Abstract
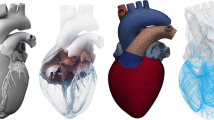
Multiscale models of the cardiovascular system are emerging as effective tools for investigating the mechanisms that drive ventricular growth and remodeling. These models can predict how molecular-level mechanisms impact organ-level structure and function and could provide new insights that help improve patient care. MyoFE is a multiscale computer framework that bridges molecular and organ-level mechanisms in a finite element model of the left ventricle that is coupled with the systemic circulation. In this study, we extend MyoFE to include a growth algorithm, based on volumetric growth theory, to simulate concentric growth (wall thickening/thinning) and eccentric growth (chamber dilation/constriction) in response to valvular diseases. Specifically in our model, concentric growth is controlled by time-averaged total stress along the fiber direction over a cardiac cycle while eccentric growth responds to time-averaged intracellular myofiber passive stress over a cardiac cycle. The new framework correctly predicted different forms of growth in response to two types of valvular diseases, namely aortic stenosis and mitral regurgitation. Furthermore, the model predicted that LV size and function are nearly restored (reversal of growth) when the disease-mimicking perturbation was removed in the simulations for each valvular disorder. In conclusion, the simulations suggest that time-averaged total stress along the fiber direction and time-averaged intracellular myofiber passive stress can be used to drive concentric and eccentric growth in simulations of valve disease.






Similar content being viewed by others
References
Frey, N., and E. N. Olson. Cardiac hypertrophy: the good, the bad, and the ugly. Annu. Rev. Physiol. 65:45–79, 2003. https://doi.org/10.1146/annurev.physiol.65.092101.142243.
Pitoulis, F. G., and C. M. Terracciano. Heart plasticity in response to pressure- and volume-overload: a review of findings in compensated and decompensated phenotypes. Front Physiol. 11:92, 2020. https://doi.org/10.3389/fphys.2020.00092.
Hill, J. A., and E. N. Olson. Cardiac plasticity. N. Engl. J. Med. 358(13):1370–1380, 2008. https://doi.org/10.1056/NEJMra072139.
Shimizu, I., and T. Minamino. Physiological and pathological cardiac hypertrophy. J. Mol. Cell Cardiol. 97:245–262, 2016. https://doi.org/10.1016/j.yjmcc.2016.06.001.
Nakamura, M., and J. Sadoshima. Mechanisms of physiological and pathological cardiac hypertrophy. Nat. Rev. Cardiol. 15(7):387–407, 2018. https://doi.org/10.1038/s41569-018-0007-y.
Rausch, M. K., A. Dam, S. Goktepe, O. J. Abilez, and E. Kuhl. Computational modeling of growth: systemic and pulmonary hypertension in the heart. Biomech. Model Mechanobiol. 10(6):799–811, 2011. https://doi.org/10.1007/s10237-010-0275-x.
Klepach, D., L. C. Lee, J. F. Wenk, M. B. Ratcliffe, T. I. Zohdi, J. A. Navia, et al. Growth and remodeling of the left ventricle: a case study of myocardial infarction and surgical ventricular restoration. Mech. Res. Commun. 42:134–141, 2012. https://doi.org/10.1016/j.mechrescom.2012.03.005.
Guterl, K. A., C. R. Haggart, P. M. Janssen, and J. W. Holmes. Isometric contraction induces rapid myocyte remodeling in cultured rat right ventricular papillary muscles. Am. J. Physiol. Heart Circ. Physiol. 293(6):H3707–H3712, 2007. https://doi.org/10.1152/ajpheart.00296.2007.
Kerckhoffs, R. C., J. Omens, and A. D. McCulloch. A single strain-based growth law predicts concentric and eccentric cardiac growth during pressure and volume overload. Mech. Res. Commun. 42:40–50, 2012. https://doi.org/10.1016/j.mechrescom.2011.11.004.
Witzenburg, C. M., and J. W. Holmes. Predicting the time course of ventricular dilation and thickening using a rapid compartmental model. J Cardiovasc. Transl. Res. 11(2):109–122, 2018. https://doi.org/10.1007/s12265-018-9793-1.
Arts, T., J. Lumens, W. Kroon, and T. Delhaas. Control of whole heart geometry by intramyocardial mechano-feedback: a model study. PLoS Comput. Biol.8(2):e1002369, 2012. https://doi.org/10.1371/journal.pcbi.1002369.
