Abstract
Purpose
To assess associations between adherence to and persistence with adjuvant hormone therapy and mortality among older women with breast cancer.
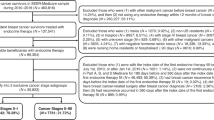
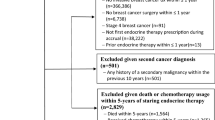
Methods
The surveillance, epidemiology, and end results data linked with U.S. Medicare claims was used. This study included older women diagnosed with stage I–III hormone receptor-positive breast cancer from 2009 through 2017. Adherence was defined as having proportion of days covered (PDC) ≥ 0.80. Persistence was defined as having no discontinuation, i.e., no break of ≥ 180 continuous days. Length of persistence was calculated as time from therapy initiation to discontinuation. Cox models with time-dependent covariates were used to assess associations between adherence and persistence with mortality.
Results
This study included 25,796 women. Adherence rates were 78.1 percent, 75.2 percent, 72.4 percent, 70.0 percent, and 61.5 percent from year 1 to year 5 after hormone therapy initiation. Persistence rates were 87.5 percent, 81.7 percent, 77.1 percent, 72.9 percent, and 68.9 percent through cumulative intervals of 1 year up to 5 years. Adherence was associated with all-cause mortality but not associated with breast cancer-specific mortality. Persistent women had lower risk of all-cause mortality and breast cancer-specific mortality. Each additional year of persistence had additional contributions to survival benefits (11% decreased risk of all-cause mortality and 37% decreased risk of breast cancer-specific mortality).
Conclusion
This study confirms the detrimental effect of nonadherence to adjuvant hormone therapy across up to 5 years on all-cause survival in older U.S. women. It also reveals the survival benefits associated with having longer persistence across up to 5 years.
Similar content being viewed by others
Data availability
The data that support the findings of this study came from the SEER-Medicare data. Restrictions apply to the availability of these data, which were used under a data use agreement with the National Cancer Institute. The public may obtain data from the National Cancer Institute through individual data use agreements.
References
U.S. Cancer Statistics Working Group (2022) U.S. Cancer statistics data visualizations tool, based on 2021 submission data (1999–2019). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. https://www.cdc.gov/cancer/breast/statistics/index.htm. Accessed 13 Sept 2022
Early Breast Cancer Trialists’ Collaborative Group (2011) Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet (London, England) 378(9793):771–784
Early Breast Cancer Trialists’ Collaborative Group (2015) Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet (London, England) 386(10001):1341–1352
Burstein HJ, Lacchetti C, Anderson H, Buchholz TA, Davidson NE, Gelmon KA, Giordano SH, Hudis CA, Solky AJ, Stearns V, Winer EP, Griggs JJ (2019) Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol 37(5):423–438
National Comprehensive Cancer Network (2021) NCCN clinical practice guidelines in oncology. Breast Cancer. Version 5.2021. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 1 Jul 2021
Murphy CC, Bartholomew LK, Carpentier MY, Bluethmann SM, Vernon SW (2012) Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat 134(2):459–478
McCowan C, Shearer J, Donnan PT, Dewar JA, Crilly M, Thompson AM, Fahey TP (2008) Cohort study examining tamoxifen adherence and its relationship to mortality in women with breast cancer. Br J Cancer 99(11):1763–1768
Hershman DL, Shao T, Kushi LH, Buono D, Tsai WY, Fehrenbacher L, Kwan M, Gomez SL, Neugut AI (2011) Early discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer. Breast Cancer Res Treat 126(2):529–537
Makubate B, Donnan PT, Dewar JA, Thompson AM, McCowan C (2013) Cohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortality. Br J Cancer 108(7):1515–1524
Hsieh KP, Chen LC, Cheung KL, Chang CS, Yang YH (2014) Interruption and non-adherence to long-term adjuvant hormone therapy is associated with adverse survival outcome of breast cancer women–an Asian population-based study. PLoS ONE 9(2):e87027
