting 200 DCIS cells (negative and positive intraductal epithelial cells) in two separate hotspot foci and the ratio was calculated. The cut-off values were reported to be 14% and 20% respectively, in compliance with recommendations from St. Gallen consensus meetings in 2011 and 2013 [29,30,31]. HER2 IHC was scored based on ASCO/CAP guidelines, as in routine diagnostic procedures [32]. HER2 silver in situ hybridization (SISH) was performed when IHC was 2 + [33]. IHC staining for ER, PR, HER2, and Ki67 was performed using a Dako Autostainer (Agilent). HER2 SISH was performed on a Roche Diagnostics BenchMark system using a fully automated Ultra-IHC/ISH staining module [34]. CC2 was used as the buffer. The details of the antibodies and HER2 SISH probes are described in Supplementary Table 3. The IHC protocol for the Dako Autostainer is shown in Supplementary Table 4. A positive control tissue was included in each run. Subtypes are described separately, according to 2011 and 2013 St. Gallen International Expert Consensus Conferences.
Statistical analysis
GraphPad Prism version 9.4 was chosen for the statistical calculations. To calculate the statistical significance, we executed different tests. The Mann–Whitney U test, a non-parametric test, was performed for independent measurements when variables between two independent groups were compared. The Kruskal–Wallis test, a non-parametric test, was chosen to compare independent measurements for variables between multiple subtypes. One-way ANOVA and parametric analysis were selected when performing normally distributed multiple comparisons and if the Shapiro–Wilk normality test was passed. Fisher's exact test was performed to calculate the p-values when comparing two proportions using a contingency table. Statistical significance was set a priori at p < 0.05.
Results
Details of the histopathological findings and grading are shown in Table 1 and include both “pure” DCIS (without an invasive component) and DCIS with an additional invasive component. We received reservations from 10 patients who were excluded from further analysis. Of the remaining 484 patients, 44 (9.0%) were grade 1, 18 (4.0%) were grade 2, and 422 (87%) were grade 3. We excluded papillary and in situ lesions of the breast. The percentage of high-grade DCIS in our study would have been 72% if we had included these. A primary discrepancy in regrading was found in 41 cases; in 58% of these cases, the final grade was DCIS grade 3 (n = 24). A report of an in situ or invasive carcinoma in the same or contralateral breast diagnosed at least one year after the primary diagnosis and treatment was found in 33 cases (6.8%). An overview of the later events is presented in Table 2. According to our local database 70 patients were registered as deceased. Only one patient was known to have passed away from metastatic IBC. We did not have access to the cause of death registry of deceased patients. The age of the patients ranged from 33 to 90 years (mean 57, and median 57). The DCIS extent ranged from 0.5 to 150 mm, (mean 28.4, and median 20). Details regarding the distribution of the extent of DCIS grade 3 and the age of the patients for each subtype are shown in Supplementary Tables 5a and 5b. Samples from 422 DCIS grade 3 were intended for IHC analysis. However, 53 cases, including 13 with an invasive component, were lost due to missing formalin-fixed paraffin-embedded (FFPE) samples in the department archive, and 12 samples lost their tissues during the IHC steps. Subsequently, 357 DCIS grade 3 cases, with all IHC markers for subtyping, were identified (Fig. 1d–g). The distribution of molecular subtypes according to the IHC surrogate markers are displayed in Tables 3 and 4 and Fig. 2a and b. Briefly, 64 patients were found to have an additional invasive carcinoma component (pT1b or less) in the surgical specimen from the same breast. 21 had an extent of ≤ 1 mm (pTmic), 27 had an extent of > 1 mm but ≤ 5 mm, (pT1a) and 16 had an extent of > 5 mm but ≤ 10 mm (pT1b). Four cases were low-grade and the remaining 60 were high-grade. Further investigations of the invasive components were not included in this study. Tables 5 and 6 demonstrate the distribution of molecular subtypes based on IHC surrogate markers for 51 cases with invasive components.
The 2011 St. Gallen conference defines (Supplementary Flowchart 1a) the subtypes as follows: luminal A is defined when ER and/or PR receptors are positive, HER2 is negative, and Ki67 < 14%. When ER and/or PR receptors are positive, HER2 is negative, and Ki67 ≥ 14%, the luminal B HER2-negative subtype is defined. Luminal B HER2 positive subtype is defined when ER, PR receptors and HER2 are positive and Ki67 is at any value. The HER2-enriched subtype is defined as having ER and PR receptors that are negative, HER2 that is positive, and Ki67 of any value. Finally, triple-negative (TPN) is defined when ER and PR receptors and HER2 are negative, and Ki67 of any value.