Goktepe, S., O. J. Abilez, K. K. Parker, and E. Kuhl. A multiscale model for eccentric and concentric cardiac growth through sarcomerogenesis. J. Theoret. Biol. 265(3):433–442, 2010. https://doi.org/10.1016/j.jtbi.2010.04.023.
Lin, I. E., and L. A. Taber. A model for stress-induced growth in the developing heart. J. Biomech. Eng. 117(3):343–349, 1995. https://doi.org/10.1115/1.2794190.
Kroon, W., T. Delhaas, T. Arts, and P. Bovendeerd. Computational modeling of volumetric soft tissue growth: application to the cardiac left ventricle. Biomech. Model Mechanobiol. 8(4):301–309, 2009. https://doi.org/10.1007/s10237-008-0136-z.
Lee, L. C., M. Genet, G. Acevedo-Bolton, K. Ordovas, J. M. Guccione, and E. Kuhl. A computational model that predicts reverse growth in response to mechanical unloading. Biomech. Model Mechanobiol. 14(2):217–229, 2015. https://doi.org/10.1007/s10237-014-0598-0.
Sharifi, H., C. K. Mann, A. L. Rockward, M. Mehri, J. Mojumder, L. C. Lee, et al. Multiscale simulations of left ventricular growth and remodeling. Biophys. Rev. 13(5):729–746, 2021. https://doi.org/10.1007/s12551-021-00826-5.
Lee, L. C., J. Sundnes, M. Genet, J. F. Wenk, and S. T. Wall. An integrated electromechanical-growth heart model for simulating cardiac therapies. Biomech. Model Mechanobiol. 15(4):791–803, 2016. https://doi.org/10.1007/s10237-015-0723-8.
Arumugam, J., J. Mojumder, G. Kassab, and L. C. Lee. Model of anisotropic reverse cardiac growth in mechanical dyssynchrony. Sci. Rep. 9(1):12670, 2019. https://doi.org/10.1038/s41598-019-48670-8.
Arts, T., T. Delhaas, P. Bovendeerd, X. Verbeek, and F. W. Prinzen. Adaptation to mechanical load determines shape and properties of heart and circulation: the CircAdapt model. Am. J. Physiol Heart Circ. Physiol. 288(4):H1943–H1954, 2005. https://doi.org/10.1152/ajpheart.00444.2004.
Guccione, J. M., and A. D. McCulloch. Mechanics of active contraction in cardiac muscle: Part I—constitutive relations for fiber stress that describe deactivation. J Biomech Eng. 115(1):72–81, 1993. https://doi.org/10.1115/1.2895473.
Guccione, J. M., L. K. Waldman, and A. D. McCulloch. Mechanics of active contraction in cardiac muscle: Part II—cylindrical models of the systolic left ventricle. J. Biomech. Eng. 115(1):82–90, 1993. https://doi.org/10.1115/1.2895474.
Estrada, A. C., K. Yoshida, J. J. Saucerman, and J. W. Holmes. A multiscale model of cardiac concentric hypertrophy incorporating both mechanical and hormonal drivers of growth. Biomech. Model Mechanobiol. 20(1):293–307, 2021. https://doi.org/10.1007/s10237-020-01385-6.
Beyar, R., and S. Sideman. Model for left ventricular contraction combining the force length velocity relationship with the time varying elastance theory. Biophys. J. 45(6):1167–1177, 1984. https://doi.org/10.1016/S0006-3495(84)84265-4.
Santamore, W. P., and D. Burkhoff. Hemodynamic consequences of ventricular interaction as assessed by model analysis. Am. J. Physiol. 260(1 Pt 2):H146–H157, 1991. https://doi.org/10.1152/ajpheart.1991.260.1.H146.
Rondanina, E., and P. H. M. Bovendeerd. Evaluation of stimulus-effect relations in left ventricular growth using a simple multiscale model. Biomech. Model Mechanobiol. 19(1):263–273, 2020. https://doi.org/10.1007/s10237-019-01209-2.
Rondanina, E., and P. H. M. Bovendeerd. Stimulus-effect relations for left ventricular growth obtained with a simple multi-scale model: the influence of hemodynamic feedback. Biomech. Model Mechanobiol. 19(6):2111–2126, 2020. https://doi.org/10.1007/s10237-020-01327-2.