Winn AN, Dusetzina SB (2016) The association between trajectories of endocrine therapy adherence and mortality among women with breast cancer. Pharmacoepidemiol Drug Saf 25(8):953–959
Font R, Espinas JA, Barnadas A, Izquierdo A, Galceran J, Saladie F, Marcos-Gragera R, Torrent A, Manchon-Walsh P, Borras JM (2019) Influence of adherence to adjuvant endocrine therapy on disease-free and overall survival: a population-based study in Catalonia. Spain Breast Cancer Res Treat 175(3):733–740
Tan X, Marshall VD, Anderson RT, Donohoe J, Camacho F, Balkrishnan R (2015) Adjuvant therapy use among Appalachian breast cancer survivors. Medicine 94(26):e1071
Dignam JJ, Huang L, Ries L, Reichman M, Mariotto A, Feuer E (2009) Estimating breast cancer-specific and other-cause mortality in clinical trial and population-based cancer registry cohorts. Cancer 115(22):5272–5283
de Brito C, Portela MC, de Vasconcellos MTL (2016) Health care factors associated with survival among women with breast cancer on hormone therapy in Rio de Janeiro, Brazil, 2004–2010. Pan Am J Public Health 39(6):358–365
Seneviratne S, Campbell I, Scott N, Kuper-Hommel M, Kim B, Pillai A, Lawrenson R (2015) Adherence to adjuvant endocrine therapy: is it a factor for ethnic differences in breast cancer outcomes in New Zealand? Breast (Edinburgh, Scotland) 24(1):62–67
Nau DP (2012) Proportion of days covered (PDC) as a preferred method of measuring medication adherence. http://ep.yimg.com/ty/cdn/epill/pdcmpr.pdf. Accessed 18 Jun 2021
Farias AJ, Du XL (2017) Racial differences in adjuvant endocrine therapy use and discontinuation in association with mortality among Medicare breast cancer patients by receptor status. Cancer Epidemiol Biomarkers Prev 26(8):1266–1275
National Cancer Institute (2021) Surveillance, epidemiology, and end results (SEER) program overview. https://seer.cancer.gov/about/factsheets/SEER_Overview.pdf. Accessed 03 Nov 2021
Centers for Medicare & Medicaid Services (2020) Medicare 2021 part C & D star ratings technical notes. https://www.cms.gov/files/document/2021technotes20201001.pdf-0. Accessed 10 Feb 2022
Chubak J, Yu O, Pocobelli G, Lamerato L, Webster J, Prout MN, Ulcickas Yood M, Barlow WE, Buist DSM (2012) Administrative data algorithms to identify second breast cancer events following early-stage invasive breast cancer. J Natl Cancer Inst 104(12):931–940
He W, Fang F, Varnum C, Eriksson M, Hall P, Czene K (2015) Predictors of discontinuation of adjuvant hormone therapy in patients with breast cancer. J Clin Oncol 33(20):2262–2269
Lambert-Côté L, Bouhnik A-D, Bendiane M-K, Bérenger C, Mondor M, Huiart L, Lauzier S (2020) Adherence trajectories of adjuvant endocrine therapy in the 5 years after its initiation among women with non-metastatic breast cancer: a cohort study using administrative databases. Breast Cancer Res Treat 180(3):777–790
Wu J, Lu ZK (2013) Hormone therapy adherence and costs in women with breast cancer. Am J Pharm Benefits 5(2):65–70
Weaver KE, Camacho F, Hwang W, Anderson R, Kimmick G (2013) Adherence to adjuvant hormonal therapy and its relationship to breast cancer recurrence and survival among low-income women. Am J Clin Oncol 36(2):181–187
Farias AJ, Du XL (2016) Association between out-of-pocket costs, race/ethnicity, and adjuvant endocrine therapy adherence among Medicare patients with breast cancer. J Clin Oncol 35(1):86–95
Yanez B, Gray RJ, Sparano JA, Carlos RC, Sadigh G, Garcia SF, Gareen IF, Whelan TJ, Sledge GW, Cella D, Wagner LI (2021) Association of modifiable risk factors with early discontinuation of adjuvant endocrine therapy: A post hoc analysis of a randomized clinical trial. JAMA Oncol 7(8):1–7
Lee HS, Lee JY, Ah YM, Kim HS, Im SA, Noh DY, Lee BK (2014) Low adherence to upfront and extended adjuvant letrozole therapy among early breast cancer patients in a clinical practice setting. Oncology 86(5–6):340–349
