The stark nakedness and simplicity of the conflict with which humanity is oppressed—that of getting angry with and wishing to hurt the very person who is most loved.
― John Bowlby.
Abstract
Intimate partner violence (IPV) is a major public health concern, with increasing rates of IPV being seen around the world during the COVID-19 pandemic. Previous research has linked the perpetration of IPV and other forms of sexual violence to aspects of romantic attachment psychology, with insecure anxious/preoccupied attachment most often linked to higher rates of IPV. Stressful events typically activate the attachment system and may either aggravate or disrupt its regulatory functioning. In the present study, we investigated whether COVID-related PTSD and depressive symptoms were associated with increased IPV perpetration and whether this relationship was moderated by levels of attachment security. Our findings indicated that higher COVID-related PTSD was significantly associated with increased IPV perpetration in securely attached individuals, whereas depressive symptoms was significantly associated with decreased IPV perpetration in securely attached individuals. IPV perpetration by insecure individuals was consistently high regardless of COVID-related PTSD or depressive symptoms. These findings suggest that COVID-related PTSD may erode adaptive attachment functioning, particularly among the previously secure, which can have important consequences for secure individuals and their intimate partners. The present findings may explain some of the recent increase in IPV cases worldwide and serve to raise awareness and motivate clinical interventions to more efficiently help both victims and perpetrators of IPV stay safe while staying home.
Similar content being viewed by others
Introduction
Once COVID-19 was pronounced a pandemic, countries began to adopt extreme behavioral interventions such as mandating physical distancing, encouraging social isolation, and at times implementing full community quarantines to slow down and contain its spread (Campbell, 2020; van Gelder et al., 2020). Although these essential public health strategies were paramount for infection control, they required individuals to remain for long periods inside their homes. This residential isolation was accompanied not only by fear and worry about one’s personal health, but also by concerns about negative economic consequences (e.g., rising unemployment figures; Kennedy, 2020), shortages of essential resources (Mannelli, 2020; McMahon et al., 2020), and heightened family burdens such as increased childcare obligations resulting from school closures (Canady, 2020; Kowal et al., 2020; Wang et al., 2022).
This prolonged and intense period of social seclusion inside the home, combined with uncertainty surrounding the duration of the lockdown and the progression of the pandemic, appears to have amplified general stress levels for most adults. For instance, the average stress level related to COVID-19, as well as the general stress level in American adults, was significantly higher than the average stress level reported in the previous year (Annual Stress in America, 2019; Kennedy, 2020). A tracking poll showed that 53% of adults in the USA reported that COVID-19 has had a negative impact on their mental health (KFF, 2020).
Several studies from around the world seem to confirm that social isolation and quarantine experiences related to COVID-19 have had negative psychological consequences, including heightening levels of anxiety, depression, anger, confusion, and stress (Brooks et al., 2020). Fear regarding the unknown nature of COVID-19, for instance, was associated with increased mental health disorders (Shigemura et al., 2020), with those affected across a range of other cultures demonstrating several symptoms of mental trauma including depression and post-traumatic stress disorder (PTSD) (Brooks et al., 2020; Rubin & Wessely, 2020; Sun et al. 2021; Tang et al., 2020; Wang et al., 2022). In a study of university students in China, the prevalence of PTSD and depression one month after the pandemic was 2.7% and 9.0%, respectively (Tang et al., 2020). A longitudinal survey of the general population in China found increased levels of PTSD symptoms during the initial outbreak as well as 4 weeks later (Wang et al., 2022). Significant increases of PTSD and depression since the onset of COVID-19 have also been found in Italy (Forte et al., 2020), Spain (González-Sanguino et al., 2020), the UK (Shevlin et al., 2020), and Lebanon (Fawaz & Samaha, 2020). Moreover, in the USA, a study of young adults showed that high levels of COVID-related worry were linked with clinical levels of PTSD and depressive symptoms (Liu et al., 2020). Recent studies including a meta-analysis supported the notion that COVID-19 can be interpreted as a traumatic event due to the PTSD responses found in the general population across several cultures—even in people that were not infected with the virus (Bridgland et al., 2021; Cooke et al., 2020).
Indeed, recent research proposed that COVID-19-related stress and worries (e.g., contracting the virus, social distancing, lifestyle and interpersonal relationship changes, uncertainty of the future, economic problems, and so forth) may even generate a new form of trauma (Forte et al., 2020). In addition, changes in employment status and income due to lockdown, may limit access to essential needs and services and cause heightened frustration and distress for individuals and their families (Brooks et al., 2020). Indeed, mental health issues have been previously associated with low socioeconomic status (SES) during COVID-19 (Marmet et al., 2021). Combined, these findings suggest that the COVID-19 pandemic may be experienced as a truly traumatic event in people’s lives all around the world. As with past research on natural disasters (Beaglehole et al., 2018) and other epidemic emergencies (James et al., 2019), these traumatic situations are likely increasing people’s levels of PTSD and depressive symptoms and can have major consequences.
The trauma of COVID-19 does not only impact individuals, but can further take a toll on interpersonal relationships, specifically intimate partnerships (Marshall & Kuijer, 2017). For instance, mental health issues have been consistently linked to an increased risk of perpetrating intimate partner violence (IPV; Cano & Vivian, 2003; Capaldi et al., 2012; Frye & Karney, 2006; Langer et al., 2008; Mason & Smithey, 2012; Roberts et al., 2011; Taft et al., 2011; van Gelder et al., 2020). Particularly, stress and mood disorders such as PTSD and depression have been linked with IPV perpetration across cultures (Bell & Orcutt, 2009; Dowd et al., 2005; Kirby et al., 2012; Shorey et al. 2015; Swan et al., 2005). IPV refers to any behavior carried out to inflict harm to romantic partners (Anderson & Bushman, 2002; Baron & Richardson, 1994) and is a public health and human rights issue worldwide (Magdol et al., 1997; McLaughlin et al., 1992; Straus, 2008).
IPV tends to increase during humanitarian crises and emergencies (Chandan et al., 2020; Roesch et al., 2020; Stark & Ager, 2011; World Health Organization, 2020). Since social isolation and stay-at-home measures came into force to slow down the spread of COVID-19, countries around the world have reported significant increases in IPV and domestic abuse cases (Campbell, 2020; Peterman et al., 2020; van Gelder et al., 2020). For instance, domestic abuse cases rose threefold in Wuhan, the first province in China under mass quarantine (Allen-Ebrahimian, 2020), and the European Union saw a significant increase of IPV with several reports of homicide related to family violence (Bradbury-Jones & Isham, 2020; Wagers, 2020). The National Domestic Abuse Hotline in the UK reported a 25% increase in calls since the COVID-19 lockdown (Kelly & Morgan, 2020) and both Italian and French governments commissioned hotels to shelter the rising number of individuals fleeing abusive homes (Davies & Batha, 2020). In the USA, domestic violence cases increased between 21 and 35% across several states (Wagers, 2020), and a 75% increase of domestic abuse support searches was observed on Google (Poate, 2020). It appears the increase of mental health issues due to COVID-19 has exacerbated IPV as a public health issue. However, not all individuals respond to PTSD and depressive symptoms with IPV perpetration. Indeed, individuals vary widely in their sensitivity to threats and their arousal of negative emotions that might further inform IPV perpetration in the time of COVID-19.
Stress Regulation and the Attachment System
Individual differences in attachment may be particularly relevant for explaining how individuals regulate their anger in times of stress (Bowlby, 1973; Mikulincer & Shaver, 2007, 2011). During human evolutionary history, infants heavily relied on primary caregivers for their survival to reproductive age. Attachment theory posits that infants are born with an innate psycho-biological system (the attachment system; Bowlby, 1973) which is activated during distress and functions to motivate proximity-seeking to an attachment figure for safety, comfort, and support (Bowlby, 1969; Mikulincer & Shaver, 2007). Once this is achieved and the infant feels safe, the attachment system is deactivated, and over time these stabilizing activation-deactivation attachment experiences in response to stress result in a “secure” attachment style. However, when the attachment figure is unavailable or unreliable, the attachment system fails to learn stabilizing patterns of activation-deactivation attachment in response to stress. These early attachment experiences provide inadequate and unstable stress regulation that interfere with the development of psychological resources needed for coping with stressors. Consequently, such individuals may develop an insecure attachment style, characterized by either anxious or avoidant attachment (Brennan et al., 1998).