Bovendeerd, P. H., P. Borsje, T. Arts, and F. N. van De Vosse. Dependence of intramyocardial pressure and coronary flow on ventricular loading and contractility: a model study. Ann. Biomed. Eng. 34(12):1833–1845, 2006. https://doi.org/10.1007/s10439-006-9189-2.
Huxley, A. F. Muscular contraction. J. Physiol. 243(1):1–43, 1974.
Freiburg, A., K. Trombitas, W. Hell, O. Cazorla, F. Fougerousse, T. Centner, et al. Series of exon-skipping events in the elastic spring region of titin as the structural basis for myofibrillar elastic diversity. Circ. Res. 86(11):1114–1121, 2000. https://doi.org/10.1161/01.res.86.11.1114.
Davis, J., L. C. Davis, R. N. Correll, C. A. Makarewich, J. A. Schwanekamp, F. Moussavi-Harami, et al. A tension-based model distinguishes hypertrophic versus dilated cardiomyopathy. Cell. 165(5):1147–1159, 2016. https://doi.org/10.1016/j.cell.2016.04.002.
Shavik, S. M., S. Wall, J. Sundnes, J. M. Guccione, P. Sengupta, S. D. Solomon, et al. Computational modeling studies of the roles of left ventricular geometry, afterload, and muscle contractility on myocardial strains in heart failure with preserved ejection fraction. J. Cardiovasc. Transl. Res. 14(6):1131–1145, 2021. https://doi.org/10.1007/s12265-021-10130-y.
Bayer, J. D., R. C. Blake, G. Plank, and N. A. Trayanova. A novel rule-based algorithm for assigning myocardial fiber orientation to computational heart models. Ann. Biomed. Eng. 40(10):2243–2254, 2012. https://doi.org/10.1007/s10439-012-0593-5.
Alnaes, M. S., J. Blechta, J. Hake, A. Johansson, B. Kehlet, A. Logg, C. Richardson, J. Ring, M. E. Rognes, and G. N. Wells. The FEniCS project version 1.5. Numer. Softw Arch. 2015. https://doi.org/10.11588/ans.2015.100.20553.
Finsberg, H., C. Xi, J. L. Tan, L. Zhong, M. Genet, J. Sundnes, et al. Efficient estimation of personalized biventricular mechanical function employing gradient-based optimization. Int. J. Numer. Method Biomed. Eng.34(7):e2982, 2018. https://doi.org/10.1002/cnm.2982.
Boffi, D., F. Brezzi, and M. Fortin. Mixed Finite Element Methods and Applications. Berlin: Springer, 2013.
Guccione, J. M., A. D. McCulloch, and L. K. Waldman. Passive material properties of intact ventricular myocardium determined from a cylindrical model. J. Biomech. Eng. 113(1):42–55, 1991. https://doi.org/10.1115/1.2894084.
Xi, C., G. S. Kassab, and L. C. Lee. Microstructure-based finite element model of left ventricle passive inflation. Acta Biomater. 90:241–253, 2019. https://doi.org/10.1016/j.actbio.2019.04.016.
Campbell, K. S. Dynamic coupling of regulated binding sites and cycling myosin heads in striated muscle. J. Gen. Physiol. 143(3):387–399, 2014. https://doi.org/10.1085/jgp.201311078.
Sharifi, H., L. C. Lee, K. S. Campbell, and J. F. Wenk. A multiscale finite element model of left ventricular mechanics incorporating baroreflex regulation. Comput. Biol. Med.168:107690, 2024. https://doi.org/10.1016/j.compbiomed.2023.107690.
Sharifi, H., C. K. Mann, J. F. Wenk, and K. S. Campbell. A multiscale model of the cardiovascular system that regulates arterial pressure via closed loop baroreflex control of chronotropism, cell-level contractility, and vascular tone. Biomech. Model Mechanobiol. 21(6):1903–1917, 2022. https://doi.org/10.1007/s10237-022-01628-8.
Rodriguez, E. K., A. Hoger, and A. D. McCulloch. Stress-dependent finite growth in soft elastic tissues. J. Biomech. 27(4):455–467, 1994. https://doi.org/10.1016/0021-9290(94)90021-3.
