Abstract
Purpose
With an increasing emphasis on patient-centered care, clinicians in subspecialties such as breast surgery and radiation oncology that offer multiple therapeutic options with equivalent outcomes are under increasing pressure to aid patients with the decision-making process. The aim of this review is to summarize existing studies that either evaluated factors in patient’s decision-making regarding locoregional therapy in early-stage breast cancer or evaluated benefit thresholds required to change therapy decisions.
Methods
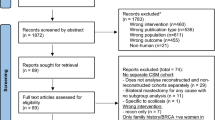
A PubMed search to identify prospective or retrospective studies written in English reporting factors in patient decision-making regarding locoregional therapy in early-stage breast cancer was conducted. No restriction was placed on publication date. Studies that focused on breast reconstruction decisions or on patient preferences for decision-making involvement were excluded.
Results
A total of 39 studies were identified; 19 examining patient preferences for breast-conserving surgery versus mastectomy, 7 on preferences for contralateral prophylactic mastectomy, 2 on non-surgical options, 2 on the extent of axillary surgery, and 9 on radiation therapy decisions. Themes such as fear of recurrence, desire to avoid additional invasive therapy, and the importance of physician preference were common, but many studies also highlighted factors important to specific subpopulations of women.
Conclusions
Patient preference is difficult to define and measure, and heterogeneity across studies renders direct comparison difficult. Future work is needed to define women’s risk-thresholds for certain treatments, delve into the psychological factors that direct their decisions, and understand how patients’ valuations of risk interact with society’s.
Similar content being viewed by others
References
Sepucha K, Mulley AG Jr (2009) A perspective on the patient's role in treatment decisions. Med Care Res Rev 66(1 Suppl):53s–74s. https://doi.org/10.1177/1077558708325511
Braddock CH 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W (1999) Informed decision making in outpatient practice: time to get back to basics. JAMA 282(24):2313–2320. https://doi.org/10.1001/jama.282.24.2313
Lee CN, Chang Y, Adimorah N, Belkora JK, Moy B, Partridge AH, Ollila DW, Sepucha KR (2012) Decision making about surgery for early-stage breast cancer. J Am Coll Surg 214(1):1–10. https://doi.org/10.1016/j.jamcollsurg.2011.09.017
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347(16):1233–1241. https://doi.org/10.1056/NEJMoa022152
Neuman HSJ, Hanlon B et al (2018) Local recurrence rates after breast-conserving therapy in patients receiving modern era therapy. American Society of Breast Surgeons Annual Meeting. 2018: Abstract 403956. Presented May 4, 2018
Darby S, McGale P, Correa C, Taylor C, Arriagada R, Clarke M, Cutter D, Davies C, Ewertz M, Godwin J, Gray R, Pierce L, Whelan T, Wang Y, Peto R (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378(9804):1707–1716. https://doi.org/10.1016/s0140-6736(11)61629-2
Mannino M, Yarnold JR (2009) Local relapse rates are falling after breast conserving surgery and systemic therapy for early breast cancer: can radiotherapy ever be safely withheld? Radiother Oncol 90(1):14–22. https://doi.org/10.1016/j.radonc.2008.05.002
Kiess AP, McArthur HL, Mahoney K, Patil S, Morris PG, Ho A, Hudis CA, McCormick B (2012) Adjuvant trastuzumab reduces locoregional recurrence in women who receive breast-conservation therapy for lymph node-negative, human epidermal growth factor receptor 2-positive breast cancer. Cancer 118(8):1982–1988. https://doi.org/10.1002/cncr.26484