Provided that exposure to stressful and traumatic events such as the COVID-19 pandemic can cause overwhelming feelings of panic and helplessness (Horowitz 1982), the attachment behavioral system should be activated by stressors related to COVID-19 (Besser et al., 2009; Mikulincer & Shaver, 2007). However, each attachment style is associated with specific coping mechanisms for affect regulation in response to distress or threat (Mikulincer & Shaver, 2007; Simpson & Rholes, 2017). Whereas attachment security is associated with reliance on intimate partners and the ability to employ flexible strategies, such as problem solving and reappraisal, to regulate distress (Mikulincer & Shaver, 2007), individuals with an insecure attachment style resort to different coping mechanisms. For instance, attachment anxiety has been linked with hyperactivating strategies such as reassurance seeking and over-dependence on support from intimate partners (Mikulincer & Shaver, 2012). Attachment avoidance, in contrast, has been linked with deactivating strategies, such as self-reliance and withdrawal from intimate partners (Mikulincer & Shaver, 2012). Consequently, these responses to stress not only require increased effort and responsiveness from intimate partners, they could also result in destructive communication patterns and low relationship quality (Mikulincer & Shaver, 2007; Petromonaco & Beck, 2015). These normative relationship processes could be further degraded by added stressors from the pandemic. For instance, individuals with anxious attachment under stress may seek excessive reassurance from intimate partners who also experience distress due to the pandemic (Overall et al., 2014; Shaver et al., 2005).
Moreover, if anxious individuals are partnered with someone who has an avoidant attachment style, they may need to increase their effort to receive sufficient and effective support (Beck et al., 2013; Girme et al., 2015). This interplay between partners’ attachment styles may exacerbate their struggle to cope and adapt to the COVID-19 crisis. Indeed, if both partners have an insecure attachment style (e.g., anxious-avoidant couples), they may have more problematic behavioral responses and communication patterns (Beck et al., 2013; Shallcross et al., 2011). For instance, an anxious person may react to an avoidant partner’s withdrawal from conflict with protest behaviors that could escalate in violence to get their need for reassurance and safety met. Conversely, if an avoidant person cannot escape from conflict due to a persistent anxious partner, they may resort to coercive tactics to create the space they need to cope with distress (Overall et al., 2014).
Potentially most relevant to the context of COVID-19, attachment styles have been found to moderate mental and relational responses to stressful life events (Mikulincer & Shaver, 2012). For instance, prolonged and chronic stress has been shown to aggravate attachment insecurities in individuals with both anxious and avoidant attachment styles (Mikulincer & Shaver, 2012). Therefore, insecurely attached individuals may be more likely to develop PTSD and depressive symptoms during COVID-19 (Mikulincer et al., 2014) and consequently may be more at risk of experiencing anger and aggression, including employing violence against intimate partners during conflict (Bond & Bond, 2004; Henderson et al., 2005; Schumacher et al., 2001; Stith et al., 2004).
Additionally, Mikulincer et al. (2015) proposed that prolonged, and chronic stress may disrupt normal attachment functioning of individuals with a secure attachment style. As such, stressors experienced during the COVID-19 pandemic could make secure individuals feel more vulnerable, promote relational worries, and potentially alter their perception of receiving sufficient support from intimate partners (e.g., Baldwin & Fehr, 1995; Davila & Cobb, 2004). Consequently, a failure to successfully cope with intense feelings of distress could keep the attachment system of secure people persistently activated, thereby eroding their sense of security and ultimately lower relationship quality (Mikulincer & Shaver, 2012). Indeed, individuals with persistent and pervasive stress were found to report higher attachment anxiety and avoidance and were less likely to activate security-related representations when exposed to threats (Mikulincer et al., 2015).
Previous studies that have investigated the impact of stress on attachment styles have mostly used laboratory environments (e.g., Carpenter & Kirkpatrick, 1996). COVID-19 provided a unique and naturalistic opportunity to assess the impact of a current, major life event and stressor on attachment styles and consequently, intimate relationships (Elkins et al., 2013; Finkel, 2013; Finkel & Eckhardt, 2013; Langhinrichsen-Rohling et al. 2012; Whitaker et al., 2013). We evaluated the following three hypotheses regarding stress, PTSD, and depression and their links to IPV within romantic relationships.
Hypothesis 1a
COVID-related PTSD will be positively associated with IPV perpetration in higher (vs. lower) levels of attachment anxiety and higher (vs. lower) avoidance.
Hypothesis 1b
Relatively secure individuals (lower levels of anxiety and lower levels of avoidance) will report heightened IPV perpetration under heightened levels of COVID-related PTSD.
Hypothesis 2
COVID-related depressive symptoms will be positively associated with IPV perpetration in higher (vs. lower) levels of attachment anxiety and higher (vs. lower) avoidance.
Method
Participants
Data were originally collected from 975 participants via MTurk. Provided individuals in exclusive intimate relationships were more likely to meet during COVID-lockdown and spend more time together at home unlike single individuals, the present study will focus on a subsample of participants (N = 812) who reported being in a romantic relationship (N = 92, 9.4%), cohabitating (N = 44, 4.5%), and married (N = 676, 69.3%) to assess their use of IPV perpetration. The mean age of participants was 35.26 years (SD = 10.47). Most participants 67.1% were men (N = 563) and 32.9% were women (N = 320), of which (N = 731, 75%) reported being attracted to individuals of the opposite sex, (N = 41, 4.2%) reported being attracted to individuals of the same sex and (N = 204, 20.9%) reported being attracted to both individuals of the opposite and same sex. Most participants (59.2%) reported living in the USA (N = 567), 3.3% resided in Europe (N = 32), 1.6% were from Brazil (N = 16), and 21.7% of participants resided in Asia, mostly in India (N = 212). COVID-19 was officially declared a pandemic in March 2020, and lockdown measures were immediately introduced worldwide. Data for the present study were collected in May 2020 (two months into COVID-lockdown). Although the degree of lockdown measures varied across nations and territories, according to an AFP database, around 4.5 billion people spanning 110 countries were obliged to stay home and were subject to partial or complete lockdown for up to two months prior to—and during data collection. All study procedures outlined below were approved by the university at which the research was conducted.
Procedure
Prospective participants viewed an advertisement for the study for a participation compensation fee of $0.50 on MTurk’s job listings. It has been suggested that participants recruited from MTurk tend to be more demographically diverse than those from standard internet samples and college samples (Buhrmester et al., 2011). Moreover, there was no association between compensation rates and data quality, and data collected on MTurk tend to be equally reliable as those retrieved via traditional methods (Gosling et al., 2004). Participants who were willing and eligible to participate (i.e., at least 18 years of age) were provided a link to an informed consent statement about the study. Those who agreed to participate could access and complete the survey, and those who did not agree to participate were exited from the study.
Measures
The Impact of Event Scale (Revised, Weiss & Marmar, 1997) is a 22-item scale which is rated on a 0 (not at all) to 4 (extremely) scale and was used to assess PTSD-responses to COVID-19 in the general population (e.g., “I had trouble concentrating,” “I felt irritable and angry,” “I had trouble staying asleep”). The instructions were adapted to specifically apply to COVID-19, e.g., “how distressing each item has been since the onset of COVID-19 lockdown.” PTSD is a common emotional disorder in the general population after a disaster. Research from previous viral outbreaks as well as from the most recent COVID-19 pandemic indicates that viral outbreaks and imposed quarantine measures can be traumatic for individuals and may result in PTSD. Indeed, PTSD in the general population has been described as a second tsunami of COVID-19 (Dutheil et al., 2021). To measure traumatic stress symptoms in the context of viral outbreaks, the Impact of Event Scale has been shown to be valuable (Horowitz et al., 1979) and has been used in several studies to assess the impact of COVID-19 in the general population across several countries (Cooke et al., 2020; Zhang et al., 2021). Importantly, compared to other self-report measures of psychological impact, the advantage of using the IES-R is that the event can be specified. Indeed, the IES-R adapted for COVID-19 has been found to be a valid measure of traumatic stress symptoms associated with the COVID-19 pandemic (Zhang et al., 2021). The IES-R with modifications for COVID-19 (Vanaken et al., 2020) showed acceptable internal validity (α = 0.75). The current study found good internal consistency for the COVID-adjusted IES scale (α = 0.96). The maximum score of the IES is 88. A score of 33–38 is the cutoff for a clinical diagnosis of PTSD (Creamer et al., 2003). Moreover, a score of 39 and above has been shown capable of suppressing the functioning of the immune system for ten years following the traumatic event (Kawamura et al., 2001).