Following the 2013 St. Gallen conference, the subtypes are defined (Supplementary Flowchart 1b) as follows: luminal A is defined when ER receptors are positive along with positive PR expression ≥ 20%, HER2 is negative, and Ki67 < 20%. Luminal B HER2-negative is defined as ER receptors that are positive and PR expression < 20%, HER2 is negative and Ki67 expression ≥ 20%, or when ER receptors are positive and Ki67 ≥ 20 or PR expression < 20%, and HER2 is negative. Luminal B HER2 positive is defined when ER and/or PR receptors are present, as well as HER2 positivity and Ki67 at any value. HER2-enriched is defined as having ER and PR negativity, HER2 positivity, and any Ki67 value. TPN is defined when ER and PR receptors and HER2 are negative, as well as Ki67 at any value.
Depending on the implementation of recommendations from St. Gallen 2011 versus 2013 meetings, we confirmed that the distribution of luminal A and luminal B HER2-negative subtypes varied. According to 2013 St. Gallen classification the proportion of luminal A was 35.6% of cases, while it was 30.8% when following the 2011 St. Gallen guidelines. By adopting the 2011 St. Gallen recommendations, we identified that luminal B cases which made up 41.7% of the total, was constituted of 19.6% HER2-negative and 22.1% HER2-positive.
Of all cases, 27.4% belonged to the non-luminal subtypes, of which 5.6% were TPN and 21.8% were HER2-enriched. Using criteria and recommendations from 2013 St. Gallen Consensus Conference revealed that the ratios of luminal A and luminal B cases were the same, 35.6% versus 36.9%; 14.8% of those with luminal B were HER2-negative and 22.1% were HER2-positive. With the TPN subtype present in 5.6% of cases and HER2-enriched subtype in 21.8% of cases, the proportion of non-luminal cases remained unchanged.
Discussion
Our IHC results support the heterogeneity of DCIS grade 3 by demonstrating that all major molecular subtypes, as recognized for IBC, are present in DCIS grade 3. IBCs are subject to the St. Gallen classifications, yet we chose to use these to study the distributions of each individual subtype when we compared the two classifications side-by-side. These recommendations have also been described in other DCIS studies [35]. To distinguish patients with luminal A cancer from those with luminal B cancer, the 2013 St. Gallen consensus meeting introduced a 20% cut-off value for PR receptors together with an enhanced threshold for Ki67 (20%). In some studies, poor PR expression was found to be an independent prognostic and predictive factor for IBC [36]. Contrary to what ER receptors suggest, there are no promising or effective drugs that specifically target PR receptors [37, 38]. When we applied only an elevated cut-off value of 20% for PR receptors, as decided at the 2013 St. Gallen conference, the number of luminal A cases declined and the number of luminal B HER2-negative cases increased. Increasing the Ki67 threshold to 20% had an opposite effect with an elevated number of luminal B HER2-negative cases and a reduction in luminal A cases; however, when we combined these two setpoints; PR receptors at 20% and/or Ki67 at 20%, as defined by 2013 St. Gallen meeting, we observed a net gain of 17 cases in favor of luminal A subtype. When luminal A cases were added to luminal B HER2-negative cases, the total number was 180 of 357 (50.4%), regardless of St. Gallen classifications (110 + 70, St. Gallen 2011 and 127 + 53, St. Gallen 2013). The so-called "non-Ki67% sensitive" subtypes, namely luminal B HER2-positive (22.1%), HER2-enriched (21.8%), and TPN (5.6%), were unaffected. Irrespective of the Ki67 cut-off of 14% or 20%, luminal B HER2-positive and HER2-enriched subtypes constituted 157 of the 357 (44% of the total), and 27 (17.2%) of these had an additional invasive component (Tables 5 and 6).
Ki67 is considered an important prognostic proliferation marker among the luminal subtypes of IBC [39, 40]. However, agreeing on a definite cut-off for this marker has been challenging [41, 42]. There are several reasons for this, such as preanalytical and analytical assessments, interlaboratory discordance in tumor regions selected for evaluation, counting methods, and subjective assessment of staining positivity [43]. In addition, Ki67 displays a continuous distribution [44].
