Abstract
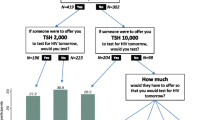
Under-detection of HIV/AIDS still burdens many low- and middle-income countries (LMICs). Our randomized trial investigated the effects of financial incentives and a behavioral nudge to induce HIV testing and learning HIV status in Ecuador. In the control group, 12.2% of participants agreed to testing, and 5.3% learned results. A financial incentive paid at testing increased the fraction of participants tested by 50.1 percentage points (95% CI 38.8 to 61.4) and the fraction who learned their status by 8.9 percentage points (95% CI 5.3 to 12.5); the nudge had no effect. The HIV-positive rate was 1.2% in the control group, and incentives prompted a 4.7 percentage point (95% CI 0.5 to 8.9) higher proportion of HIV-positive detection. Incentives also induced earlier testing, suggesting reduced procrastination. This suggests that information with appropriately timed small financial incentives can improve HIV testing and detection of new cases in the general population in LMIC settings.

Similar content being viewed by others
Data Availability
Data for replication purposes is available from the corresponding author upon reasonable request.
Code Availability
The code used to produce the analyses is available from the corresponding author upon reasonable request.
References
Ecuador Ministry of Health (Ministerio de Salud Publica, MdSP). Estrategia Nacional de VIH/SIODA-ITS. Viceministerio de Gobernanza y Vigilancia de Salud. Direccion Nacional de Estrategias de Salud Colectiva. Quito: Ministerio de Salud de Ecuador; 2012.
Joint United Nations Programme on HIV/AIDS. Country Fact Sheets – Ecuador 2017. Geneva: Joint United Nations Programme on HIV/AIDS; 2017. https://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf. Accessed 24 Feb 2021
Joint United Nations Programme on HIV/AIDS. AIDSinfo. Geneva: Joint United Nations Programme on HIV/AIDS; 2017. https://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf. Accessed 24 Feb 2021
Thaler R, Sunstein C. Nudge: improving decisions about health, wealth, and happiness. New Haven, CT: Yale University Press; 2008. p. 304.
Thornton R. The demand for, and impact of, learning HIV status. AER. 2008;98(5):1829–63.
Chamie G, Schaffer EM, Ndyabakira A, Emperador DM, Kwarisiima D, Camlin CS, Havlir DV, Kahn JG, Kamya MR, Thirumurthy H. Comparative effectiveness of novel non-monetary incentives to promote HIV testing: a randomized trial. AIDS. 2018;32(11):1443–51.
Montoy JCC, Dow WH, Kaplan BC. Patient choice in opt-in, active choice, and opt-out HIV screening: randomized clinical trial. BMJ. 2016;532:h6895. https://doi.org/10.1136/bmj.h6895.
Montoy JCC, Dow WH, Kaplan BC. Cash incentives versus defaults for HIV testing: a randomized clinical trial. PLoS ONE. 2018;13(7):e0199833. https://doi.org/10.1371/journal.pone.0199833.
Lee R, Cui RR, Muessig KE, Thirumurthy H, Tucker JD. Incentivizing HIV/STI testing: a systematic review of the literature. AIDS Behav. 2014;18(5):905–12.
Sibanda EL, Tumushime M, Mufuka J, Mavedzenge SN, Gudukeya S, Bautista-Arredondo S, Hatzold K, Thirumurthy H, McCoy SI, Padian N, Copas A. Effect of non-monetary incentives on uptake of couples’ counselling and testing among clients attending mobile HIV services in rural Zimbabwe: a cluster-randomized trial. Lancet Glob Health. 2017;5(9):e907–15.
Wall K, Allen S. Incentives to improve couples’ HIV testing uptake and cost-effectiveness. Lancet Glob Health. 2017;5(9):e847–8.
Yotebieng M, Thirumurthy H, Moracco KE, Kawende B, Chalachala JL, Wenzi LK, Ravelomanana NLR, Edmonds A, Thompson D, Okitolonda EW, Behets F. Conditional cash transfers and uptake of and retention in prevention of mother-to-child HIV transmission care: a randomized controlled trial. Lancet HIV. 2016;3(2):e85-93.
Thirumurthy H, Masters SH, Rao S, Bronson MA, Lanham M, Omanga E, Evens E, Agot K. Effect of providing conditional economic compensation on uptake of voluntary medical male circumcision in Kenya: a randomized clinical trial. JAMA. 2014;312(7):703–11.
Mills EJ, Adhvaryu A, Jakiela P, Birungi J, Okoboi S, Chimulwa TNW, Wanganisi J, Achilla T, Popoff E, Golchi S, Karlan D. Unconditional cash transfers for clinical and economic outcomes among HIV-affected Ugandan households. AIDS. 2018;32(14):2023–31.
de Walque D, Dow W, Nathan R, et al. Incentivising safe sex: a randomized trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open. 2012;2:e000747. https://doi.org/10.1136/bmjopen-2011-000747.