Kondaurov, V. I., and L. V. Nikitin. Finite strains of viscoelastic muscle tissue. Appl. Math. Mech. 51(3):346–353, 1987. https://doi.org/10.1016/0021-8928(87)90111-0.
Takamizawa, K., and K. Hayashi. Strain energy density function and uniform strain hypothesis for arterial mechanics. Biomechanics. 20(1):7–17, 1987. https://doi.org/10.1016/0021-9290(87)90262-4.
Takamizawa, K., and T. Matsuda. Kinematics for bodies undergoing residual stress and its applications to the left ventricle. Appl. Mech. 57(2):321–329, 1990. https://doi.org/10.1115/1.2891992.
Takamizawa, K. Stress-free configuration of a thick-walled cylindrical model of the artery: an application of riemann geometry to the biomechanics of soft tissues. Appl. Mech. 58(3):840–842, 1991. https://doi.org/10.1115/1.2897272.
Sadik, S., and A. Yavari. On the origins of the idea of the multiplicative decomposition of the deformation gradient. Math. Mech. Solids. 22(4):771–772, 2015. https://doi.org/10.1177/1081286515612280.
Walt, S. V. D., S. C. Colbert, and G. Varoquaux. The NumPy Array: a structure for efficient numerical computation. Comput. Sci. Eng. 13:22–30, 2011. https://doi.org/10.1109/MCSE.2011.37.
Virtanen, P., R. Gommers, T. E. Oliphant, M. Haberland, T. Reddy, D. Cournapeau, et al. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat. Methods. 17(3):261–272, 2020. https://doi.org/10.1038/s41592-019-0686-2.
al. RJe. pandas-dev/pandas: Pandas 1.3.2. 2021.
Petersen, S. E., N. Aung, M. M. Sanghvi, F. Zemrak, K. Fung, J. M. Paiva, et al. Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. J. Cardiovasc. Magn. Reson. 19(1):18, 2017. https://doi.org/10.1186/s12968-017-0327-9.
Maceira, A. M., S. K. Prasad, M. Khan, and D. J. Pennell. Normalized left ventricular systolic and diastolic function by steady state free precession cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 8(3):417–426, 2006. https://doi.org/10.1080/10976640600572889.
Otto, C. M., R. A. Nishimura, R. O. Bonow, B. A. Carabello, J. P. Erwin 3rd., F. Gentile, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 143(5):e72–e227, 2021. https://doi.org/10.1161/CIR.0000000000000923.
Chin, C. W., H. J. Khaw, E. Luo, S. Tan, A. C. White, D. E. Newby, et al. Echocardiography underestimates stroke volume and aortic valve area: implications for patients with small-area low-gradient aortic stenosis. Can. J. Cardiol. 30(9):1064–1072, 2014. https://doi.org/10.1016/j.cjca.2014.04.021.
Chin, C. W. L., R. J. Everett, J. Kwiecinski, A. T. Vesey, E. Yeung, G. Esson, et al. Myocardial fibrosis and cardiac decompensation in aortic stenosis. JACC Cardiovasc. Imaging. 10(11):1320–1333, 2017. https://doi.org/10.1016/j.jcmg.2016.10.007.
Luszczak, J., M. Olszowska, S. Drapisz, W. Plazak, I. Karch, M. Komar, et al. Assessment of left ventricle function in patients with symptomatic and asymptomatic aortic stenosis by 2-dimensional speckle-tracking imaging. Med. Sci. Monit. 18(12):MT91-6, 2012. https://doi.org/10.12659/msm.883587.
Everett, R. J., T. A. Treibel, M. Fukui, H. Lee, M. Rigolli, A. Singh, et al. Extracellular myocardial volume in patients with aortic stenosis. J. Am. Coll. Cardiol. 75(3):304–316, 2020. https://doi.org/10.1016/j.jacc.2019.11.032.
Spath, N. B., M. Gomez, R. J. Everett, S. Semple, C. W. L. Chin, A. C. White, et al. Global longitudinal strain analysis using cardiac mri in aortic stenosis: comparison with left ventricular remodeling, myocardial fibrosis, and 2-year clinical outcomes. Radiol. Cardiothorac. Imaging.1(4):e190027, 2019. https://doi.org/10.1148/ryct.2019190027.