The CES-D scale, a self-report depression scale for research in the general population (Radloff, 1977), is a 20-item measure assessing symptoms of depression in the general population with items phrased as self-statements (e.g., “I felt sad,” “I felt lonely,” “I felt hopeful about the future”). Respondents rated how frequently each item applied to them since the COVID-19 lockdown. Ratings were based on a 4-point Likert scale ranging from 0 (rarely or none of the time [less than 1 day]) to 3 (most or all of the time [5–7 days]). Previous studies reported an internal consistency ranging from 0.74 to 0.95 (Straus 2007; Straus et al., 1996). The current study found adequate internal reliability (α = 0.80). Higher scores signify greater symptoms, and the CES-D cutoff score is 16 indicating a risk for clinical depression ranging from “mild” (16–23) to “severe” (24–60) depressive symptomatology (Radloff, 1977).
Intimate partner violence perpetration was measured using The Revised Conflict Tactics Scales (CTS2; Straus et al., 1996). The CTS2 contains five subscales: psychological aggression, physical assault, sexual coercion, negotiation, and sustained injury. Considering the focus of the present research is on perpetration (and not victimization) of IPV, the subsequent analyses focused on the physical (e.g., “Slammed my partner against a wall”) and sexual (e.g., “Used force to make my partner have sex”) perpetration domains. Items were rated on a 6-point scale ranging from 1 (once since the lockdown) to 6 (more than 20 times since the lockdown).
To assess romantic attachment, participants completed the 12-item Experiences in Close Relationships Inventory-Short (ECR-S; Wei et al. 2007). Sample questions include “It helps to turn to my romantic partner in times of need” (anxiety subscale) and “I want to get close to my partner, but I keep pulling back” (avoidance subscale). Items were rated using a 7-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). An overall score was computed for the 6 items each anxious and avoidant subscales. The original article found good internal reliability for anxious attachment (α = 0.78–0.86) and avoidant attachment (α = 0.78–0.88). The current study similarly found adequate internal reliability for anxious attachment (α = 0.72) and avoidant attachment (α = 0.87).
SES-harm was measured with one item “Has your household been negatively affected by the lockdown” and scored on a scale from 1 (none at all) to 5 (a great deal).
Results
COVID-Related PTSD
Tables 1 and 2 contain descriptive statistics for all participants and intercorrelations among all study variables. The mean COVID-IES-R score for all participants was M = 38.13 (SD = 18.07), with male participants M = 38.78 (SD = 18.09) and female participants M = 36.85 (SD = 17.98), indicating the likely presence of PTSD. Those in an exclusive relationship indicated a mean score of M = 28 (SD = 17.50), participants who were cohabitating indicated a mean score of M = 23.90 (SD = 16.73), and those who were married were found to indicate a mean score of M = 40.75 (SD = 17.03). This may suggest that COVID-related PTSD may be especially present in married individuals. Demographic variables that had statistically significant negative associations with COVID-IES score were age and SES (see Table 1).
Two moderation analyses were run with SPSS PROCESS macro (Hayes, 2017) to examine the relationship between COVID-related PTSD and IPV. To assess whether anxious and avoidant attachment style moderated this relationship, age, gender, SES-harm, depressive symptoms, and avoidant attachment style, respectively, were controlled for. All variables were mean-centered and deviation scores calculated to enable creation of the interaction term (see Table 3).
COVID-related PTSD was associated with IPV, b = 0.08, p = .02, 95% CI [1.3, 19.12]. There was no relationship between anxious attachment and IPV perpetration; however, attachment significantly moderated the relationship between PTSD and IPV perpetration as indicated by the significant interaction effect of anxious attachment and PTSD, b = − 0.01, p < .001, 95% CI [− 0.01, − 0.01]. PTSD and anxious attachment explained 12.14% of the variability in IPV. The second moderation investigating the moderated effect of avoidant attachment showed that PTSD was related to IPV, b = 0.07, p = .04, 95% CI [0.01, 0.14]. There was no relationship between avoidant attachment, and IPV perpetration. However, there was a significant interaction effect of attachment avoidance and PTSD, b = − 0.01, p < .001, 95% CI [− 0.02, − 0.01]. PTSD and avoidant attachment explained 12.09% of the variability in IPV.
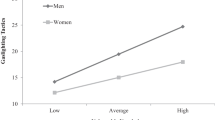
Simple slopes analyses were used to further examine the combined effect of PTSD and anxious and avoidant attachment, respectively, on IPV perpetration (Field, 2013). The interaction between PTSD and IPV perpetration was tested at low (minus one standard deviation below the mean), medium (mean), and high (plus one standard deviation above the mean) levels of anxious and avoidant attachment (see Figs. 1, 2). At low levels of anxious attachment, there was a positive relationship between PTSD and IPV, b = 0.15, p < .001, 95% CI [0.08, 0.23]. At medium levels of anxious attachment, there was a positive relationship between PTSD and IPV, b = 0.08, p = .03, 95% CI [0.01, 0.15]. There was no significant relationship between PTSD and IPV at high levels of anxious attachment, b = 0.01, p = .89, 95% CI [− 0.08, 0.09] (see Fig. 1).
Effect of COVID-PTSD on IPV moderated by Anxious Attachment. Note: IPV = intimate partner violence. Effect of COVID-PTSD on IPV as moderated by anxious attachment and controlling for age, gender, SES, COVID-depressive symptoms, and avoidant attachment. As COVID-PTSD increases, IPV decreases in individuals with low levels of anxious attachment (relatively secure attachment)
Effect of COVID-PTSD on IPV moderated by Avoidant Attachment. Note: IPV = intimate partner violence. Effect of COVID-PTSD on IPV as moderated by avoidant attachment and controlling for age, gender, SES, COVID-depressive symptoms, and anxious attachment. As COVID-PTSD increases, IPV decreases in individuals with low levels of avoidant attachment (relatively secure attachment)
At low levels of avoidant attachment, there was a positive relationship between PTSD and IPV, b = 0.15, p < .001, 95% CI [0.08, 0.23]. At medium levels of avoidant attachment, there was no relationship between PTSD and IPV, b = 0.07, p = .05, 95% CI [0.00, 0.15]. There was no relationship between PTSD and IPV at high levels of avoidant attachment, b = − 0.00, p = .93, 95% CI [− 0.09, 0.09] (see Fig. 2).
COVID-Related Depressive Symptoms
Tables 1 and 2 contain descriptive statistics and intercorrelations among all participants and study variables. The mean CES-D score for all participants was M = 34.87 (SD = 9.53), with male participants M = 34.76 (SD = 9.30) and female participants M = 35.07 (SD = 9.98), indicating severe depressive symptomatology and an increased risk for clinical depression. Those in an exclusive relationship indicated a mean score of M = 39.62 (SD = 8.21), participants who were cohabitating indicated a mean score of M = 40.38 (SD = 7.48), and those who were married were found to indicate a mean score of M = 34.00 (SD = 9.52). Demographic variables that had statistically significant positive associations with CES-D score were age and SES (see Table 1).
Two moderation analyses were run with SPSS PROCESS macro (Hayes, 2017) to examine the relationship between COVID-related depressive symptoms and IPV. To assess whether anxious and avoidant attachment style moderated this relationship, age, gender, SES-harm, PTSD, anxious and avoidant attachment style, respectively, were controlled for. All variables were mean-centered and deviation scores calculated to enable creation of the interaction term (see Table 4).
COVID-related depressive symptoms were not associated with IPV perpetration, and there was also no relationship between anxious attachment and IPV perpetration. However, anxious attachment significantly moderated the relationship as indicated by the significant interaction effect of anxious attachment and depressive symptoms, b = 0.02, p < .001, 95% CI [0.01, − 0.03]. COVID-related depressive symptoms and anxious attachment explained 12.23% of the variability in IPV perpetration. The second moderation investigating the moderated effect of avoidant attachment, showed no relationship between depressive symptoms and IPV perpetration and there was no relationship between avoidant attachment and IPV perpetration. However, there was a significant interaction effect of depressive symptoms and avoidant attachment indicating that avoidant attachment significantly moderated the relationship between depressive symptoms and IPV perpetration, b = 0.03, p < .001, 95% CI [0.01, 0.04]. Depressive symptoms and avoidant attachment explained 11.8% of the variability in IPV.
