Abstract
Corynebacterium striatum is an emerging, multidrug-resistant pathogen that frequently causes nosocomial infections worldwide. This study aimed to investigate phylogenetic relationship and presence of genes responsible for antimicrobial resistance among C. striatum strains associated with an outbreak at the Shanxi Bethune Hospital, China, in 2021. Fecal samples were collected from 65 patients with C. striatum infection at Shanxi Bethune Hospital between February 12, 2021 and April 12, 2021. C. striatum isolates were identified by 16S rRNA and rpoB gene sequencing. E-test strips were used to examine the antimicrobial susceptibility of the isolates. Whole-genome sequencing and bioinformatics analysis were employed to assess the genomic features and identify antimicrobial resistance genes of the isolates. Crystal violet staining was conducted to determine the ability of biofilm formation of each isolate. A total of 64 C. striatum isolates were identified and categorized into 4 clades based on single nucleotide polymorphisms. All isolates were resistant to penicillin, meropenem, ceftriaxone, and ciprofloxacin but susceptible to vancomycin and linezolid. Most isolates were also resistant to tetracycline, clindamycin, and erythromycin, with susceptibility rates of 10.77, 4.62, and 7.69%, respectively. Genomic analysis revealed 14 antimicrobial resistance genes in the isolates, including tetW, ermX, and sul1. Crystal violet staining showed that all isolates formed biofilms on the abiotic surface. Four clades of multidrug-resistant C. striatum spread in our hospitals possibly due to the acquisition of antimicrobial resistance genes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Corynebacterium striatum is a Gram-positive, normal constituent of the microbiota of human skin and nasal mucosa, and thus has been considered a contaminant of clinical specimens(Lee et al. 2005; Bernard et al. 2013). However, a larger number of invasive infections by C. striatum have emerged worldwide in the last five decades (Campanile et al. 2009; Martins et al. 2009; Wong et al. 2010). According to a recent review, a total of 254 cases of C. striatum human infections and nosocomial outbreaks have occurred since 1976 (Silva-Santana et al. 2021), affecting both immunosuppressive and immunocompetent individuals(Verma and Kravitz 2016; Lee et al. 2018; Ramos et al. 2019). Nosocomial outbreaks and antibiotic treatment failure of C. striatum infection are associated with the resistance of C. striatum to multiple antimicrobial agents(Renom et al. 2007). Earlier studies have shown that C. striatum isolates were susceptible to many antimicrobial drugs, including tetracycline, β-lactams, and fluoroquinolones(Soriano et al. 1995; Martinez-Martinez et al. 1997; Lagrou et al. 1998). However, more recent reports have indicated increasing multidrug resistance of C. striatum strains(Verroken et al. 2014; Yoo et al. 2015; Werth et al. 2016), resulting a mortality rate of nearly 20% in patients with C. striatum invasive infection as well as recurrence, superinfection, and limb amputation in many survived patients (Milosavljevic et al. 2021). Thus, it is critically important to unveil the multidrug-resistance mechanisms of C. striatum.
Genomic determinants are associated with antimicrobial resistance of C. striatum. Horizontal gene transfer plays an essential role in the dissemination of antimicrobial resistance genes within C. striatum associated with mobile genomic elements such as plasmids, transposons and insertion sequences(Leyton et al. 2021). For example, ermX transported by transposon Tn5432 is associated with the resistance of C. striatum to macrolides, lincosamides, and streptogramin(Tauch et al. 2000). Plasmid pJA144188 and insertion sequences IS3502, IS3503, and IS3504 can transport tetW that confers tetracycline resistance(Schroder et al. 2012; Nudel et al. 2018; Wang et al. 2019). Whole-genome sequencing compared with those available in the GenBank database is more accurate method for the identification of C. striatum compared with MALDI-TOF, Vitek 2 and API (Milosavljevic et al. 2021). When combined with bioinformatics analysis, whole-genome sequencing serves as a powerful tool to understand the genomic features and track nosocomial transmission of pathogens(Quainoo et al. 2017). Genomic analysis has revealed that the acquisition of antimicrobial resistance genes through genetic transfer contributes to C. striatum hospital infections(Alibi et al. 2017; Wang et al. 2019). In addition, C. striatum strains can form biofilms on abiotic substrates, including indwelling medical devices and steel surfaces, thus facilitating the tolerance of C. striatum to disinfectants and antiseptics agents(Souza et al. 2015; Souza et al. 2020). Therefore, identification of antimicrobial resistance genes and examination of the biofilm-forming ability of C. striatum strains may help elucidate the multidrug-resistance mechanisms of C. striatum.
In this study, we investigated the genomic diversity and the multidrug resistance mechanism of C. striatum that caused a nosocomial outbreak at Shanxi Bethune Hospital, China, in 2021. Our results may provide valuable information for the prevention and management of C. striatum infection in the hospital.