Lanning RM, Morrow M, Riaz N, McArthur HL, Dang C, Moo TA, El-Tamer M, Krause K, Siu C, Hsu M, Zhang Z, Pei X, McCormick B, Powell SN, Ho A (2015) The effect of adjuvant trastuzumab on locoregional recurrence of human epidermal growth factor receptor 2-positive breast cancer treated with mastectomy. Ann Surg Oncol 22(8):2517–2525. https://doi.org/10.1245/s10434-014-4321-2
Voogd AC, van Oost FJ, Rutgers EJ, Elkhuizen PH, van Geel AN, Scheijmans LJ, van der Sangen MJ, Botke G, Hoekstra CJ, Jobsen JJ, van de Velde CJ, von Meyenfeldt MF, Tabak JM, Peterse JL, van de Vijver MJ, Coebergh JW, van Tienhoven G (2005) Long-term prognosis of patients with local recurrence after conservative surgery and radiotherapy for early breast cancer. Eur J Cancer 41(17):2637–2644. https://doi.org/10.1016/j.ejca.2005.04.040
Killoran M, Moyer A (2006) Surgical treatment preferences in Chinese-American women with early-stage breast cancer. Psychooncology 15(11):969–984. https://doi.org/10.1002/pon.1032
Benedict S, Cole DJ, Baron L, Baron P (2001) Factors influencing choice between mastectomy and lumpectomy for women in the Carolinas. J Surg Oncol 76(1):6–12. https://doi.org/10.1002/1096-9098(200101)76:1<6:aid-jso1002>3.0.co;2-f
Agrawal S, Goel AK, Lal P (2012) Participation in decision making regarding type of surgery and treatment-related satisfaction in North Indian women with early breast cancer. J Cancer Res Ther 8(2):222–225. https://doi.org/10.4103/0973-1482.98974
Dicks E, Roome R, Chafe J, Powell E, McCrate F, Simmonds C, Etchegary H (2019) Factors influencing surgical treatment decisions for breast cancer: a qualitative exploration of surgeon and patient perspectives. Curr Oncol 26(2):e216–e225. https://doi.org/10.3747/co.26.4305
Gollop SJ, Kyle SM, Fancourt MW, Gilkison WT, Mosquera DA (2009) Why Taranaki women choose to have a mastectomy when suitable for breast conservation treatment. ANZ J Surg 79(9):604–609. https://doi.org/10.1111/j.1445-2197.2009.05014.x
Katz SJ, Lantz PM, Zemencuk JK (2001) Correlates of surgical treatment type for women with noninvasive and invasive breast cancer. J Womens Health Gend Based Med 10(7):659–670. https://doi.org/10.1089/15246090152563533
Greenup RA, Rushing C, Fish L, Campbell BM, Tolnitch L, Hyslop T, Peppercorn J, Wheeler SB, Zafar SY, Myers ER, Hwang ES (2019) Financial Costs and Burden Related to Decisions for Breast Cancer Surgery. J Oncol Pract 15(8):e666–e676. https://doi.org/10.1200/jop.18.00796
Fayanju OM, Stoll CR, Fowler S, Colditz GA, Margenthaler JA (2014) Contralateral prophylactic mastectomy after unilateral breast cancer: a systematic review and meta-analysis. Ann Surg 260(6):1000–1010. https://doi.org/10.1097/sla.0000000000000769
Lostumbo L, Carbine NE, Wallace J (2010) Prophylactic mastectomy for the prevention of breast cancer. Cochrane Database Syst Rev 11:CD002748. https://doi.org/10.1002/14651858.CD002748.pub3
De Abreu LR, Haas M, Hall J, Parish K, Stuart D, Viney R (2019) My mind is made up: cancer concern and women's preferences for contralateral prophylactic mastectomy. Eur J Cancer Care (Engl) 28(4):e13058. https://doi.org/10.1111/ecc.13058
Rosenberg SM, Tracy MS, Meyer ME, Sepucha K, Gelber S, Hirshfield-Bartek J, Troyan S, Morrow M, Schapira L, Come SE, Winer EP, Partridge AH (2013) Perceptions, knowledge, and satisfaction with contralateral prophylactic mastectomy among young women with breast cancer: a cross-sectional survey. Ann Intern Med 159(6):373–381. https://doi.org/10.7326/0003-4819-159-6-201309170-00003
Hawley ST, Griffith KA, Hamilton AS, Ward KC, Morrow M, Janz NK, Katz SJ, Jagsi R (2017) The association between patient attitudes and values and the strength of consideration for contralateral prophylactic mastectomy in a population-based sample of breast cancer patients. Cancer 123(23):4547–4555. https://doi.org/10.1002/cncr.30924