Simple slopes analyses were used to further examine the combined effect of depressive symptoms and anxious and avoidant attachment, respectively, on IPV perpetration (Field, 2013). The interaction between depressive symptoms and IPV perpetration were tested at low (minus one standard deviation below the mean), medium (mean), and high (plus one standard deviation above the mean) levels of anxious and avoidant attachment (see Figs. 3, 4). At low levels of anxious attachment, there was no relationship between depressive symptoms and IPV, b = − 0.10, p = .25, 95% CI [− 0.25, 0.07]. At medium levels of anxious attachment, there was also no relationship between depressive symptoms and IPV, b = 0.06, p = .37, 95% CI [− 0.07, 0.20]. There was a significant relationship between depressive symptoms and IPV at high levels of anxious attachment, b = 0.22, p = .003, 95% CI [0.07, 0.36] (see Fig. 3).
Effect of COVID-depressive symptoms on IPV moderated by Anxious Attachment. Note: IPV = intimate partner violence. Effect of COVID-depressive symptoms on IPV as moderated by anxious attachment and controlling for age, gender, SES, COVID-PTSD and avoidant attachment. As COVID-depressive symptoms increase, IPV increases in individuals with high levels of anxious attachment
Effect of COVID-depressive symptoms on IPV moderated by Avoidant Attachment. Note: IPV = intimate partner violence. Effect of COVID-depressive symptoms on IPV as moderated by avoidant attachment and controlling for age, gender, SES, COVID-PTSD and anxious attachment. As COVID-depressive symptoms increase, IPV increases in individuals with high levels of avoidant attachment
At low levels of avoidant attachment, there was no relationship between depressive symptoms and IPV, b = − 0.09, p = .30, 95% CI [− 0.26, 0.08]. At medium levels of avoidant attachment, there was no relationship between depressive symptoms and IPV, b = 0.06, p = .39, 95% CI [− 0.08, 0.20]. There was a significant relationship between depressive symptoms and IPV at high levels of avoidant attachment, b = 0.21, p = .005, 95% CI [0.06, 0.35] (see Fig. 4).
Discussion
The emergence of the COVID-19 pandemic exacerbated another pre-existing public health issue–rates of IPV have increased globally. Previously, it was found that individuals with insecure attachment style (anxious and avoidant) are more at risk of developing PTSD and depressive symptoms due to stress, and moreover are more likely to perpetrate violence against intimate partners. The aim of the present study was to determine the extent to which COVID-19-related PTSD and depressive symptoms are related to IPV perpetration and whether these relationships are moderated by individuals’ attachment styles.
In line with Hypothesis 1a, the findings of the present study indicated that those with an insecure attachment style (high levels of anxiety, high levels of avoidance) reported higher levels of IPV perpetration under high levels of COVID-related PTSD; however, contrary to what was expected, there was no difference in frequency of IPV perpetration at lower levels vs higher levels of COVID-related PTSD. This means that insecure individuals (both anxious and avoidant) perpetrated violence against intimate partners at equal frequency regardless of COVID-related PTSD.
Moreover, in line with Hypothesis 1b, there was a significant increase in IPV among individuals with a relatively secure attachment style (low levels of anxiety and low levels of avoidance) under high levels of COVID-related PTSD compared to low levels of COVID-related PTSD. This suggests that individuals with a relatively secure attachment style may be at risk of perpetrating violence against intimate partners under heightened distress. Previously, it was shown that persistent PTSD (related to war trauma) may disrupt the regulatory functioning of the attachment system and thereby erode attachment security (Mikulincer et al., 2014). It may therefore be that COVID-related PTSD disrupts the regulatory functions of secure individuals’ attachment system and disables the activation-deactivation responsiveness just when it is needed the most.
In light of Mikulincer et al.’s (2014) findings that among individuals with persistent PTSD, security priming failed to lower the availability of thoughts related to trauma or induce a positive mood in times of need, it may be that although the attachment system is activated, persistent PTSD may keep individuals feeling helpless and frustrated regardless of comfort and support from intimate partners. Moreover, the erosion of attachment security may result in poor relationship quality and consequently to IPV perpetration during conflict, thereby equating secure individuals to insecure people who show heightened IPV perpetration without any indication of COVID-related PTSD. Future studies will be needed to replicate these findings and should further investigate whether such erosions of attachment security have additional impacts on secure individuals’ intimate relationship quality.
From an attachment perspective, protest behaviors should function to signal or communicate distress to elicit help or support from attachment figures (Mikulincer & Shaver, Shaver & Mikulincer, 2002; Simpson et al., 1992). Consequently, it may be that certain individuals resort to more maladaptive protest behaviors in the form of violent responses when they need help the most (Gilbert & Allan, 1998). Indeed, aggression for signaling has been shown to occur more frequently in individuals with PTSD (Cantor, 2009), and serious threats may lead to the activation of aggressive defenses. Hyperarousal symptoms of anger, induced by COVID-19, may place individuals at an increased risk of perpetrating violence against intimate partners (Taft et al., 2011).
Alternatively, anger may serve as a means of influencing the behavior of intimate partners to attain a set goal of a hypothesized power/dominance behavioral system (DBS, Galinsky et al., 2003; Keltner et al., 2003). This biologically based system has been shown to guide dominance motivations and dominant behaviors in individuals and has been linked with various psychopathologies including PTSD (Johnson et al., 2012). From this perspective, experiencing a sense of power may serve as an approach orientation (e.g., heightened attention to rewards, Carver & White, 1994) or promotion orientation (e.g., heightened attention to threats, Higgins, 1998). Indeed, Mikulincer and Shaver (2011) suggested that consequences of elevated power are also moderated by individuals’ attachment styles because they are likely to depend on how one relates to others. Combined with research that has linked violence toward intimate partners with an attempt to maintain control and power (Hamberger et al., 2017; Hamby, 1996; Straus, 2008; Voith et al., 2020), it may be that individuals who develop COVID-related PTSD may feel powerless and resort to IPV to achieve a sense of control and power over intimate partners. This would further be in line with research showing that PTSD may play a role in the power and control dynamics that have been linked with the perpetration of IPV (Gilbar et al., 2020; Rosenbaum & Leisring, 2003; Taft et al., 2016). Future research should investigate the potentially pivotal role of the DBS in IPV perpetration during heightened distress.
The present study found, in line with Hypothesis 2, that higher levels of COVID-related depressive symptoms were linked with heightened IPV perpetration in insecure individuals (both anxious and avoidant attachment style). These findings provide support for previous research indicating that depressive symptoms due to COVID-19 may aggravate hyperactivating strategies and deactivating strategies may collapse under heightened distress which may place them at an increased risk of developing depressive symptoms (Mikulincer & Shaver, 2012; Mikulincer et al., 2000). Under heightened levels of COVID-related depressive symptoms, those with an insecure attachment style may fail to seek the support and safety from intimate partners and in their desperate state may resort to maladaptive protest behaviors which could escalate in IPV perpetration (e.g., “anger of despair,” Bowlby, 1973).
The present finding may also provide support for the notion that secure individuals are better at seeking support and safety from intimate partners, at least within the context of depressive reactions to stress. An evolutionary perspective of psychopathologies, whereby PTSD and depressive symptoms should function as independent defense strategies in response to adversity, may further explain this finding. Whereas PTSD induces action, often preceding an adversity, and is associated with increased aggression or IPV generally, and among those who are securely attached when under extreme stress (e.g., Orth & Wieland, 2006; Taft et al., 2011), depression induces a lack of action among the secure (Brown et al., 1995) precisely when it would otherwise be too energetically expensive or risky to aggress (Nesse, 2002; Nettle & Bateson, 2012). From this perspective, PTSD may be a trigger that activates IPV perpetration (among those who are secure and not normally high in IPV), whereas depression may decrease aggressive responses in times of conflict and individuals with a relatively secure attachment style may resort to more adaptive strategies to gain help and support from partners (Hagen, 1999, 2002; Hagen & Thomson, 2004; Shaver et al., 2001; Sheeber et al., 2001; Watson & Andrews, 2002). Future research is needed to investigate this notion further with respect to the differing interactions of attachment security with PTSD and depression in predicting IPV perpetration.
Strengths and Limitations
The present study is the first to investigate the implications of COVID-related mental health experiences and their interaction with attachment styles in predicting IPV perpetration. This research adds to the limited literature on the consequences of traumatic events on the attachment system and intimate relationship outcomes. The present findings provide support for both the notion that a) COVID-related PTSD may contribute to the way stressful and traumatic experiences erode attachment security and further increase the risk of IPV perpetration, and b) COVID-related depressive symptoms may contribute to the way stressful and traumatic experiences aggravate insecure individuals’ coping strategies and place them at an increased risk to perpetrate IPV. The strengths of the present study include its relatively large and international sample as well as the timing of data collection, which allowed for exploration of how COVID-related psychopathologies during the crucial period of a global lockdown may be associated with IPV perpetration. Importantly, the present findings need to be cautiously interpreted with respect to their limitations.