Materials and methods
Study design and ethical approval
This study was approved by the local medical ethical committee (YXLL-KY-2021–015; Shanxi, China). All experiments were performed following relevant regulations. Fecal samples were obtained from 65 patients infected with C. striatum. Patients were admitted to Shanxi Bethune Hospital from February 12, 2021 to April 12, 2021. The inclusion criteria were: (1) patients stayed in the hospital at least 3 days; (2) patients showed clinical symptoms of respiratory or urinary tract infection or had pain, redness, or swelling around the insertion site of venous catheter; (3) the sputum or bronchial aspirate specimen contained ≥ 25 white blood cells/high-power filed and the number of C. striatum clones isolated from sputum ≥ 106 CFU/ml in quantitative sputum culture. (4) the urine sample contained > 5 white blood cells/ high-power filed and the number of C. striatum clones isolated from urine ≥ 104 CFU/ml in quantitative urine culture (5) the number of C. striatum clones isolated from venous catheter ≥ 15 CFU/5 cm.
Isolation and identification of C. striatum
Clinical specimens were inoculated on agar plates (Autobio Diagnostics, Zhengzhou, Henan, China) and cultured at 35 °C for 24–72 h in an atmosphere of 5% CO2. Genomic DNA was isolated from the colonies using a Gentra Puregene Yeast/Bact Kit (Qiaqen, Hilden, Germany) according to the manufacturer’s instruction. The quality of genomic DNA was assessed by electrophoresis on 1% agarose gels and OD 260/280 ratio. The DNA concentration was measured using a Qubit® DNA assay kit (Invitrogen, Waltham, MA, USA). All isolates were initially identified as C. striatum by MALDI-TOF using the Microflex LT/SH MS system (Bruker Daltonics, Bremen, Germany) in IVD HCCA solution, followed by 16 s rRNA sequencing (Novogene, Beijing, China) and PCR amplification of rpoB encoding RNA polymerase β subunit. The 16 s rRNA sequencing results were aligned to the complete genomic sequence of C. striatum in NCBI (https://www.ncbi.nlm.nih.gov/) using the BLAST algorithm and the Ribosomal Database Project II (http://rdp.cme.msu.edu/). All the isolates were confirmed as C. striatum with similarity ≥ 99%. PCR amplification of rpoB was conducted on a Mastercycler® nexus thermal cycler (Eppendorf, Hamburg, Germany) using primers 5´-CGTATGAACATYGGBCAGGT-3ʹ (forward) and 5ʹ -TCCATYTCRCCRAARCGCTG-3ʹ (reverse) (Sangon Biotech, Shanghai, China). The thermal cycles were 94 °C for 5 min, 30 cycles of 90 °C for 30 s, 64 °C for 30 s, and 72 °C for 1 min, followed by 72 °C for 2 min. The rpoB sequence of each isolate was aligned to the rpoB sequence of C. striatum in the GenBank database. All the isolates were confirmed as C. striatum with similarities ≥ 99%.
Whole-genome sequencing
A total of 0.2 μg DNA per sample was used to prepare the DNA library. The sequencing library was generated using NEB Next® Ultra™ DNA library prep kit for Illumina (New England Biolabs, Ipswich, MA, USA) following the manufacturer’s instructions. The index codes were added to each sample. Briefly, genomic DNA was sonicated into fragments of 350 bp. Then, DNA fragments were end-polished, A-tailed, and ligated with the full-length adapter for Illumina sequencing, followed by PCR amplification. The PCR products were purified by the AMPure XP system (Beckman Coulter, Beverly, USA), and the DNA concentration was measured using a Qubit®3.0 flurometer (Invitrogen). The DNA library was analyzed for size distribution using Agilent 2100 Bioanalyzer (Agilent, Santa Clara, CA, USA) and quantified by real-time PCR (> 2 nM). The clustering of the index-coded samples was performed on a cBot cluster generation system using Illumina PE cluster kit (Illumina, USA) according to the manufacturer’s instructions. Then, the DNA library was sequenced on the Illumina platform to generate 150 bp paired-end reads.
Phylogenetic analysis
A single nucleotide polymorphism (SNP)-based phylogenetic analysis was performed using the whole genome sequence of C. striatum RefCP021252 as the reference. The Trimmomatic software31 was used to filter low-quality reads before SNP extraction. The clean reads of the isolates were aligned to the reference genome using SPAdes software (http://bioinf.spbau.ru/en/spades) under the default parameters. The Snippy pipeline, version 3.0 (https://github.com/tseemann/snippy), was used for read mapping and variant calling. SNPs were identified to reveal the phylogenomic relationship of C. striatum isolates using CSI Phylogeny as previously described(Kaas et al. 2014; Ahrenfeldt et al. 2017). The Z-score cutoff value was 1.96. SNPs within 10 base pairs were removed. A maximum likelihood tree was generated by MEGA Software (Kumar et al. 1994). A phylogenetic test was conducted using the assembled contigs from the root strain as reference genome, SNP pruning disabled(Efron et al. 1996).