Tesson S, Richards I, Porter D, Phillips KA, Rankin N, Costa D, Musiello T, Marven M, Butow P (2017) Women's preferences for contralateral prophylactic mastectomy following unilateral breast cancer: what risk-reduction makes it worthwhile? Breast 31:233–240. https://doi.org/10.1016/j.breast.2016.11.025
Huang J, Chagpar A (2019) Factors associated with decision to undergo contralateral prophylactic mastectomy versus unilateral mastectomy. Am J Surg 218(1):170–174. https://doi.org/10.1016/j.amjsurg.2018.11.040
Katz SJ, Janz NK, Abrahamse P, Wallner LP, Hawley ST, An LC, Ward KC, Hamilton AS, Morrow M, Jagsi R (2017) Patient reactions to surgeon recommendations about contralateral prophylactic mastectomy for treatment of breast cancer. JAMA Surg 152(7):658–664. https://doi.org/10.1001/jamasurg.2017.0458
Hind D, Wyld L, Beverley CB, Reed MW (2006) Surgery versus primary endocrine therapy for operable primary breast cancer in elderly women (70 years plus). Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004272.pub2
Husain LS, Collins K, Reed M, Wyld L (2008) Choices in cancer treatment: a qualitative study of the older women's (> 70 years) perspective. Psychooncology 17(4):410–416. https://doi.org/10.1002/pon.1242
Wyld L, Garg DK, Kumar ID, Brown H, Reed MW (2004) Stage and treatment variation with age in postmenopausal women with breast cancer: compliance with guidelines. Br J Cancer 90(8):1486–1491. https://doi.org/10.1038/sj.bjc.6601742
Lavelle K, Sowerbutts AM, Bundred N, Pilling M, Degner L, Stockton C, Todd C (2014) Is lack of surgery for older breast cancer patients in the UK explained by patient choice or poor health? A prospective cohort study. Br J Cancer 110(3):573–583. https://doi.org/10.1038/bjc.2013.734
Schonberg MA, Marcantonio ER, Li D, Silliman RA, Ngo L, McCarthy EP (2010) Breast cancer among the oldest old: tumor characteristics, treatment choices, and survival. J Clin Oncol 28(12):2038–2045. https://doi.org/10.1200/jco.2009.25.9796
Asaad M, Tamer M, Mokbel K (2003) British women's choice between sentinel node biopsy and axillary node clearance for breast cancer. Curr Med Res Opin 19(6):570–574. https://doi.org/10.1185/030079903125002199
Lucci A, McCall LM, Beitsch PD, Whitworth PW, Reintgen DS, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Giuliano AE (2007) Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol 25(24):3657–3663. https://doi.org/10.1200/jco.2006.07.4062
Veronesi U, Viale G, Paganelli G, Zurrida S, Luini A, Galimberti V, Veronesi P, Intra M, Maisonneuve P, Zucca F, Gatti G, Mazzarol G, De Cicco C, Vezzoli D (2010) Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann Surg 251(4):595–600. https://doi.org/10.1097/SLA.0b013e3181c0e92a
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Ashikaga T, Weaver DL, Miller BJ, Jalovec LM, Frazier TG, Noyes RD, Robidoux A, Scarth HM, Mammolito DM, McCready DR, Mamounas EP, Costantino JP, Wolmark N (2007) Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III trial. Lancet Oncol 8(10):881–888. https://doi.org/10.1016/s1470-2045(07)70278-4
Galimberti V, Cole BF, Viale G, Veronesi P, Vicini E, Intra M, Mazzarol G, Massarut S, Zgajnar J, Taffurelli M, Littlejohn D, Knauer M, Tondini C, Di Leo A, Colleoni M, Regan MM, Coates AS, Gelber RD, Goldhirsch A (2018) Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23–01): 10-year follow-up of a randomised, controlled phase 3 trial. Lancet Oncol 19(10):1385–1393. https://doi.org/10.1016/S1470-2045(18)30380-2
Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, Cataliotti L, Westenberg AH, Klinkenbijl JH, Orzalesi L, Bouma WH, van der Mijle HC, Nieuwenhuijzen GA, Veltkamp SC, Slaets L, Duez NJ, de Graaf PW, van Dalen T, Marinelli A, Rijna H, Snoj M, Bundred NJ, Merkus JW, Belkacemi Y, Petignat P, Schinagl DA, Coens C, Messina CG, Bogaerts J, Rutgers EJ (2014) Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981–22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol 15(12):1303–1310. https://doi.org/10.1016/s1470-2045(14)70460-7