An important limitation of this research is that like most previous studies that have investigated associations between attachment styles and PTSD, the present study is cross-sectional and correlational, which means that the causal direction of these associations cannot be determined. Therefore, the generalizability of the present findings is limited, and further studies are needed to replicate and extend these findings.
More research is also needed on how traumatic events and PTSD affect the attachment system. Although previous longitudinal studies have investigated changes in PTSD as a function of attachment styles (e.g., Fraley et al., 2006), future research should investigate if the reverse implies to gain a better understanding of whether PTSD can disrupt attachment functions and erode attachment security over time, as well as how such outcomes could be reversed or prevented.
Although it has been shown that data collected via MTurk are of equal quality to data collected by other internet methods and from college undergraduates in person (Buhrmester et al., 2011; Casler et al., 2013) and tend to be more socioeconomically and ethnically diverse than traditional internet or college samples (Casler et al., 2013), the present study did not assess ethnic and socioeconomic diversity in participants other than their countries of residence and whether COVID-19 negatively impacted their finances. Moreover, the survey did not include measures that would ensure the high quality of the present MTurk data (e.g., attention check questions).
Cultural differences may also be taken into consideration as there could be regional differences in mental well-being depending on the severity of the outbreak, lockdown measures and regulations, government responses, dissemination of information related to COVID-19, national economy, and availability of medical supplies (Xiong et al., 2020; Zhang et al., 2021). Although the present study included a larger sample of Indian participants, cross-cultural differences were not explored. Moreover, data collection took place in May 2020, and some US states may had already lifted or resorted to more relaxed lockdown measures at the time of collection. Additional information about participants may contribute to a better understanding of individuals’ susceptibility to develop COVID-related PTSD and depressive symptoms and thereby place individuals at an increased risk of perpetrating violence against intimate partners. Such factors could further include whether participants had COVID-19 or not and the severity of symptoms, or if they are following social distancing measures, are working from home, or have children living in their household. Future studies should assess these individual, contextual, and cross-cultural differences further.
Although the present sample did not find any significant gender differences, individual differences in sexual orientation were not explored given the rather small sample size of LGBTQ + participants. Previous research has consistently found that LGBTQ + individuals may be more susceptible to develop psychopathologies and were also shown to have increased levels of anxiety and depressive symptoms due to COVID-19 (e.g., Forte et al., 2020; Liu et al., 2020; Sun et al. 2021). Consequently, future studies should explore the impact of COVID-related mental health issues on IPV perpetration in LGBT + individuals. Moreover, the present analyses did not distinguish between couples that were in a relationship, cohabitating or married. Future studies could further investigate context-dependent and dyadic variables that could impact the association of COVID-related PTSD and IPV such as relationship quality and the buffering role of partner support (e.g., Balzarini et al., 2020). Additional research is also needed to assess other risk factors found to promote IPV perpetration and that may be related to COVID-related PTSD and depressive symptoms, such as alcohol and drug abuse.
Finally, although the present study draws attention to the potential mental health issues that can arise from COVID-19, another limitation of the present study is that it did not assess how participants’ current mental health compares to their mental health well-being before COVID-19. Longitudinal studies will be needed to examine whether COVID-related PTSD and depressive symptoms may decrease over time as lockdown measures are eased and for the most part removed. When assessing the psychological impact of COVID-19, the duration of symptoms should be taken into consideration. From an evolutionary perspective, psychological responses to traumatic and stressful events can be protective (Brosschot et al., 2016; Yaribeygi et al., 2017). However, persistent stressors could result in chronic PTSD symptoms and may pose a long-term threat to individuals and their intimate partners which could last years (Kessler et al., 1995).
The present findings further point out the importance of identifying the mental health impact of COVID-19 in the general population. However, although the present study supports previous evidence that COVID-19 may be understood as a traumatic stressor, this interpretation could add to the issue of conceptual bracket creep in defining trauma and PTSD (McNally, 2003). Therefore, future studies investigating the impact of COVID-19 stress on individuals, should consider differentiating between evolutionary responses to stress and genuine symptoms of a disorder, specifically in the context of COVID-19 (e.g., Arpaci et al., 2020; Taylor et al., 2020).
Finally, the present study was not pre-registered; however for the purpose of transparency, the data for the specific variables including the syntax and output of the analyses were made public on OSF. Future studies should seek to replicate these findings using a pre-registered design.
Implications
A key finding of the present study was that secure individuals indicated heightened levels of IPV perpetration under heightened levels of COVID-related PTSD. An important novel contribution to the literature is that individuals with a relatively secure attachment style seem to perpetrate more violence against intimate partners under high levels of COVID-related PTSD, whereas heightened levels of COVID-related depressive symptoms are associated with heightened levels of IPV perpetration in insecure individuals. These findings could explain the recent and global spike in IPV cases during COVID-19 and highlight the importance for future research to integrate individual differences to better understand these differences in susceptibility to stress and trauma which can have profound consequences not only for individuals but also for their intimate partners. The present study also points out the necessity for developing both practical prevention and interventions to help people cope better with COVID-related stress and trauma. For example, psychological interventions in the form of cognitive processing therapy (CPT; Resick & Schnicke, 1992) which has been shown to be helpful for individuals with PTSD who perpetrate violence against intimate partners (Murphy & Eckhardt,2005), as well as standard anger management approaches that have been found to lead to reductions in IPV perpetration among individuals with PTSD (Chemtob et al., 1997) could be made more accessible and affordable such as via internet, phone or text messaging services (Slakoff et al., 2020). Moreover, when treating individuals with COVID-related PTSD, the associated attachment needs, worries, and doubts need to be taken into consideration. For instance, a therapeutic setting could provide experiences of security which may help individuals re-establish a normal functioning of attachment security.
Conclusion
Violence against intimate partners tends to increase during humanitarian crises and emergencies. Since the onset of COVID-19 and imposed lockdown measures that forced couples into close-proximity, IPV cases have soared world-wide. Attachment styles likely play an important role in how individuals cope with distress. Although secure attachment has been consistently associated with better adjustment in times of need, the findings of the present study add to the existing literature on how persistent stress responses to traumatic events may cumulatively erode healthy attachment functioning. The present study provides additional evidence on the importance of understanding the psychological consequences of COVID-19 on individuals and intimate relationships. Identifying the risk factors that place individuals at an increased risk of IPV perpetration is critical for improving mental health interventions, better enabling psychologists to deal with future crises that require us to help both individuals and their intimate partners stay safe while staying home.
References
Allen-Ebrahimian, B. (2020). China’s domestic violence epidemic. Axios, 10, w26823.
American Psychological Association (2019). Stress in America: Stress and Current Events. Stress in America Survey. https://www.apa.org/news/press/releases/stress/2019/stress-america-2019.pdf
Anderson, C. A., & Bushman, B. J. (2002). Human aggression. Annual Review of Psychology, 53, 27–51.
Arpaci, I., Karataş, K., & Baloğlu, M. (2020). The development and initial tests for the psychometric properties of the COVID-19 Phobia Scale (C19P-S). Personality and Individual Differences, 164, 110108. https://doi.org/10.1016/j.paid.2020.110108
Baldwin, M. W., & Fehr, B. (1995). On the instability of attachment style ratings. Personal Relationships, 2(3), 247–261.
Balzarini, R. N., Muise, A., Zoppolat, G., Di Bartolomeo, A., Rodrigues, D. L., Alonso-Ferres, M., Urganci, B., Debrot, A., Pichayayothin, N. B., Dharma, C., Chi, P., Karremans, J., Schoebi, D., & Slatcher, R. B. (2020). Love in the time of COVID: Perceived partner responsiveness buffers people from lower relationship quality associated with COVID-related stressors. https://doi.org/10.31234/osf.io/e3fh4
Baron, R. A., & Richardson, D. R. (1994). Human aggression (2nd ed.). Plenum.
Beaglehole, B., Mulder, R. T., Frampton, C. M., Boden, J. M., Newton-Howes, G., & Bell, C. J. (2018). Psychological distress and psychiatric disorder after natural disasters: Systematic review and meta-analysis. British Journal of Psychiatry, 213(6), 716–722.