Identification of antimicrobial resistance genes
Clean reads from whole-genome sequencing were obtained by removing the adapters, the reads with unknown bases > 10%, and the reads with low-quality bases (Q-value < 5) > 50% using the Trimmomatic Software(Bolger et al. 2014), followed by assembly using SPAdes(Bankevich et al. 2012). Antimicrobial resistance genes were identified using the Center for Genomic Epidemiology server (http://www.genomicepidemiology.org/) (Hendriksen et al. 2019). An antimicrobial resistance gene was considered present in the isolate when the sequence exhibited ≥ 99.9% identity to that in the GeneBank (www.ncbi.nlm.nih.gov/genbank/). A heatmap of the antimicrobial resistance genes was generated using the R pheatmap package.
Antimicrobial susceptibility test
Antimicrobial susceptibility was determined using E-test strips in Mueller–Hinton agar plates (Autobio Diagnostics, Zhengzhou, Henan, China) as previously described(Ramos et al. 2019). E-test strips containing penicillin, meropenem, ceftriaxone, tetracycline, ciprofloxacin, clindamycin, erythromycin, gentamicin, and vancomycin were from Autobio Diagnostics. E-test strips containing rifampicin and linezolid were from Beijing Weitaike Biotechnology (Beijing, China). The plates were incubated at 37 °C in an atmosphere of 5% CO2 for 24 h. The minimum inhibitory concentration (MIC) was determined and interpreted according to The Clinical and Laboratory Standards Institute (CLSI) M45 guidelines (JA Hindler 2016).
Semiquantitative analysis of biofilm formation
Ten microliter of 0.5 McFarland bacterial suspension was plated in 200 uL trypticase soy broth (Sangon Biotech) in a 96-well plate and cultured for 24 h at 37°C. After removing the broth, the adherent bacteria (biofilms) were washed with ice-cold phosphate-buffered saline, fixed with 200 μL methanol for 15 min, and stained with 200 μL 0.1% crystal violet (Sangon Biotech) for 5 min. The absorbance (OD value) was determined at 595 nm. The experiment was performed in quadruplets. Trypticase soy broth was used as a negative control.
Statistical analysis
Categorical data were expressed as percentages. Data were analyzed using SPSS 26 (Armonk, NY, USA). Quantitative data were expressed as the mean ± standard deviation. The differences between the two groups were compared using one-way analysis of variance and Chi-square test. A P value < 0.05 was considered statistically significant.
Results
Identification of C. striatum isolates
A total of 64 C. striatum isolates were obtained from 65 patients infected with C. striatum, including 18 (27.69%) females and 47 (72.31%) males predominantly aged between 51 and 79 years (75.38%). The clinical features of the patients were summarized in Table 1. The presence of C. striatum was mainly confirmed in sputum specimens (51/78.46%), followed by bronchial aspirate (9/13.84%), venous catheter (2/3.08%), wound secretion (2/3.08%), and urine (1/1.54%) specimens. The isolates were from 9 wards, with neurosurgery wards (30/47.68%), intensive care units (9/13.85%), and general medicine wards (8/12.31%) representing the most common locations. The most common preexisting conditions of the patients were cerebral hemorrhage (44/67.69%), hypertension (32/49.23%), and pulmonary inflammation (32/49.23%). All patients received at least one type of antibiotic treatment. Of these, 23 (35.38%) received two types of antibiotics, and 27 (41.54%) received three or more types of antibiotics. In addition, ward distribution and strain acquisition time of C. striatum infection were shown in supplementary table 1. These results suggest that males, patients with critical underlying conditions, patients exposed to multiple antibiotics and patients over 50 years old were higher proportion compared with counterparts.
Phylogenetic analysis
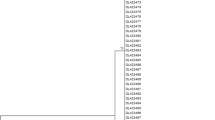
To characterize the genomic diversity of the C. striatum isolates, we performed an SNP-based phylogenetic analysis. As shown in Fig. 1, the isolates were clustered into four clades compared with the referenc genome (RefCP021252), with clade I containing the highest number of isolates (n = 20), followed by clade II, IV, and III containg 18, 15, and 11 isolates, respectively. Of the 64 isolates, isolate 62 showed the greatest evolution. Clade III exhibited the greatest diversity compared with other clades. Furthermore, clades I and III circulted in 6 wards, whereas clades II and IV circulated in 4 wards. The neurosurgery ward was the only ward that contained all the 4 clades and was the main ward in clade I (Supplementary table2). In addition, we conducted the correlation analysis between gene clades and the neurosurgery ward. Nevertheless, the result was negative (Supplementary table3). A long-term multicenter investigation is urgent in the future.