Miller CL, Specht MC, Skolny MN, Horick N, Jammallo LS, O'Toole J, Shenouda MN, Sadek BT, Smith BL, Taghian AG (2014) Risk of lymphedema after mastectomy: potential benefit of applying ACOSOG Z0011 protocol to mastectomy patients. Breast Cancer Res Treat 144(1):71–77. https://doi.org/10.1007/s10549-014-2856-3
Leidenius MH, Smitten KAV, Hietanen PS (2002) Patient preference for dissection of sentinel nodes outside Level I-II of the Axilla. Acta Oncol 41(7–8):652–658. https://doi.org/10.1080/028418602321028274
Rosenberger LH, Thomas SM, Plichta JK, Fayanju OM, Hyslop T, Greenup RA, Hwang ES (2019) Decreasing rates of axillary lymph node dissections over time: Implications for surgical resident exposure and operative skills development. Am J Surg 218(4):786–791. https://doi.org/10.1016/j.amjsurg.2019.07.013
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, Ollila DW, Hansen NM, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Morrow M (2017) Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA 318(10):918–926. https://doi.org/10.1001/jama.2017.11470
Hughes KS, Schnaper LA, Bellon JR, Cirrincione CT, Berry DA, McCormick B, Muss HB, Smith BL, Hudis CA, Winer EP, Wood WC (2013) Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J Clin Oncol 31(19):2382–2387. https://doi.org/10.1200/jco.2012.45.2615
Martelli G, Boracchi P, Ardoino I, Lozza L, Bohm S, Vetrella G, Agresti R (2012) Axillary dissection versus no axillary dissection in older patients with T1N0 breast cancer: 15-year results of a randomized controlled trial. Ann Surg 256(6):920–924. https://doi.org/10.1097/SLA.0b013e31827660a8
Rudenstam CM, Zahrieh D, Forbes JF, Crivellari D, Holmberg SB, Rey P, Dent D, Campbell I, Bernhard J, Price KN, Castiglione-Gertsch M, Goldhirsch A, Gelber RD, Coates AS (2006) Randomized trial comparing axillary clearance versus no axillary clearance in older patients with breast cancer: first results of International Breast Cancer Study Group Trial 10–93. J Clin Oncol 24(3):337–344. https://doi.org/10.1200/jco.2005.01.5784
Hayman JA, Fairclough DL, Harris JR, Weeks JC (1997) Patient preferences concerning the trade-off between the risks and benefits of routine radiation therapy after conservative surgery for early-stage breast cancer. J Clin Oncol 15(3):1252–1260. https://doi.org/10.1200/jco.1997.15.3.1252
Jagsi R, Abrahamse P, Morrow M, Hawley ST, Griggs JJ, Graff JJ, Hamilton AS, Katz SJ (2010) Patterns and correlates of adjuvant radiotherapy receipt after lumpectomy and after mastectomy for breast cancer. J Clin Oncol 28(14):2396–2403. https://doi.org/10.1200/jco.2009.26.8433
Haviland JS, Owen JR, Dewar JA, Agrawal RK, Barrett J, Barrett-Lee PJ, Dobbs HJ, Hopwood P, Lawton PA, Magee BJ, Mills J, Simmons S, Sydenham MA, Venables K, Bliss JM, Yarnold JR (2013) The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol 14(11):1086–1094. https://doi.org/10.1016/s1470-2045(13)70386-3
Whelan TJ, Pignol JP, Levine MN, Julian JA, MacKenzie R, Parpia S, Shelley W, Grimard L, Bowen J, Lukka H, Perera F, Fyles A, Schneider K, Gulavita S, Freeman C (2010) Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med 362(6):513–520. https://doi.org/10.1056/NEJMoa0906260
Hoopes DJ, Kaziska D, Chapin P, Weed D, Smith BD, Hale ER, Johnstone PA (2012) Patient preferences and physician practice patterns regarding breast radiotherapy. Int J Radiat Oncol Biol Phys 82(2):674–681. https://doi.org/10.1016/j.ijrobp.2010.11.077
Kawaguchi H, Tsujino K, Miki M, Matsumoto Y, Ota Y, Hirokaga K, Takao S, Soejima T, Sasaki R (2019) Patient preference study comparing hypofractionated versus conventionally fractionated whole-breast irradiation after breast-conserving surgery. Jpn J Clin Oncol 49(6):545–553. https://doi.org/10.1093/jjco/hyz003