Beck, L. A., Pietromonaco, P. R., DeBuse, C. J., Powers, S. I., & Sayer, A. G. (2013). Spouses’ attachment pairings predict neuroendocrine, behavioral, and psychological responses to marital conflict. Journal of Personality and Social Psychology, 105(3), 388.
Bell, K. M., & Orcutt, H. K. (2009). Posttraumatic stress disorder and male-perpetrated intimate partner violence. Journal of the American Medical Association, 302(5), 562–564. https://doi.org/10.1001/jama.2009.1126
Besser, A., Neria, Y., & Haynes, M. (2009). Adult attachment, perceived stress, and PTSD among civilians exposed to ongoing terrorist attacks in Southern Israel. Personality and Individual Differences, 47(8), 851–857.
Bond, S. B., & Bond, M. (2004). Attachment styles and violence within couples. Journal of Nervous and Mental Disease, 192(12), 857–863.
Bowlby, J. (1969). Attachment and loss (Vol. 1). Random House.
Bowlby, J. (1973). Attachment and loss: Separation: anxiety and anger (Vol. 2). Basic Books.
Bowlby, J. (1982). Attachment and loss: Retrospect and prospect. American Journal of Orthopsychiatry, 52(4), 664.
Bradbury-Jones, C., & Isham, L. (2020). The pandemic paradox: The consequences of COVID-19 on domestic violence. Journal of Clinical Nursing, 29(13–14), 2047–2049. https://doi.org/10.1111/jocn.15296
Brennan, K. A., & Bosson, J. K. (1998). Attachment-style differences in attitudes toward and reactions to feedback from romantic partners: An exploration of the relational bases of self-esteem. Personality and Social Psychology Bulletin, 24(7), 699–714.
Bridgland, V., Moeck, E. K., Green, D. M., Swain, T. L., Nayda, D. M., Matson, L. A., Hutchison, N. P., & Takarangi, M. (2021). Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE, 16(1), e0240146. https://doi.org/10.1371/journal.pone.0240146
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920.
Brosschot, J. F., Verkuil, B., & Thayer, J. F. (2016). The default response to uncertainty and the importance of perceived safety in anxiety and stress: An evolution-theoretical perspective. Journal of Anxiety Disorders, 41, 22–34. https://doi.org/10.1016/j.janxdis.2016.04.012
Brown, G. W., Harris, T. O., & Hepworth, C. (1995). Loss, humiliation and entrapment among women developing depression: A patient and non-patient comparison. Psychological Medicine, 25(1), 7–21. https://doi.org/10.1017/s003329170002804x
Buhrmester, M., Kwang, T., & Gosling, S. D. (2011). Amazon’s mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science, 6(1), 3–5. https://doi.org/10.1177/1745691610393980
Canady, V. A. (2020). Study finds COVID-19 survivors exhibit MH signs one month after treatment. Mental Health Weekly, 30(32), 1–3.
Cano, A., & Vivian, D. (2003). Are life stressors associated with marital violence? Journal of Family Psychology, 17(3), 302–314. https://doi.org/10.1037/0893-3200.17.3.302
Cantor, C. (2009). Post-traumatic stress disorder: Evolutionary perspectives. Australian & New Zealand Journal of Psychiatry, 43(11), 1038–1048.
Capaldi, D. M., & Langhinrichsen-Rohling, J. (2012). Informing intimate partner violence prevention efforts: Dyadic, developmental, and contextual considerations. Prevention Science, 13(4), 323–328.
Carpenter, E. M., & Kirkpatrick, L. A. (1996). Attachment style and presence of a romantic partner as moderators of psychophysiological responses to a stressful laboratory situation. Personal Relationships, 3(4), 351–367.
Carver, C. S., & White, T. L. (1994). Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. Journal of Personality and Social Psychology, 67(2), 319–333.
Casler, K., Bickel, L., & Hackett, E. (2013). Separate but equal? A comparison of participants and data gathered via Amazon’s MTurk, social media, and face-to-face behavioral testing. Computers in Human Behavior, 29(6), 2156–2160.
Chandan, J. S., Taylor, J., Bradbury-Jones, C., Nirantharakumar, K., Kane, E., & Bandyopadhyay, S. (2020). COVID-19: A public health approach to manage domestic violence is needed. The Lancet. Public Health, 5(6), e309. https://doi.org/10.1016/S2468-2667(20)30112-2
Chemtob, C. M., Novaco, R. W., Hamada, R. S., Gross, D. M., & Smith, G. (1997). Anger regulation deficits in combat-related posttraumatic stress disorder. Journal of Traumatic Stress, 10(1), 17–36.
Cooke, J. E., Eirich, R., Racine, N., & Madigan, S. (2020). Prevalence of posttraumatic and general psychological stress during COVID-19: A rapid review and meta-analysis. Psychiatry Research, 292, 113347. https://doi.org/10.1016/j.psychres.2020.113347
Creamer, M., Bell, R., & Failla, S. (2003). Psychometric properties of the impact of event scale—revised. Behaviour Research and Therapy, 41(12), 1489–1496.
Davies, S., & Batha, E. (2020). Europe braces for domestic abuse “perfect storm” amid coronavirus lockdown. Thomas Reuters Foundation News.
Davila, J., & Cobb, R. J. (2004). Predictors of change in attachment security during adulthood. In W. S. Rholes & J. A. Simpson (Eds.), Adult attachment: Theory, research, and clinical implications (pp. 133–156). Guilford Publications.
Dowd, L. S., Leisring, P. A., & Rosenbaum, A. (2005). Partner aggressive women: Characteristics and treatment attrition. Violence and Victims, 20(2), 219–233.
Dutheil, F., Mondillon, L., & Navel, V. (2021). PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychological Medicine, 51(10), 1773–1774.
Field, A. (2013). Discovering statistics using IBM SPSS statistics. Sage.
Finkel, E. J., & Eckhardt, C. I. (2013). Intimate partner violence. In J. A. Simpson & L. Campbell (Eds.), The Oxford handbook of close relationships (pp. 452–474). Oxford University Press.
Forte, G., Favieri, F., Tambelli, R., & Casagrande, M. (2020). COVID-19 pandemic in the Italian population: Validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. International Journal of Environmental Research and Public Health, 17(11), 4151. https://doi.org/10.3390/ijerph17114151
Fraley, R. C., Fazzari, D. A., Bonanno, G. A., & Dekel, S. (2006). Attachment and psychological adaptation in high exposure survivors of the September 11th attack on the World Trade Center. Personality and Social Psychology Bulletin, 32(4), 538–551.
Frye, N. E., & Karney, B. R. (2006). The context of aggressive behavior in marriage: A longitudinal study of newlyweds. Journal of Family Psychology, 20(1), 12.
Galinsky, A., Gruenfeld, D., & Magee, J. (2003). From power to action. Journal of Personality and Social Psychology, 85, 453–466. https://doi.org/10.1037/0022-3514.85.3.453
Gilbar, O., Taft, C., & Dekel, R. (2020). Male intimate partner violence: Examining the roles of childhood trauma, PTSD symptoms, and dominance. Journal of Family Psychology, 34(8), 1004–1013. https://doi.org/10.1037/fam0000669
Gilbert, P., & Allan, S. (1998). The role of defeat and entrapment (arrested flight) in depression: An exploration of an evolutionary view. Psychological Medicine, 28(3), 585–598.
Girme, Y. U., Overall, N. C., Simpson, J. A., & Fletcher, G. J. (2015). “All or nothing”: Attachment avoidance and the curvilinear effects of partner support. Journal of Personality and Social Psychology, 108(3), 450–475. https://doi.org/10.1037/a0038866
González-Sanguino, C., Ausín, B., Castellanos, M. Á., Saiz, J., López-Gómez, A., Ugidos, C., & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity, 87, 172–176. https://doi.org/10.1016/j.bbi.2020.05.040
Gosling, S. D., Vazire, S., Srivastava, S., & John, O. P. (2004). Should we trust Web-based studies? A comparative analysis of six preconceptions about Internet questionnaires. American Psychologist, 59, 93–104.