Phylogenomic analysis of C. striatum isolates. Phylogenomic analysis was performed using CSI Phylogeny. The assembled contigs from the root strain was uesd as reference genome, SNP pruning disabled. C. striatum CP021252 was used as the reference sequence. Clades I (n = 20), II (n = 18), III (n = 11), and IV (n = 15) are indicated in black, red, blue, and green, respectively. csy: C. striatum obtained from steriles amples; csn: C. striatum obtained from non-sterile samples. (Color figure online)
Antimicrobial susceptibility testing
To assess the antibiotic resistance of the isolates, we determined the antimicrobial susceptibility. All isolates were resistant to penicillin, meropenem, ceftriaxone, and ciprofloxacin but susceptible to vancomycin and linezolid. Most isolates were also resistant to tetracycline, clindamycin, and erythromycin, with susceptibility rates of 10.77, 4.62, and 7.69%, respectively. However, most isolates were susceptible to gentamicin and rifampicin, with susceptibility rates of 75.38 and 96.92%, respectively. The MICs and susceptibility rates were summarized in Table 2. These results indicate that the C. striatum isolates in this study are resistant to multiple antibiotics. Vancomycin and linezolid are the antibiotics of choice for the treatment of C. striatum infections.
Identification of antimicrobial resistance genes
To investigate the underlying mechanism of antibiotic resistance of the isolates, we sought to identify antimicrobial resistance genes. Genomic analysis revealed 14 antimicrobial resistance genes in the isolates (Fig. 2). Of these genes, APH(3ʹ)-Via was only present in csn-61 isolate. ErmB, tet32 and RlmAII were only present in csn-32 isolate. TetW was present in 59 isolates, followed by ermX in 52 isolates, sul1 in 45 isolates. TetW conferring resistance to tetracycline was the most frequent (Hahn et al. 2016), followed by ermX conferring resistance to erythromycin and clindamycin(Campanile et al. 2009), sul1 conferring resistance to sulfamethoxazole (Yao et al. 2020), aac(6ʹ)-Ia, ant (3″)-IIa, aph(3')-Ia, and aph(3')-Ib conferring resistance to aminoglycosides(Miro et al. 2013; Nie et al. 2014), tetA conferring resistance to tetracycline(Nguyen et al. 1983), cmx conferring resistance to chloramphenicol and lincomycin(Peterson and Kaur 2018), and aph(6)-Id conferring resistance to streptomycin(Ashenafi et al. 2014). Besides, we observed the presence of aph(3)-VIa, tet32, and ErmB conferring resistance to streptomycin, tetracycline, and erythromycin in isolate 32 as well as RImAII conferring resistance to tylosin(Liu and Douthwaite 2002)in isolate 61. Overall, 61 (93.8%) of the isolates contained more than five antibiotic-resistance genes (Supplementary table2). These results suggest that the C. striatum isolates evolve to multidrug-resistant clones by acquiring antimicrobial resistance genes. We also discovered csn-14 and csn-19 isolates in clades II contained ten identical antimicrobial resistance genes; isolates csn-4, csn-16 and csn-59 contained the same ermX in clade III (Supplementary table2). The correlation analysis between gene clades and numbers of antimicrobial resistance genes was conducted (P < 0.05). It was potential of different patterns that these genes distributed among four different clades (Supplementary table3). Isolates csn-7, csn-8 and csn-10 from neurosurgery ward contained seven identical antimicrobial resistance genes. This discovery implicated small clonal circulations in our hospital.
Heatmap of antimicrobial resistance genes in C. striatum isolates. Antimicrobial resistance genes were identified using the Center for Genomic Epidemiology server (http://www.genomicepidemiology.org) based on whole-genome analysis. A heatmap was generated to illustrate antimicrobial resistance genes in each isolate. Red (1) indicates the presence of antimicrobial resistance genes; blue (0) indicates the absence of antimicrobial resistance genes. The vertical axis represents antimicrobial resistance genes. The horizontal axis represents C. striatum isolates. csy: C. striatum obtained from sterile samples; csn: C. striatum obtained from non-sterile samples. (Color figure online)
Semiquantitative analysis of biofilm formation
Considering the critical contribution of bacterial biofilms to antibiotic resistance(Sharma et al. 2019), we determined the biofilm formation of the isolates. Crystal violet staining showed that all isolates formed biofilms with OD values ranging from 0.14 to 0.67 (Fig. 3). We divided all strains into two groups according to OD value of biofilms (< 0.35 or ≥ 0.35) and explored if gene clades was associated with biofilm-forming ability of the isolates. As a pity, the result was negative (Supplementary table3). This requires the advanced method of biofilm detection and expansion the size of the study.