Bonin K, McGuffin M, Presutti R, Harth T, Mesci A, Feldman-Stewart D, Chow E, DiProspero L, Vesprini D, Rakovitch E, Lee J, Paszat L et al (2018) Breast cancer patients' preferences for adjuvant radiotherapy post lumpectomy: whole breast irradiation vs partial breast irradiation-single institutional study. J Cancer Educ 33(1):37–43
Vaidya JS, Wenz F, Bulsara M, Tobias JS, Joseph DJ, Keshtgar M, Flyger HL, Massarut S, Alvarado M, Saunders C, Eiermann W, Metaxas M, Sperk E, Sutterlin M, Brown D, Esserman L, Roncadin M, Thompson A, Dewar JA, Holtveg HM, Pigorsch S, Falzon M, Harris E, Matthews A, Brew-Graves C, Potyka I, Corica T, Williams NR, Baum M (2014) Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer: 5-year results for local control and overall survival from the TARGIT-a randomised trial. Lancet 383(9917):603–613. https://doi.org/10.1016/s0140-6736(13)61950-9
Alvarado MD, Conolly J, Park C, Sakata T, Mohan AJ, Harrison BL, Hayes M, Esserman LJ, Ozanne EM (2014) Patient preferences regarding intraoperative versus external beam radiotherapy following breast-conserving surgery. Breast Cancer Res Treat 143(1):135–140. https://doi.org/10.1007/s10549-013-2782-9
Spaich S, Krickeberg S, Hetjens S, Wenz F, Gerhardt A, Sutterlin M (2019) Patient preferences regarding intraoperative versus external beam radiotherapy for early breast cancer and the impact of socio-demographic factors. Arch Gynecol Obstet 299(4):1121–1130. https://doi.org/10.1007/s00404-018-5025-9
Corica T, Saunders CM, Bulsara MK, Taylor M, Joseph DJ, Nowak AK (2019) Patient preferences for adjuvant radiotherapy in early breast cancer are strongly influenced by treatment received through random assignment. Eur J Cancer Care (Engl) 28(2):e12985. https://doi.org/10.1111/ecc.12985
Sepucha KR, Scholl I (2014) Measuring shared decision making: a review of constructs, measures, and opportunities for cardiovascular care. Circ Cardiovasc Qual Outcomes 7(4):620–626. https://doi.org/10.1161/circoutcomes.113.000350
Sepucha KR, Belkora JK, Chang Y, Cosenza C, Levin CA, Moy B, Partridge A, Lee CN (2012) Measuring decision quality: psychometric evaluation of a new instrument for breast cancer surgery. BMC Med Inform Decis Mak 12:51. https://doi.org/10.1186/1472-6947-12-51
Wallston KA, Wallston BS, DeVellis R (1978) Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Educ Monogr 6(2):160–170. https://doi.org/10.1177/109019817800600107
Russo S, Jongerius C, Faccio F, Pizzoli SFM, Pinto CA, Veldwijk J, Janssens R, Simons G, Falahee M, de Bekker-Grob E, Huys I, Postmus D, Kihlbom U, Pravettoni G (2019) Understanding patients' preferences: a systematic review of psychological instruments used in patients' preference and decision studies. Value Health 22(4):491–501. https://doi.org/10.1016/j.jval.2018.12.007
Degner LF, Sloan JA, Venkatesh P (1997) The Control Preferences Scale. Can J Nurs Res 29(3):21–43
Mulhern B, Norman R, Street DJ, Viney R (2019) One method, many methodological choices: a structured review of discrete-choice experiments for health state valuation. Pharmacoeconomics 37(1):29–43. https://doi.org/10.1007/s40273-018-0714-6
Louviere J, Flynn T, Carson R (2010) Discrete choice experiments are not conjoint analysis. J Choice Model 3:57–72
Gafni A (1994) The standard gamble method: what is being measured and how it is interpreted. Health Serv Res 29(2):207–224
Stiggelbout AM, de Haes JC (2001) Patient preference for cancer therapy: an overview of measurement approaches. J Clin Oncol 19(1):220–230. https://doi.org/10.1200/jco.2001.19.1.220
Ballinger RS, Mayer KF, Lawrence G, Fallowfield L (2008) Patients' decision-making in a UK specialist centre with high mastectomy rates. Breast 17(6):574–579. https://doi.org/10.1016/j.breast.2008.08.001