Hagen, E. H. (1999). The functions of postpartum depression. Evolution and Human Behavior, 20(5), 325–359. https://doi.org/10.1016/S1090-5138(99)00016-1
Hagen, E. H. (2002). Depression as bargaining: The case postpartum. Evolution and Human Behavior, 23(5), 323–336. https://doi.org/10.1016/S1090-5138(01)00102-7
Hagen, E. H., & Thomson, J. A., Jr. (2004). Social navigation hypothesis of depression revisited: Comment. Journal of Affective Disorders, 83(2–3), 285–286. https://doi.org/10.1016/j.jad.2004.08.008
Hamberger, L. K., Larsen, S. E., & Lehrner, A. (2017). Coercive control in intimate partner violence. Aggression and Violent Behavior, 37, 1–11. https://doi.org/10.1016/j.avb.2017.08.003
Hamby, S. L. (1996). The Dominance Scale: Preliminary psychometric properties. Violence and Victims, 11(3), 199–212.
Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Publications.
Henderson, A. J. Z., Bartholomew, K., Trinke, S. J., & Kwong, M. J. (2005). When loving means hurting: An exploration of attachment and intimate abuse in a community sample. Journal of Family Violence, 20(4), 219. https://doi.org/10.1007/s10896-005-5985-y
Higgins, E. T. (1998). Promotion and prevention: Regulatory focus as a motivational principle. In M. P. Zanna (Ed.), Advances in experimental social psychology (Vol. 30, pp. 1–46). Academic Press.
Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine, 41(3), 209–218.
James, P. B., Wardle, J., & Steel, A. (2019). Post-Ebola psychosocial experiences and coping mechanisms among Ebola survivors: A systematic review. Tropical Medicine & International Health, 24(6), 671–691.
Johnson, S. L., Leedom, L. J., & Muhtadie, L. (2012). The dominance behavioral system and psychopathology: Evidence from self-report, observational, and biological studies. Psychological Bulletin, 138(4), 692–743. https://doi.org/10.1037/a0027503
Kawamura, N., Kim, Y., & Asukai, N. (2001). Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. American Journal of Psychiatry, 158(3), 484–486. https://doi.org/10.1176/appi.ajp.158.3.484
Kelly, J., & Morgan, T. (2020). ‘Coronavirus’: Domestic abuse calls up 25% since lockdown, charity says. BBC News.
Keltner, D., Gruenfeld, D. H., & Anderson, C. (2003). Power, approach, and inhibition. Psychological Review, 110(2), 265.
Kennedy, S. (2020). Jobs destroyed worldwide as coronavirus triggers deep recession. The Japan Times. Retrieved on 10th April, 2020 from: https://www.japantimes.co.jp/news/2020/04/06/business/economy‐business/jobs‐destroyed‐worldwide‐coronavirus‐recession/#.XpUVQcgzbD4
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. https://doi.org/10.1001/archpsyc.1995.03950240066012
Kirby, A. C., Beckham, J. C., Calhoun, P. S., Roberts, S. T., Taft, C. T., Elbogen, E. B., & Dennis, M. F. (2012). An examination of general aggression and intimate partner violence in women with posttraumatic stress disorder. Violence and Victims, 27(5), 777–792.
Kowal, M., Coll-Martín, T., Ikizer, G., Rasmussen, J., Eichel, K., Studzinska, A., & Ahmed, O. (2020). Who is the most stressed during COVID-19 isolation? Data from 27 countries.
Langer, A., Lawrence, E., & Barry, R. A. (2008). Using a vulnerability-stress-adaptation framework to predict physical aggression trajectories in newlywed marriage. Journal of Consulting and Clinical Psychology, 76(5), 756–768. https://doi.org/10.1037/a0013254
Langhinrichsen-Rohling, J., Misra, T. A., Selwyn, C., & Rohling, M. L. (2012). Rates of bidirectional versus unidirectional intimate partner violence across samples, sexual orientations, and race/ethnicities: A comprehensive review. Partner Abuse, 3(2), 199–230.
Liu, C. H., Zhang, E., Wong, G., Hyun, S., & Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290, 113172. https://doi.org/10.1016/j.psychres.2020.113172
Magdol, L., Moffitt, T. E., Caspi, A., Newman, D. L., Fagan, J., & Silva, P. A. (1997). Gender differences in partner violence in a birth cohort of 21-year-olds: Bridging the gap between clinical and epidemiological approaches. Journal of Consulting and Clinical Psychology, 65(1), 68–78. https://doi.org/10.1037/0022-006X.65.1.68
Marmet, S., Wicki, M., Gmel, G., Gachoud, C., Daeppen, J. B., Bertholet, N., & Studer, J. (2021). The psychological impact of the COVID-19 crisis is higher among young Swiss men with a lower socioeconomic status: Evidence from a cohort study. PLoS ONE, 16(7), e0255050.
Marshall, E. M., & Kuijer, R. G. (2017). Weathering the storm? The impact of trauma on romantic relationships. Current Opinion in Psychology, 13, 54–59.
Mason, B., & Smithey, M. (2012). The effects of academic and interpersonal stress on dating violence among college students: A test of classical strain theory. Journal of Interpersonal Violence, 27(5), 974–986. https://doi.org/10.1177/0886260511423257
McLaughlin, I. G., Leonard, K. E., & Senchak, M. (1992). Prevalence and distribution of premarital aggression among couples applying for a marriage license. Journal of Family Violence, 7(4), 309–319. https://doi.org/10.1007/BF00994621
McNally, R. J. (2003). Progress and controversy in the study of posttraumatic stress disorder. Annual Review of Psychology, 54, 229–252. https://doi.org/10.1146/annurev.psych.54.101601.145112
Mikulincer, M., & Shaver, P. R. (2011). Attachment, anger, and aggression.
Mikulincer, M., Shaver, P. R., & Solomon, Z. (2015). An attachment perspective on traumatic and posttraumatic reactions. In M. P. Safir, H. S. Wallach, & A. S. Rizzo (Eds.), Future directions in post-traumatic stress disorder (pp. 79–96). Springer.
Mikulincer, M., Birnbaum, G., Woddis, D., & Nachmias, O. (2000). Stress and accessibility of proximity-related thoughts: Exploring the normative and intraindividual components of attachment theory. Journal of Personality and Social Psychology, 78(3), 509–523. https://doi.org/10.1037/0022-3514.78.3.509
Mikulincer, M., Gillath, O., & Shaver, P. R. (2002). Activation of the attachment system in adulthood: Threat-related primes increase the accessibility of mental representations of attachment figures. Journal of Personality and Social Psychology, 83(4), 881.
Mikulincer, M., & Shaver, P. R. (2007). Boosting attachment security to promote mental health, prosocial values, and inter-group tolerance. Psychological Inquiry, 18(3), 139–156.
Mikulincer, M., & Shaver, P. R. (2012). An attachment perspective on psychopathology. World Psychiatry, 11(1), 11–15.
Mikulincer, M., Shaver, P. R., & Pereg, D. (2003). Attachment theory and affect regulation: The dynamics, development, and cognitive consequences of attachment-related strategies. Motivation and Emotion, 27(2), 77–102.
Mikulincer, M., Shaver, P., Solomon, Z., & Ein-Dor, T. (2014). Attachment-related consequences of war captivity and trajectories of posttraumatic stress disorder: A 17-year longitudinal study. Journal of Social and Clinical Psychology, 33, 207–228. https://doi.org/10.1521/jscp.2014.33.3.207
Nesse, R. M. (2002). Evolution and addiction: Comment. Addiction, 97(4), 470–471. https://doi.org/10.1046/j.1360-0443.2002.00086.x
Nettle, D., & Bateson, M. (2012). The evolutionary origins of mood and its disorders. Current Biology, 22(17), R712–R721.
Orth, U., & Wieland, E. (2006). Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: A meta-analysis. Journal of Consulting and Clinical Psychology, 74(4), 698.
Overall, N. C., Girme, Y. U., Lemay, E. P., Jr., & Hammond, M. D. (2014). Attachment anxiety and reactions to relationship threat: The benefits and costs of inducing guilt in romantic partners. Journal of Personality and Social Psychology, 106(2), 235–256. https://doi.org/10.1037/a0034371
Peterman, A., Potts, A., O’Donnell, M., Thompson, K., Shah, N., Oertelt-Prigione, S., & Van Gelder, N. (2020). Pandemics and violence against women and children (Vol. 528). Center for Global Development.
Pietromonaco, P. R., & Beck, L. A. (2015). Attachment processes in adult romantic relationships.
Poate, S. (2020). 75% increase in domestic violence searches since Coronavirus. NBN News. Retrieved on 7th April, 2020 from: https://www.nbnnews.com.au/2020/03/31/dvsearches-coronavirus/
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Resick, P. A., & Schnicke, M. K. (1992). Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology, 60(5), 748.