Our results are similar to those of a study performed by Maisonneuve et al. [45], in which the distributions of luminal A and luminal B HER2-negative cases among 9,415 patients who underwent surgery for endocrine-responsive HER2-negative breast cancer, were investigated. The relative proportions of luminal A and luminal B HER2-negative cases varied, with a net gain in favor of luminal A, when elevated setpoints for Ki67 and PR receptors were conducted. This was despite the fact that some cases had to be redefined as luminal B HER2-negative owing to a higher setpoint of the PR threshold (20%).
According to our findings, HER2-positive expression (IHC 3 + or SISH amplification) was observed in 157 samples. Of these, 79 of the 357 were luminal B HER2-positive, and 78 of the 357 were HER2-enriched, constituting 44.0% of the material. This is consistent with the findings of SA Lari et al. [46], where the mean expression rate of HER2 positivity was 40% (range, 9 – 67%). It is well known that DCIS has a higher positive expression rate of HER2 than IBC, which is approximately 15 – 20% [47,48,49]. In contrast, the frequency of TPN subtype is higher in IBC than in DCIS (approximately 10–20%), depending on ethnic background, underlined by the fact that this phenotype is more common in African-American patients than in Caucasian patients [50]. Perez et al. [51] reported 202 cases of high-grade DCIS, either “pure” or associated with IBC. They found the following distribution of subtypes among the “pure” DCIS: luminal A at 57.1%, luminal B at 11.9%, HER2-enriched at 16.7%, basal-like at 0%, and "not classified" (14.3%). They found no significant difference in immunophenotype frequencies between “pure” DCIS and DCIS associated with IBC (p > 0.05). The differences between their findings and those of our study can be explained by the role of Ki67 in defining the subtypes. Compared to our findings and as defined at the St. Gallen meeting in 2011 (Table 3), we found that the proportions of the subtypes differed between those classified as “pure” DCIS and those classified as having an additional invasive component, in which the HER2-enriched subtype was the largest among those with an invasive component (p-value = 0.0169, Fisher's exact test). Thus, the HER2 subtype had the highest risk of harboring an invasive lesion in addition to the in situ component. Thorat et al. [52] reported HER2 expression (IHC 3+) in 34.4% of DCIS cases, however they did not distinguish between cases of luminal B HER2-positive and those of “pure” HER2-enriched subtype. They did not find a significant risk of a simultaneous invasive component; however, when we combined our “pure” HER2-enriched and luminal B HER2-positive cases, we found the same result. Thorat et al. found a significantly higher risk of recurrent DCIS but not invasive lesions in this group. Thus, according to our results, a significant risk of a simultaneous invasive component is linked to the HER2-enriched subtype. Furthermore, in our study the extents of HER2-enriched and luminal B HER2-positive lesions were significantly greater than that of luminal A lesional extent (adjusted p values < 0.0001 and 0.0063, Kruskal–Wallis test). We also found that the relative proportions of luminal A cases were identical between “pure” DCIS and DCIS with an invasive component, when the St. Gallen 2011 recommendations were conducted; 30.8% and 29.5% respectively (Tables 3 and 4). In contrast, the proportions of the remaining subtypes (luminal B HER2-negative, luminal B HER2-positive, and TPN) showed a reduction.
Strengths of the study
A substantial number of DCIS samples (n = 494) from the surgical specimens and biopsies used to make the initial diagnoses were collected over a 22-year period. Qualified mammary pathologists assessed and rated all samples. Nationally standardized methods were used, and all IHC analyses were performed in a single laboratory.
Limitations of the study
The analysis of IHC samples of Ki67 is a well-known challenge, causing variations in the analysis and assessment guidelines, both within a single pathology department and among different institutions. We did not have access to clinical follow-up and cause of death registry which was a limitation of our study [53].
Conclusions
All the four main molecular subtypes recognized for IBC are also present in high-grade DCIS, resulting in a considerably heterogeneous group. Our findings suggest that the choice of the classification system can have a notable impact on the distribution of DCIS subtypes, which may have an impact on treatment options and patient outcomes. Further studies are required to identify the most precise and therapeutically beneficial system to identify high-grade DCIS subtypes. In contrast to the other subtypes, the luminal B subtypes displayed a distinguishable heterogeneity for all four surrogate IHC markers. Hence, it is crucial to devote greater focus to conducting separate studies on luminal B subtypes. Our study may contribute to a better selection of patients with high-grade DCIS in future clinical trials. There are strong indications that the HER2-enriched subtype is considered a high-risk entity among DCIS grade 3 cases, as it is significantly associated with the presence of an invasive component in our cohort (p value = 0.0169).
Data availability
The data contain sensitive patient information and is restricted by the local rules to not be distributed externally.