Semiquantitative analysis of biofilm formation. Ten microliters of 0.5 McFarland C. striatum suspension was incubated in 200 uL trypticase soy broth in a 96-well plate for 24 h at 37 °C. Crystal violet staining was performed, and the absorbance (OD value) was measured at 595 nm to determine biofilm formation. Trypticase soy broth was used as a negative control. Black, blue, brown, and red branches indicate four clades. The length of the blue horizontal column indicates the OD value shown alongside. (Color figure online)
Discussion
In this study, we obtained 64 C. striatum isolates from 65 patients with C. striatum infection in a tertiary hospital in China. Sample 63 was excluded due to inadequate amounts of DNA (< 200 ng/uL) for subsequent analysis. SNP-based phylogenetic analysis categorized the isolates into 4 clades. Antimicrobial susceptibility test revealed that the isolates were resistant to multiple antibiotics due to the presence of antimicrobial resistance genes. The distribution pattern of antibiotic-resistance genes was different among 4 clades. Three isolates shared the same genetic background in neurosurgery and two isolates with ten identical antimicrobial resistance genes belonged to clade II. A circulation of single-clone probably existed in our hospital. Therefore, a comprehensive infection control measure is urgent in the future.
C. striatum isolates have been frequently reported in sputum and bronchial aspirate(Hahn et al. 2016; Wang et al. 2019). Consistently, in this study, the presence of C. striatum was mainly confirmed in sputum specimens (51/78.46%) and bronchial aspirate (9/13.84%). Recently, bloodstream and catheter-related C. striatum infections have attracted attention due to the increased number of cases(Ramos et al. 2019; Souza et al. 2019). Indeed, we also obtained C. striatum isolates from the venous catheter (2/3.08%), possibly resulting from the biofilm-forming ability of the isolates on abiotic surfaces(Souza et al. 2019). Studies have demonstrated that most C. striatum infections occur in immunocompromised patients and patients with underlying medical problems or skin damage(Superti et al. 2009; Diez-Aguilar et al. 2013). Invasive medical devices, long-term exposure to broad-spectrum antibiotics, and long-term hospitalization are also risk factors for C. striatum infections(Lee et al. 2005). Similarly, our results showed that males (72.3%), elderly patients over 50 years old (86.2%), patients in the neurosurgery ward, patients with cerebral hemorrhage (67.7%), and those receiving at least two antibiotics (76.9%) were more likely to develop C. striatum infection compared with their counterparts (Supplementary table4). Thus, a standard surveillance program for these patients is recommended for the prevention and early diagnosis of C. striatum infections.
Studies have shown that C. striatum isolates are resistant to penicillin, meropenem, ceftriaxone, tetracycline, clindamycin, erythromycin, and ciprofloxacin(Hahn et al. 2016; McMullen et al. 2017). Consistently, all isolates in this study were resistant to penicillin, meropenem, ceftriaxone, and ciprofloxacin. Most isolates were also resistant to tetracycline, clindamycin, and erythromycin, with susceptibility rates of 10.77%, 4.62%, and 7.69%, respectively. However, despite the resistance to multiple antibiotics, C. striatum isolates in this study were susceptible to vancomycin, linezolid, gentamicin, and rifampicin, with susceptibility rates of 100%, 100%, 75.38%, and 96.92%, respectively, consistent with previous findings(Navas et al. 2016; Alibi et al. 2017). Therefore, vancomycin and linezolid are the antibiotics of choice for the treatment of C. striatum infections, sometimes in combination with other antibiotics such as gentamicin (Rufael and Cohn 1994; Marull and Casares 2008).
C. striatum may evolve into persistent and dominant clones within the hospital by acquiring antimicrobial resistance genes(Wang et al. 2019; Wang et al. 2021). Our genomic analysis identified 14 antimicrobial resistance genes in the isolates. Of these genes, tetW, ermX, sul1, aac(6ʹ)-Ia, and ant (3″)-IIa were expressed in more than 75% of the isolates, suggesting that resistance to antimicrobials may be acquired by horizontal gene transfer within the hospital. In addition, 61 (93.8%) isolates carried at least 5 antimicrobial resistance genes, explaining the resistance of the isolates to multiple antibiotics.
The ability of biofilm formation allows C. striatum to adhere to living and artificial surfaces to resist antibiotics and host immune factors, playing an important role in the virulence potential of C. striatum(Souza et al. 2019). Multidrug-resistant C. striatum strains exhibit greater abilities to adhere to both hydrophilic and hydrophobic abiotic surfaces than multidrug-sensitive counterparts(Souza et al. 2015), suggesting that biofilm production contribute to multidrug resistance of C. striatum. All the 64 C. striatum isolates in this study formed biofilms on the abiotic surface, suggesting that C. striatum isolates were resistant to multiple antibiotics at least partially due to the biofilm-forming ability of the isolates.