Roberts, A. L., McLaughlin, K. A., Conron, K. J., & Koenen, K. C. (2011). Adulthood stressors, history of childhood adversity, and risk of perpetration of intimate partner violence. American Journal of Preventive Medicine, 40(2), 128–138. https://doi.org/10.1016/j.amepre.2010.10.016
Roesch, E., Amin, A., Gupta, J., & García-Moreno, C. (2020). Violence against women during covid-19 pandemic restrictions. British Medical Journal (clinical Research Ed.), 369, m1712. https://doi.org/10.1136/bmj.m1712
Rosenbaum, A., & Leisring, P. A. (2003). Beyond power and control: Towards an understanding of partner abusive men. Journal of Comparative Family Studies, 34(1), 7–22.
Rubin, G. J., & Wessely, S. (2020). The psychological effects of quarantining a city. British Medical Journal, 368.
Schumacher, J. A., Feldbau-Kohn, S., Slep, A. M. S., & Heyman, R. E. (2001). Risk factors for male-to-female partner physical abuse. Aggression and Violent Behavior, 6(2–3), 281–352. https://doi.org/10.1016/S1359-1789(00)00027-6
Shallcross, S. L., Howland, M., Bemis, J., Simpson, J. A., & Frazier, P. (2011). Not “capitalizing” on social capitalization interactions: The role of attachment insecurity. Journal of Family Psychology, 25(1), 77.
Shaver, P. R., & Mikulincer, M. (2002). Attachment-related psychodynamics. Attachment & Human Development, 4(2), 133–161. https://doi.org/10.1080/14616730210154171
Shigemura, J., Ursano, R. J., Morganstein, J. C., Kurosawa, M., & Benedek, D. M. (2020). Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences, 74(4), 281.
Shorey, R. C., McNulty, J. K., Moore, T. M., & Stuart, G. L. (2015). Emotion regulation moderates the association between proximal negative affect and intimate partner violence perpetration. Prevention Science, 16(6), 873–880.
Simpson, J. A., & Rholes, W. S. (2017). Adult attachment, stress, and romantic relationships. Current Opinion in Psychology, 13, 19–24. https://doi.org/10.1016/j.copsyc.2016.04.006
Simpson, J. A., Rholes, W. S., & Nelligan, J. S. (1992). Support seeking and support giving within couples in an anxiety-provoking situation: The role of attachment styles. Journal of Personality and Social Psychology, 62(3), 434.
Slakoff, D. C., Aujla, W., & PenzeyMoog, E. (2020). The role of service providers, technology, and mass media when home isn’t safe for intimate partner violence victims: Best practices and recommendations in the era of CoViD-19 and beyond. Archives of Sexual Behavior, 49(8), 2779–2788.
Stark, L., & Ager, A. (2011). A systematic review of prevalence studies of gender-based violence in complex emergencies. Trauma, Violence & Abuse, 12(3), 127–134. https://doi.org/10.1177/1524838011404252
Stith, S. M., Smith, D. B., Penn, C. E., Ward, D. B., & Tritt, D. (2004). Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggression and Violent Behavior, 10(1), 65–98.
Straus, M. A. (2008). Dominance and symmetry in partner violence by male and female university students in 32 nations. Children and Youth Services Review, 30(3), 252–275.
Straus, M. A., Hamby, S. L., Boney-McCoy, S., & Sugarman, D. B. (1996). The Revised Conflict Tactics Scale (CTS2): Development and preliminary psychometric data. Journal of Family Issues, 17(3), 283–316. https://doi.org/10.1177/019251396017003001
Sun, L., Sun, Z., Wu, L., Zhu, Z., Zhang, F., Shang, Z., Jia, Y., Gu, J., Zhou, Y., Wang, Y., Liu, N., & Liu, W. (2021). Prevalence and risk factors acute posttraumatic stress disorder during the COVID-19 Outbreak. medRxiv, 2020.2003.2006.20032425. https://doi.org/10.1101/2020.03.06.20032425
Swan, S. C., Gambone, L. J., Fields, A. M., Sullivan, T. P., & Snow, D. L. (2005). Women who use violence in intimate relationships: The role of anger, victimization, and symptoms of posttraumatic stress and depression. Violence and Victims, 20(3), 267–285. https://doi.org/10.1891/vivi.20.3.267
Taft, C. T., Macdonald, A., Creech, S. K., Monson, C. M., & Murphy, C. M. (2016). A randomized controlled clinical trial of the Strength at Home Men’s Program for partner violence in military veterans. Journal of Clinical Psychiatry, 77(9), 20066.
Taft, C. T., Watkins, L. E., Stafford, J., Street, A. E., & Monson, C. M. (2011). Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology, 79(1), 22–33. https://doi.org/10.1037/a0022196
Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., Xie, C., Chen, S., & Xu, J. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders. https://doi.org/10.1016/j.jad.2020.05.009
Taylor, S., Landry, C. A., Paluszek, M. M., Fergus, T. A., McKay, D., & Asmundson, G. J. (2020). COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety, 37(8), 706–714.
van Gelder, N., Peterman, A., Potts, A., O’Donnell, M., Thompson, K., Shah, N., Oertelt-Prigione, S., Gender and COVID-19 working group. (2020). COVID-19: Reducing the risk of infection might increase the risk of intimate partner violence. EClinicalMedicine, 21, 100348. https://doi.org/10.1016/j.eclinm.2020.100348
Vanaken, L., Scheveneels, S., Belmans, E., & Hermans, D. (2020). Validation of the Impact Event Scale with modifications for COVID-19 (IES-COVID19). Frontiers in Psychiatry, 11, 738.
Voith, L. A., Logan-Greene, P., Strodthoff, T., & Bender, A. E. (2020). A paradigm shift in batterer intervention programming: A need to address unresolved trauma. Trauma, Violence, & Abuse, 21(4), 691–705.
Wagers, S. (2020). Domestic violence growing in wake of coronavirus outbreak. The Conversation. Retrieved on 10th April, 2020 from: https://theconversation.com/domestic‐violence‐growing‐in‐wake‐of‐coronavirus‐outbreak‐135598
Wang, S., Kamerāde, D., Bessa, I., Burchell, B., Gifford, J., Green, M., & Rubery, J. (2022). The impact of reduced working hours and furlough policies on workers’ mental health at the onset of COVID-19 pandemic: A longitudinal study. Journal of Social Policy, 1–25.
Watson, P. J., & Andrews, P. W. (2002). Toward a revised evolutionary adaptationist analysis of depression: The social navigation hypothesis. Journal of Affective Disorders. https://doi.org/10.1017/S0047279422000599
Weiss, D. S., & Marmar, C. R. (1997). The Impact of Event Scale-Revised. In J. P. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399-411). The Guilford Press.
Whitaker, D. J., Murphy, C. M., Eckhardt, C. I., Hodges, A. E., & Cowart, M. (2013). Effectiveness of primary prevention efforts for intimate partner violence. Partner Abuse, 4(2), 175–195.
World Health Organization. (2020). COVID-19 and violence against women: what the health sector/system can do, 7 April 2020 (No. WHO/SRH/20.04). World Health Organization.
Yaribeygi, H., Panahi, Y., Sahraei, H., Johnston, T. P., & Sahebkar, A. (2017). The impact of stress on body function: A review. EXCLI Journal, 16, 1057–1072. https://doi.org/10.17179/excli2017-480
Zhang, L., Pan, R., Cai, Y., & Pan, J. (2021). The prevalence of post-traumatic stress disorder in the general population during the COVID-19 pandemic: A systematic review and single-arm meta-analysis. Psychiatry Investigation, 18(5), 426.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
David Schmitt serves as scientific advisor for Dionysus Digital Health, Inc. and holds shares of this company.
Ethical Approval
We have complied with ethical standards regarding the treatment of human subjects and reporting of results in this article.
Informed consent
Informed consent was obtained from all participants included in the study.
Editor’s note
This paper was to be part of the Special Section on the Impact of COVID-19 on Sexual Health and Behavior (Guest-Edited By Lori A. J. Scott-Sheldon, Kristen P. Mark, Rhonda N. Balzarini, and Lisa L. M. Welling), which was published in the January 2022 issue of the Journal. Unfortunately, the paper was not accepted for publication until after the January 2022 issue went to press.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gottlieb, L., Schmitt, D.P. When Staying Home Is Not Safe: An Investigation of the Role of Attachment Style on Stress and Intimate Partner Violence in the Time of COVID-19. Arch Sex Behav 52, 639–654 (2023). https://doi.org/10.1007/s10508-022-02457-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-022-02457-7