Abbreviations
- DCIS:
-
Ductal carcinoma in situ
- IBC:
-
Invasive breast carcinoma
- IHC:
-
Immunohistochemistry
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- HER2:
-
Human epidermal growth factor receptor 2
- Ki67:
-
Proliferation index
- SISH:
-
Silver in situ hybridization
- FFPE:
-
Formalin-fixed paraffin-embedded
- RBC:
-
Red blood cell
References
Nagasawa S, Kuze Y, Maeda I, Kojima Y, Motoyoshi A, Onishi T et al (2021) Genomic profiling reveals heterogeneous populations of ductal carcinoma in situ of the breast. Commun Biol 4(1):438
Adriance MC, Inman JL, Petersen OW, Bissell MJ (2005) Myoepithelial cells: good fences make good neighbors. Breast Cancer Res 7(5):190
Monabati A, Sokouti A-R, Noori SN, Safaei A, Talei A-R, Omidvari S et al (2015) Large palpable ductal carcinoma in situ is Her-2 positive with high nuclear grade. Int J Clin Exp Pathol 8(4):3963–3970
Allred DC, Wu Y, Mao S, Nagtegaal ID, Lee S, Perou CM et al (2008) Ductal carcinoma in situ and the emergence of diversity during breast cancer evolution. Clin Cancer Res 14(2):370–378
Lips EH, Kumar T, Megalios A, Visser LL, Sheinman M, Fortunato A et al (2022) Genomic analysis defines clonal relationships of ductal carcinoma in situ and recurrent invasive breast cancer. Nat Genet 54(6):850–860
van Seijen M, Lips EH, Thompson AM, Nik-Zainal S, Futreal A, Hwang ES et al (2019) Ductal carcinoma in situ: to treat or not to treat, that is the question. Br J Cancer 121(4):285–292
Groen EJ, Elshof LE, Visser LL, Rutgers EJT, Winter-Warnars HAO, Lips EH et al (2017) Finding the balance between over- and under-treatment of ductal carcinoma in situ (DCIS). Breast 31:274–283
Baxter NN, Virnig BA, Durham SB, Tuttle TM (2004) Trends in the treatment of ductal carcinoma in situ of the breast. J Natl Cancer Inst 96(6):443–448
Barclay J, Ernster V, Kerlikowske K, Grady D, Sickles EA (1997) Comparison of risk factors for ductal carcinoma in situ and invasive breast cancer. J Natl Cancer Inst 89(1):76–82
Eliyatkın N, Yalçın E, Zengel B, Aktaş S, Vardar E (2015) Molecular classification of breast carcinoma: from traditional, old-fashioned way to a new age, and a new way. J Breast Health 11(2):59–66
Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA et al (2000) Molecular portraits of human breast tumours. Nature 406(6797):747–752
Cho SY, Park SY, Bae YK, Kim JY, Kim EK, Kim WG et al (2021) Standardized pathology report for breast cancer. J Breast Cancer 24(1):1–21
Schneeweiss A, Bauerfeind I, Fehm T, Janni W, Thomssen C, Witzel I et al (2020) Therapy algorithms for the diagnosis and treatment of patients with early and advanced breast cancer. Breast Care (Basel) 15(6):608–618
Miligy IM, Toss MS, Khout H, Whisker L, Burrell HC, Ellis IO et al (2019) Surgical management of ductal carcinoma in situ of the breast: A large retrospective study from a single institution. Breast J 25(6):1143–1153
Wilkinson L, Thomas V, Sharma N (2017) Microcalcification on mammography: approaches to interpretation and biopsy. Br J Radiol 90(1069):20160594
Tot T, Gere M, Hofmeyer S, Bauer A, Pellas U (2021) The clinical value of detecting microcalcifications on a mammogram. Semin Cancer Biol 72:165–174
Ponti A, Lynge E, James T, Májek O, von Euler-Chelpin M, Anttila A et al (2014) International variation in management of screen-detected ductal carcinoma in situ of the breast. Eur J Cancer (Oxf, Engl, 1990) 50(15):2695–704
Lynge E, Ponti A, James T, Májek O, von Euler-Chelpin M, Anttila A et al (2014) Variation in detection of ductal carcinoma in situ during screening mammography: a survey within the International Cancer Screening Network. Eur J Cancer (Oxf, Engl, 1990) 50(1):185–92
Elin Wølner Bjørnson ÅSH, Sagstad S, Larsen M, Thy J, Mangerud G, Kathrin A, Ertzaas SH (2022) BreastScreen Norway: 25 years of organized screening. Cancer Registry of Norway, Oslo
Vincent-Salomon A, Lucchesi C, Gruel N, Raynal V, Pierron G, Goudefroye R et al (2008) Integrated genomic and transcriptomic analysis of ductal carcinoma in situ of the breast. Clin Cancer Res 14(7):1956–65