This study has some limitations that will be addressed in the future. First, the presence of antimicrobial resistance genes needs to be verified using molecular methods such as PCR. Second, scanning electron microscopy will be employed to demonstrate the production of biofilms.
Conclusion
In conclusion, four clades of multidrug-resistant C. striatum spread at our hospital between February and April 2021. Horizontal transfer of antimicrobial resistance genes and the ability of biofilm formation are likely responsible for the transmission of C. striatum in the hospital. These findings may provide helpful information about the prevention and treatment of nosocomial outbreak of C. striatum. The raw sequence data reported in this paper have been deposited in the Genome Sequence Archive (Genomics, Proteomics & Bioinformatics 2021) in National Genomics Data Center (Nucleic Acids Res 2022), China National Center for Bioinformation / Beijing Institute of Genomics, Chinese Academy of Sciences (GSA: CRA008854) that are publicly accessible at https://ngdc.cncb.ac.cn/gsa.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ahrenfeldt J, Skaarup C, Hasman H, Pedersen AG, Aarestrup FM, Lund O (2017) Bacterial whole genome-based phylogeny: construction of a new benchmarking dataset and assessment of some existing methods. BMC Genom 18:19. https://doi.org/10.1186/s12864-016-3407-6
Alibi S et al (2017) Occurrence of Corynebacterium striatum as an emerging antibiotic-resistant nosocomial pathogen in a Tunisian hospital. Sci Rep 7:9704. https://doi.org/10.1038/s41598-017-10081-y
Ashenafi M, Ammosova T, Nekhai S, Byrnes WM (2014) Purification and characterization of aminoglycoside phosphotransferase APH(6)-Id, a streptomycin-inactivating enzyme. Mol Cell Biochem 387:207–216. https://doi.org/10.1007/s11010-013-1886-1
Bankevich A et al (2012) SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol 19:455–477. https://doi.org/10.1089/cmb.2012.0021
Bernard K, Pacheco AL, Cunningham I, Gill N, Burdz T, Wiebe D (2013) Emendation of the description of the species Corynebacterium propinquum to include strains which produce urease. Int J Syst Evol Microbiol 63:2146–2154. https://doi.org/10.1099/ijs.0.046979-0
Bolger AM, Lohse M, Usadel B (2014) Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30:2114–2120. https://doi.org/10.1093/bioinformatics/btu170
Campanile F et al (2009) Clonal multidrug-resistant Corynebacterium striatum strains, Italy. Emerg Infect Dis 15:75–78. https://doi.org/10.3201/eid1501.080804
Diez-Aguilar M et al (2013) Non-diphtheriae Corynebacterium species: an emerging respiratory pathogen. Eur J Clin Microbiol Infect Dis 32:769–772. https://doi.org/10.1007/s10096-012-1805-5
Efron B, Halloran E, Holmes S (1996) Bootstrap confidence levels for phylogenetic trees. Proc Natl Acad Sci USA 93:13429–13434. https://doi.org/10.1073/pnas.93.23.13429
Hahn WO, Werth BJ, Butler-Wu SM, Rakita RM (2016) Multidrug-resistant Corynebacterium striatum associated with increased use of parenteral antimicrobial drugs. Emerg Infect Dis. https://doi.org/10.3201/eid2211.160141
Hendriksen RS, Bortolaia V, Tate H, Tyson GH, Aarestrup FM, McDermott PF (2019) Using genomics to track global antimicrobial resistance. Front Public Health 7:242. https://doi.org/10.3389/fpubh.2019.00242
Hindler JA (2016) Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria, 3rd edn. CLSI guideline Clinical and Laboratory Standards Institute
Kaas RS, Leekitcharoenphon P, Aarestrup FM, Lund O (2014) Solving the problem of comparing whole bacterial genomes across different sequencing platforms. PLoS ONE 9:e104984. https://doi.org/10.1371/journal.pone.0104984
Kumar S, Tamura K, Nei M (1994) MEGA: Molecular evolutionary genetics analysis software for microcomputers. Comput Appl Biosci 10:189–191. https://doi.org/10.1093/bioinformatics/10.2.189
Lagrou K, Verhaegen J, Janssens M, Wauters G, Verbist L (1998) Prospective study of catalase-positive coryneform organisms in clinical specimens: identification, clinical relevance, and antibiotic susceptibility. Diagn Microbiol Infect Dis 30:7–15. https://doi.org/10.1016/s0732-8893(97)00193-4
Lee PP, Ferguson DA Jr, Sarubbi FA (2005) Corynebacterium striatum : an underappreciated community and nosocomial pathogen. J Infect 50:338–343. https://doi.org/10.1016/j.jinf.2004.05.005