Bryan G, Karlan D, Nelson S. Commitment devices. Annu Rev Econom. 2010;2:671–98.
Anderberg D, Cerrone C, Chevalier A. Soft commitment: a study on demand and compliance. Appl Econ Lett. 2018;25(16):1140–6.
O’Donoghue T, Rabin M. Incentives for procrastinators. Q J Econ. 1999;114(3):769–816.
Owens SG, Bowman CG, Dill CA. Overcoming procrastination: the effect of implementation intentions 1. J Appl Soc Psychol. 2008;38(2):366–84.
Luiken GP, Joore IK, Taselaar A, Schuit SC, Geerlings SE, Govers A, Rood PP, Prins JM, Nichols BE, Verbon A, de Vries-Sluijs TEMS. Non-targeted HIV screening in emergency departments in the Netherlands. Neth J Med. 2017;75(9):386–93.
de Salud M, del Ecuador P. Monitoreo Global del Sida [Internet]. Quito: Informe GAM Ecuador; 2017. p. 1–65.
Censo de población y vivienda 2010. Ecuador: Instituto Nacional de Estadística y Censos; 2010.
Unger D, Gilbert M, Brownrigg B. Ethical considerations regarding anonymous HIV testing. Vancouver: Clinical Prevention Services, BC Centre for Disease Control; 2012.
Salway-Hottes T, Gilbert M. Anonymous HIV testing: evidence review and environmental scan. Vancouver: Clinical Prevention Services, BC Centre for Disease Control; 2012.
Wooldridge JM. Econometric analysis of cross section and panel data. Cambridge, MA: MIT Press; 2001. p. 776.
StataCorp. Stata statistical software: release 15. College Station, TX: StataCorp LLC; 2017.
Rogers W. Regression standard errors in clustered samples. Stata Technical Bulletin. 1994; 3(13)
Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–6.
Grieco D, Lacetera N, Macis M, Martino D. Motivating cord blood donation with information and behavioral nudges. Sci Rep. 2018;8(1):252.
Huang YLA, Lasry A, Hutchinson AB, Sansom SL. A systematic review on cost effectiveness of HIV prevention interventions in the United States. Appl Health Econ Health Policy. 2015;13(2):149–56.
Joint United Nations Programme on HIV/AIDS (UNAIDS). 90–90–90: An ambitious treatment target to help end the AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS; 2014. https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf. Accessed 24 Feb 2021
Bindman AB, Osmond D, Hecht FM, Lehman JS, Vranizan K, Keane D, Reingold A. Multistate evaluation of anonymous HIV testing and access to medical care. JAMA. 1998;280(16):1416–20.
Acknowledgements
We are grateful to the Creative and Novel Ideas in HIV Research (CNIHR) leadership and to 2017 and 2018 CNIHR workshop participants for valuable comments and support. We gratefully acknowledge the support of the Municipality of Esmeraldas, especially Mayor Lenin Lara, and Council Member Rubin Perea. We thank Adriana Elba Campos for excellent research assistance, and Sheronda Gordon for outstanding administrative support. We are especially grateful to Dr. Diogenes Cuero Caicedo and his team at the Fundacion Raices. Dr. Cuero Caicedo passed away prematurely in January 2019. He will be missed by many in his community of Esmeraldas. This article is dedicated to his memory.
Funding
This research was supported by the Creative and Novel Ideas in HIV Research (CNIHR) Program through a supplement to the University of Alabama at Birmingham (UAB) Center For AIDS Research funding (P30 AI027767). This funding was made possible by collaborative efforts of the Office of AIDS Research, the National Institute of Allergy and Infectious Diseases, and the International AIDS Society.
Author information
Authors and Affiliations
Contributions
MM, MG, RI, MRO, PP, and ET conceived and designed the study. CR and EG conducted the fieldwork and collected the data. ET and MM supervised the study. ET was responsible for the lab analysis. MM performed the statistical analysis. MM and PP and wrote the first draft. All authors contributed to the interpretation of the results, revised the manuscript for important intellectual content, and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
The study was approved by the Johns Hopkins Homewood Institutional Review Board and by the Institutional Review Board of the Universidad San Francisco de Quito in Ecuador.
Consent to Participate
Verbal informed consent was obtained prior to the interview and intervention.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Macis, M., Grunauer, M., Gutierrez, E. et al. Using Incentives and Nudging to Improve Non-Targeted HIV Testing in Ecuador: A Randomized Trial. AIDS Behav 25, 2542–2550 (2021). https://doi.org/10.1007/s10461-021-03215-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03215-x