Collins ED, Moore CP, Clay KF, Kearing SA, O'Connor AM, Llewellyn-Thomas HA, Barth RJ, Sepucha KR (2009) Can women with early-stage breast cancer make an informed decision for mastectomy? J Clin Oncol 27(4):519–525. https://doi.org/10.1200/jco.2008.16.6215
Hamelinck VC, Bastiaannet E, Pieterse AH, van de Velde CJH, Liefers GJ, Stiggelbout AM (2018) Preferred and perceived participation of younger and older patients in decision making about treatment for early breast cancer: a prospective study. Clin Breast Cancer 18(2):e245–e253. https://doi.org/10.1016/j.clbc.2017.11.013
Kirby RM, Basit A, Manimaran N (2008) Patient choice significantly affects mastectomy rates in the treatment of breast cancer. Int Semin Surg Oncol 5:20. https://doi.org/10.1186/1477-7800-5-20
Lazovich D, Raab KK, Gurney JG, Chen H (2000) Knowledge and preference for breast conservation therapy among women without breast cancer. Womens Health Issues 10(4):210–216. https://doi.org/10.1016/s1049-3867(00)00045-1
Mandelblatt JS, Hadley J, Kerner JF, Schulman KA, Gold K, Dunmore-Griffith J, Edge S, Guadagnoli E, Lynch JJ, Meropol NJ, Weeks JC, Winn R (2000) Patterns of breast carcinoma treatment in older women: patient preference and clinical and physical influences. Cancer 89(3):561–573
Mastaglia B, Kristjanson LJ (2001) Factors influencing women's decisions for choice of surgery for Stage I and Stage II breast cancer in Western Australia. J Adv Nurs 35(6):836–847. https://doi.org/10.1046/j.1365-2648.2001.01921.x
Molenaar S, Oort F, Sprangers M, Rutgers E, Luiten E, Mulder J, de Haes H (2004) Predictors of patients' choices for breast-conserving therapy or mastectomy: a prospective study. Br J Cancer 90(11):2123–2130. https://doi.org/10.1038/sj.bjc.6601835
Sivell S, Elwyn G, Edwards A, Manstead AS (2013) Factors influencing the surgery intentions and choices of women with early breast cancer: the predictive utility of an extended theory of planned behaviour. BMC Med Inform Decis Mak 13:92. https://doi.org/10.1186/1472-6947-13-92
Staradub VL, Hsieh YC, Clauson J, Langerman A, Rademaker AW, Morrow M (2002) Factors that influence surgical choices in women with breast carcinoma. Cancer 95(6):1185–1190. https://doi.org/10.1002/cncr.10824
Storm-Dickerson T, Das L, Gabriel A, Gitlin M, Farias J, Macarios D (2018) What drives patient choice: preferences for approaches to surgical treatments for breast cancer beyond traditional clinical benchmarks. Plast Reconstr Surg Glob Open 6(4):e1746. https://doi.org/10.1097/gox.0000000000001746
Hooper RC, Hsu J, Duncan A, Bensenhaver JM, Newman LA, Kidwell KM, Chung KC, Momoh AO (2019) Breast cancer knowledge and decisions made for contralateral prophylactic mastectomy: a survey of surgeons and women in the general population. Plast Reconstr Surg 143(5):936e–945e. https://doi.org/10.1097/prs.0000000000005523
Rosenberg SM, Greaney ML, Patenaude AF, Sepucha KR, Meyer ME, Partridge AH (2018) "I don't want to take chances": a qualitative exploration of surgical decision making in young breast cancer survivors. Psychooncology 27(6):1524–1529. https://doi.org/10.1002/pon.4683
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CAM reports no disclosures. TAK has received speaker fees from Genomic Health. EAM reports receiving honoraria from Physician Education Resource; paid compensation for participation on Scientific Advisory Boards for Genomic Health, Merck, Paregrine Pharmaceuticals, Sella Life Science, and Tapimmune; and research funding from Glaxo SmithKline. Her institution has received research funding from Astra Zeneca, EMD Serono, Galena Biopharma and Genentech/Roche.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Minami, C.A., King, T.A. & Mittendorf, E.A. Patient preferences for locoregional therapy in early-stage breast cancer. Breast Cancer Res Treat 183, 291–309 (2020). https://doi.org/10.1007/s10549-020-05737-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05737-9