Lee JY, Lee SH, Kim WH (2018) Three-valve endocarditis caused by Corynebacterium striatum. Korean Circ J 48:861–862. https://doi.org/10.4070/kcj.2018.0126
Leyton B et al (2021) Treat me well or will resist: uptake of mobile genetic elements determine the resistome of Corynebacterium striatum. Int J Mol Sci. https://doi.org/10.3390/ijms22147499
Liu M, Douthwaite S (2002) Resistance to the macrolide antibiotic tylosin is conferred by single methylations at 23S rRNA nucleotides G748 and A2058 acting in synergy. Proc Natl Acad Sci U S A 99:14658–14663. https://doi.org/10.1073/pnas.232580599
Martinez-Martinez L, Suarez AI, Rodriguez-Bano J, Bernard K, Muniain MA (1997) Clinical significance of Corynebacterium striatum isolated from human samples. Clin Microbiol Infect 3:634–639. https://doi.org/10.1111/j.1469-0691.1997.tb00470.x
Martins C et al (2009) Microbiological and host features associated with corynebacteriosis in cancer patients: a five-year study. Mem Inst Oswaldo Cruz 104:905–913. https://doi.org/10.1590/s0074-02762009000600015
Marull J, Casares PA (2008) Nosocomial valve endocarditis due to Corynebacterium striatum : a case report. Cases J 1:388. https://doi.org/10.1186/1757-1626-1-388
McMullen AR, Anderson N, Wallace MA, Shupe A, Burnham CA (2017) When good bugs go bad: epidemiology and antimicrobial resistance profiles of corynebacterium striatum, an emerging multidrug-resistant opportunistic pathogen. Antimicrob Agents Chemother. https://doi.org/10.1128/AAC.01111-17
Milosavljevic MN et al (2021) Antimicrobial treatment of Corynebacterium striatum invasive infections: a systematic review. Rev Inst Med Trop Sao Paulo 63:e49. https://doi.org/10.1590/S1678-9946202163049
Miro E et al (2013) Characterization of aminoglycoside-modifying enzymes in enterobacteriaceae clinical strains and characterization of the plasmids implicated in their diffusion. Microb Drug Resist 19:94–99. https://doi.org/10.1089/mdr.2012.0125
Navas J, Fernandez-Martinez M, Salas C, Cano ME, Martinez-Martinez L (2016) Susceptibility to aminoglycosides and distribution of aph and aac(3)-XI genes among Corynebacterium striatum clinical isolates. PLoS ONE 11:e0167856. https://doi.org/10.1371/journal.pone.0167856
Nguyen TT, Postle K, Bertrand KP (1983) Sequence homology between the tetracycline-resistance determinants of Tn10 and pBR322. Gene 25:83–92. https://doi.org/10.1016/0378-1119(83)90170-1
Nie L et al (2014) Genetic basis of high level aminoglycoside resistance in Acinetobacter baumannii from Beijing, China. Acta Pharm Sin B 4:295–300. https://doi.org/10.1016/j.apsb.2014.06.004
Nudel K et al (2018) Genomics of Corynebacterium striatum, an emerging multidrug-resistant pathogen of immunocompromised patients. Clin Microbiol Infect. https://doi.org/10.1016/j.cmi.2017.12.024
Peterson E, Kaur P (2018) Antibiotic resistance mechanisms in bacteria: relationships between resistance determinants of antibiotic producers, environmental bacteria, and clinical pathogens. Front Microbiol 9:2928. https://doi.org/10.3389/fmicb.2018.02928
Quainoo S et al (2017) Whole-genome sequencing of bacterial pathogens: the future of nosocomial outbreak analysis. Clin Microbiol Rev 30:1015–1063. https://doi.org/10.1128/CMR.00016-17
Ramos JN et al (2019) Bloodstream and catheter-related infections due to different clones of multidrug-resistant and biofilm producer Corynebacterium striatum. BMC Infect Dis 19:672. https://doi.org/10.1186/s12879-019-4294-7
Renom F, Garau M, Rubi M, Ramis F, Galmes A, Soriano JB (2007) Nosocomial outbreak of Corynebacterium striatum infection in patients with chronic obstructive pulmonary disease. J Clin Microbiol 45:2064–2067. https://doi.org/10.1128/JCM.00152-07
Rufael DW, Cohn SE (1994) Native valve endocarditis due to Corynebacterium striatum : case report and review. Clin Infect Dis 19:1054–1061. https://doi.org/10.1093/clinids/19.6.1054
Schroder J et al (2012) Complete genome sequence, lifestyle, and multi-drug resistance of the human pathogen Corynebacterium resistens DSM 45100 isolated from blood samples of a leukemia patient. BMC Genom 13:141. https://doi.org/10.1186/1471-2164-13-141
Sharma D, Misba L, Khan AU (2019) Antibiotics versus biofilm: an emerging battleground in microbial communities. Antimicrob Resist Infect Control 8:76. https://doi.org/10.1186/s13756-019-0533-3
Silva-Santana G et al (2021) Worldwide survey of Corynebacterium striatum increasingly associated with human invasive infections, nosocomial outbreak, and antimicrobial multidrug-resistance, 1976–2020. Arch Microbiol 203:1863–1880. https://doi.org/10.1007/s00203-021-02246-1