Meijnen P, Peterse JL, Antonini N, Rutgers EJ, van de Vijver MJ (2008) Immunohistochemical categorisation of ductal carcinoma in situ of the breast. Br J Cancer 98(1):137–142
Strand SH, Rivero-Gutiérrez B, Houlahan KE, Seoane JA, King LM, Risom T et al (2022) Molecular classification and biomarkers of clinical outcome in breast ductal carcinoma in situ: analysis of TBCRC 038 and RAHBT cohorts. Cancer Cell 40(12):1521–36.e7
Clark SE, Warwick J, Carpenter R, Bowen RL, Duffy SW, Jones JL (2011) Molecular subtyping of DCIS: heterogeneity of breast cancer reflected in pre-invasive disease. Br J Cancer 104(1):120–127
Sinha VC, Piwnica-Worms H (2018) Intratumoral heterogeneity in ductal carcinoma in situ: chaos and consequence. J Mammary Gland Biol Neoplasia 23(4):191–205
Cserni G, Chmielik E, Cserni B, Tot T (2018) The new TNM-based staging of breast cancer. Virch Arch 472(5):697–703
Silverstein MJ, Poller DN, Waisman JR, Colburn WJ, Barth A, Gierson ED et al (1995) Prognostic classification of breast ductal carcinoma-in-situ. Lancet 345(8958):1154–1157
Siziopikou KP (2013) Ductal carcinoma in situ of the breast: current concepts and future directions. Arch Pathol Lab Med 137(4):462–466
Lee RJ, Vallow LA, McLaughlin SA, Tzou KS, Hines SL, Peterson JL (2012) Ductal carcinoma in situ of the breast. Int J Surg Oncol 2012:123549
Brouckaert O, Laenen A, Vanderhaegen J, Wildiers H, Leunen K, Amant F et al (2012) Applying the 2011 St Gallen panel of prognostic markers on a large single hospital cohort of consecutively treated primary operable breast cancers. Ann Oncol 23(10):2578–2584
Harbeck N, Thomssen C, Gnant M (2013) St. Gallen 2013: brief preliminary summary of the consensus discussion. Breast Care (Basel) 8(2):102–109
Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B et al (2013) Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol 24(9):2206–2223
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS et al (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J Clin Oncol 36(20):2105–2122
Papouchado BG, Myles J, Lloyd RV, Stoler M, Oliveira AM, Downs-Kelly E et al (2010) Silver in situ hybridization (SISH) for determination of HER2 gene status in breast carcinoma: comparison with FISH and assessment of interobserver reproducibility. Am J Surg Pathol 34(6):767–776
RDO (ed) (2020) VENTANA HER2 Dual ISH DNA Probe Cocktail. FDA, Silver Spring. https://diagnostics.roche.com/content/dam/diagnostics/us/en/LandingPages/her2-dual-ish/VENTANA-HER2-Dual-ISH-Method-Sheet.pdf
Zhou W, Jirström K, Amini R-M, Fjällskog M-L, Sollie T, Lindman H et al (2013) Molecular subtypes in ductal carcinoma in situ of the breast and their relation to prognosis: a population-based cohort study. BMC Cancer 13(1):512
Cao SS, Lu CT (2016) Recent perspectives of breast cancer prognosis and predictive factors. Oncol Lett 12(5):3674–3678
Ono M, Tsuda H, Yoshida M, Shimizu C, Kinoshita T, Tamura K (2017) Prognostic significance of progesterone receptor expression in estrogen-receptor positive, HER2-negative, node-negative invasive breast cancer with a low Ki-67 labeling index. Clin Breast Cancer 17(1):41–47
Brisken C, Hess K, Jeitziner R (2015) Progesterone and overlooked endocrine pathways in breast cancer pathogenesis. Endocrinology 156(10):3442–3450
de Azambuja E, Cardoso F, de Castro G Jr, Colozza M, Mano MS, Durbecq V et al (2007) Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br J Cancer 96(10):1504–1513
Criscitiello C, Disalvatore D, De Laurentiis M, Gelao L, Fumagalli L, Locatelli M et al (2014) High Ki-67 score is indicative of a greater benefit from adjuvant chemotherapy when added to endocrine therapy in luminal B HER2 negative and node-positive breast cancer. Breast 23(1):69–75
Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M et al (2015) Tailoring therapies–improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol 26(8):1533–1546
Lombardi A, Lazzeroni R, Bersigotti L, Vitale V, Amanti C (2021) The proper Ki-67 cut-off in hormone responsive breast cancer: a monoinstitutional analysis with long-term follow-up. Breast Cancer (Dove Med Press) 13:213–217