Bosco-Lévy P, Jové J, Robinson P, Moore N, Fourrier-Réglat A, Bezin J (2016) Persistence to 5 year hormonal breast cancer therapy: a French national population-based study. Br J Cancer 115(8):912–919
Duan W, Li S, Meng X, Sun Y, Jia C (2017) Smoking and survival of breast cancer patients: a meta-analysis of cohort studies. The Breast 33:117–124
Sella T, Chodick G (2020) Adherence and persistence to adjuvant hormonal therapy in early-stage breast cancer patients: a population-based retrospective cohort study in Israel. Breast Care (Basel) 15(1):45–53
Nelson SH, Marinac CR, Patterson RE, Nechuta SJ, Flatt SW, Caan BJ, Kwan ML, Poole EM, Chen WY, Shu XO, Pierce JP (2016) Impact of very low physical activity, BMI, and comorbidities on mortality among breast cancer survivors. Breast Cancer Res Treat 155(3):551–557
Hagen KB, Aas T, Kvaløy JT, Søiland H, Lind R (2019) Adherence to adjuvant endocrine therapy in postmenopausal breast cancer patients: a 5 year prospective study. The Breast 44:52–58
Wuensch P, Hahne A, Haidinger R, Meißler K, Tenter B, Stoll C, Senf B, Huebner J (2015) Discontinuation and non-adherence to endocrine therapy in breast cancer patients: is lack of communication the decisive factor? J Cancer Res Clin Oncol 141(1):55–60
Jacob Arriola KR, Mason TA, Bannon KA, Holmes C, Powell CL, Horne K, O’Regan R (2014) Modifiable risk factors for adherence to adjuvant endocrine therapy among breast cancer patients. Patient Educ Couns 95(1):98–103
National Cancer Institute (2022) SEER-Medicare linked data resource. Measures that are limited or not available in the data. https://healthcaredelivery.cancer.gov/seermedicare/considerations/measures.html. Accessed 6 Apr 2023
Warren JL, Mariotto A, Melbert D, Schrag D, Doria-Rose P, Penson D, Yabroff KR (2016) Sensitivity of Medicare claims to identify cancer recurrence in elderly colorectal and breast cancer patients. Med Care 54(8):e47-54
Pazzagli L, Linder M, Zhang M, Vago E, Stang P, Myers D, Andersen M, Bahmanyar S (2018) Methods for time-varying exposure related problems in pharmacoepidemiology: an overview. Pharmacoepidemiol Drug Saf 27(2):148–160
van Walraven C, Davis D, Forster AJ, Wells GA (2004) Time-dependent bias was common in survival analyses published in leading clinical journals. J Clin Epidemiol 57(7):672–682
Acknowledgements
This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; Information Management Services (IMS), Inc.; and the surveillance, epidemiology, and end results (SEER) Program tumor registries in the creation of the SEER-Medicare database. The collection of cancer incidence data used in this study was supported by the California Department of Public Health pursuant to California Health and Safety Code Section 103885; Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries, under cooperative agreement 1NU58DP007156; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201800032I awarded to the University of California, San Francisco, contract HHSN261201800015I awarded to the University of Southern California, and contract HHSN261201800009I awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the author(s) and do not necessarily reflect the opinions of the State of California, Department of Public Health, the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors.
Funding
This work was supported in part by a grant from the Lilly Endowment, Inc., to the Purdue University College of Pharmacy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by Purdue University’s Institutional Review Board as exempt.
Informed consent
This study was approved by Purdue University’s Institutional Review Board as exempt, waiving participant written informed consent for limited data set.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, D., Thomas, J. Survival benefits associated with being adherent and having longer persistence to adjuvant hormone therapy across up to five years among U.S. Medicare population with breast cancer. Breast Cancer Res Treat 201, 89–104 (2023). https://doi.org/10.1007/s10549-023-06992-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06992-2