Soriano F, Zapardiel J, Nieto E (1995) Antimicrobial susceptibilities of Corynebacterium species and other non-spore-forming gram-positive bacilli to 18 antimicrobial agents. Antimicrob Agents Chemother 39:208–214. https://doi.org/10.1128/AAC.39.1.208
Souza C et al (2015) Biofilm production by multiresistant Corynebacterium striatum associated with nosocomial outbreak. Mem Inst Oswaldo Cruz 110:242–248. https://doi.org/10.1590/0074-02760140373
Souza C et al (2019) Virulence potential of Corynebacterium striatum towards Caenorhabditis elegans. Antonie Van Leeuwenhoek 112:1331–1340. https://doi.org/10.1007/s10482-019-01265-9
Souza C et al (2020) Resistance to antiseptics and disinfectants of planktonic and biofilm-associated forms of Corynebacterium striatum. Microb Drug Resist 26:1546–1558. https://doi.org/10.1089/mdr.2019.0124
Superti SV et al (2009) Corynebacterium striatum infecting a malignant cutaneous lesion: the emergence of an opportunistic pathogen. Rev Inst Med Trop Sao Paulo 51:115–116. https://doi.org/10.1590/s0036-46652009000200011
Tauch A, Krieft S, Kalinowski J, Puhler A (2000) The 51,409-bp R-plasmid pTP10 from the multiresistant clinical isolate Corynebacterium striatum M82B is composed of DNA segments initially identified in soil bacteria and in plant, animal, and human pathogens. Mol Gen Genet 263:1–11. https://doi.org/10.1007/pl00008668
Verma R, Kravitz GR (2016) Corynebacterium striatum empyema and osteomyelitis in a patient with advanced rheumatoid arthritis. BMJ Case Rep. https://doi.org/10.1136/bcr-2016-214691
Verroken A et al (2014) Epidemiological investigation of a nosocomial outbreak of multidrug-resistant Corynebacterium striatum at one Belgian university hospital. Clin Microbiol Infect 20:44–50. https://doi.org/10.1111/1469-0691.12197
Wang X et al (2019) Whole-genome sequencing reveals a prolonged and persistent intrahospital transmission of corynebacterium striatum, an emerging multidrug-resistant pathogen. J Clin Microbiol. https://doi.org/10.1128/JCM.00683-19
Wang X et al (2021) Genomic epidemiology of Corynebacterium striatum from three regions of China: an emerging national nosocomial epidemic. J Hosp Infect 110:67–75. https://doi.org/10.1016/j.jhin.2020.10.005
Werth BJ, Hahn WO, Butler-Wu SM, Rakita RM (2016) Emergence of high-level daptomycin resistance in Corynebacterium striatum in two patients with left ventricular assist device infections. Microb Drug Resist 22:233–237. https://doi.org/10.1089/mdr.2015.0208
Wong KY, Chan YC, Wong CY (2010) Corynebacterium striatum as an emerging pathogen. J Hosp Infect 76:371–372. https://doi.org/10.1016/j.jhin.2010.05.018
Yao L et al (2020) Prevalence of fluoroquinolone, macrolide and sulfonamide-related resistance genes in landfills from East China, mainly driven by MGEs. Ecotoxicol Environ Saf 190:110131. https://doi.org/10.1016/j.ecoenv.2019.110131
Yoo G, Kim J, Uh Y, Lee HG, Hwang GY, Yoon KJ (2015) Multidrug-resistant Corynebacterium striatum bacteremia: first case in Korea. Ann Lab Med 35:472–473. https://doi.org/10.3343/alm.2015.35.4.472
Acknowledgements
We gratefully thank Novogene Bioinformatics Institute, Beijing, China for providing technical support.
Funding
This study was supported by Financial Aid Project of Shanxi Province (2021RC0329).
Author information
Authors and Affiliations
Contributions
This study was conceived and designed by YC L. YC L and CY G performed the experiments. JR R provided guidance on data analysis. YC L analyzed the data and drafted the manuscript. All authors reviewed this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no commercial or financial relationships that could be a potential conflict of interest.
Consent for publication
Not applicable.
Ethical approval
This study was approved by the Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences ethical committee (YXLL-KY-2021–015) and all patients signed informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Y., Rong, J. & Gao, C. Phylogenetic analyses of antimicrobial resistant Corynebacterium striatum strains isolated from a nosocomial outbreak in a tertiary hospital in China. Antonie van Leeuwenhoek 116, 907–918 (2023). https://doi.org/10.1007/s10482-023-01855-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10482-023-01855-8