Polley MY, Leung SC, McShane LM, Gao D, Hugh JC, Mastropasqua MG et al (2013) An international Ki67 reproducibility study. J Natl Cancer Inst 105(24):1897–1906
Sood N (2019) Ki-67, an elusive marker in the prognosis of breast cancer. Indian J Med Res 150(3):214–216
Maisonneuve P, Disalvatore D, Rotmensz N, Curigliano G, Colleoni M, Dellapasqua S et al (2014) Proposed new clinicopathological surrogate definitions of luminal A and luminal B (HER2-negative) intrinsic breast cancer subtypes. Breast Cancer Res (BCR) 16(3):R65
Lari SA, Kuerer HM (2011) Biological markers in DCIS and risk of breast recurrence: a systematic review. J Cancer 2:232–261
Miligy IM, Toss MS, Gorringe KL, Lee AHS, Ellis IO, Green AR et al (2019) The clinical and biological significance of HER2 over-expression in breast ductal carcinoma in situ: a large study from a single institution. Br J Cancer 120(11):1075–1082
Stark AT, Claud S, Kapke A, Lu M, Linden M, Griggs J (2005) Race modifies the association between breast carcinoma pathologic prognostic indicators and the positive status for HER-2/neu. Cancer 104(10):2189–2196
Huang HJ, Neven P, Drijkoningen M, Paridaens R, Wildiers H, Van Limbergen E et al (2005) Hormone receptors do not predict the HER2/neu status in all age groups of women with an operable breast cancer. Ann Oncol 16(11):1755–1761
Morris GJ, Naidu S, Topham AK, Guiles F, Xu Y, McCue P et al (2007) Differences in breast carcinoma characteristics in newly diagnosed African-American and Caucasian patients. Cancer 110(4):876–884
Perez AA, Rocha RM, Balabram D, Souza Áda S, Gobbi H (2013) Immunohistochemical profile of high-grade ductal carcinoma in situ of the breast. Clinics (Sao Paulo) 68(5):674–678
Thorat MA, Levey PM, Jones JL, Pinder SE, Bundred NJ, Fentiman IS et al (2021) Prognostic and predictive value of HER2 expression in ductal carcinoma in situ: results from the UK/ANZ DCIS randomized trial. Clin Cancer Res 27(19):5317–5324
Focke CM, Bürger H, van Diest PJ, Finsterbusch K, Gläser D, Korsching E et al (2017) Interlaboratory variability of Ki67 staining in breast cancer. Eur J Cancer (Oxf, Engl) 84:219–227
Silverstein MJ, Lagios MD, Craig PH, Waisman JR, Lewinsky BS, Colburn WJ et al (1996) A prognostic index for ductal carcinoma in situ of the breast. Cancer 77(11):2267–2274
Funding
Open access funding provided by Akershus University Hospital (AHUS). We are thankful for the general research funding provided by the University of Oslo (J.G.). Open access funding was provided by Akershus University Hospital (AHUS), Norway.
Author information
Authors and Affiliations
Contributions
All authors contributed to the content of this manuscript. Material preparation, data collection and analysis were performed by TS, and HS. The initial draft of the manuscript was written by HS. YLK contributed to the IHC analysis. ML and IST contributed to the primary analysis of the histopathological specimens and classification of DCIS. TS, DP, and HS regraded the DCIS when required. HS, DP, JG, and TS edited the manuscript and approved its final version. TS was responsible for handling the database used in this study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This was a retrospective study, and the use of data and histological material was approved by the Regional Committees for Medical and Health Research Ethics (REK), case Nos. 29299 and 307976.
Consent to participate
All analyses were performed on historical or archived material from female patients who had not been under treatment for at least 3 years. We received reservations from 10 patients, who were excluded from further analysis. Information letters to relatives of the deceased patients were not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schandiz, H., Park, D., Kaiser, Y.L. et al. Subtypes of high-grade breast ductal carcinoma in situ (DCIS): incidence and potential clinical impact. Breast Cancer Res Treat 201, 329–338 (2023). https://doi.org/10.1007/s10549-023-07016-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07016-9