Lyon, R. C., F. Zanella, J. H. Omens, and F. Sheikh. Mechanotransduction in cardiac hypertrophy and failure. Circ. Res. 116(8):1462–1476, 2015. https://doi.org/10.1161/CIRCRESAHA.116.304937.
Knoll, R., M. Hoshijima, H. M. Hoffman, V. Person, I. Lorenzen-Schmidt, M. L. Bang, et al. The cardiac mechanical stretch sensor machinery involves a Z disc complex that is defective in a subset of human dilated cardiomyopathy. Cell. 111(7):943–955, 2002. https://doi.org/10.1016/s0092-8674(02)01226-6.
Edwards, N. C., W. E. Moody, M. Yuan, P. Weale, D. Neal, J. N. Townend, et al. Quantification of left ventricular interstitial fibrosis in asymptomatic chronic primary degenerative mitral regurgitation. Circ. Cardiovasc. Imaging. 7(6):946–953, 2014. https://doi.org/10.1161/CIRCIMAGING.114.002397.
Schiros, C. G., L. J. Dell’Italia, J. D. Gladden, D. Clark 3rd., I. Aban, H. Gupta, et al. Magnetic resonance imaging with 3-dimensional analysis of left ventricular remodeling in isolated mitral regurgitation: implications beyond dimensions. Circulation. 125(19):2334–2342, 2012. https://doi.org/10.1161/CIRCULATIONAHA.111.073239.
Seldrum, S., C. de Meester, S. Pierard, A. Pasquet, S. Lazam, J. Boulif, et al. Assessment of left ventricular reverse remodeling by cardiac MRI in patients undergoing repair surgery for severe aortic or mitral regurgitation. J. Cardiothorac. Vasc. Anesth. 33(7):1901–1911, 2019. https://doi.org/10.1053/j.jvca.2018.11.013.
Badke, F. R., and J. W. Covell. Early changes in left ventricular regional dimensions and function during chronic volume overloading in the conscious dog. Circ. Res. 45(3):420–428, 1979. https://doi.org/10.1161/01.res.45.3.420.
Park, K., T. H. Park, Y. S. Jo, Y. R. Cho, J. S. Park, M. H. Kim, et al. Prognostic effect of increased left ventricular wall thickness in severe aortic stenosis. Cardiovasc. Ultrasound. 19(1):5, 2021. https://doi.org/10.1186/s12947-020-00234-x.
Barone-Rochette, G., S. Pierard, S. Seldrum, C. de Meester Ravenstein, J. Melchior, F. Maes, et al. Aortic valve area, stroke volume, left ventricular hypertrophy, remodeling, and fibrosis in aortic stenosis assessed by cardiac magnetic resonance imaging: comparison between high and low gradient and normal and low flow aortic stenosis. Circ. Cardiovasc. Imaging. 6(6):1009–1017, 2013. https://doi.org/10.1161/CIRCIMAGING.113.000515.
Huxley, A. F. Muscle structure and theories of contraction. Prog. Biophys. Biophys. Chem. 7:255–318, 1957.
Yoshida, K., and J. W. Holmes. Computational models of cardiac hypertrophy. Prog. Biophys. Mol. Biol. 159:75–85, 2021. https://doi.org/10.1016/j.pbiomolbio.2020.07.001.
Yoshida, K., A. D. McCulloch, J. H. Omens, and J. W. Holmes. Predictions of hypertrophy and its regression in response to pressure overload. Biomech. Model Mechanobiol. 19(3):1079–1089, 2020. https://doi.org/10.1007/s10237-019-01271-w.
Witzenburg, C. M., and J. W. Holmes. A comparison of phenomenologic growth laws for myocardial hypertrophy. J. Elast. 129(1–2):257–281, 2017. https://doi.org/10.1007/s10659-017-9631-8.
Oomen, P. J. A., T. N. Phung, S. H. Weinberg, K. C. Bilchick, and J. W. Holmes. A rapid electromechanical model to predict reverse remodeling following cardiac resynchronization therapy. Biomech. Model Mechanobiol. 21(1):231–247, 2022. https://doi.org/10.1007/s10237-021-01532-7.
Walther, T., A. Schubert, V. Falk, C. Binner, C. Walther, N. Doll, et al. Left ventricular reverse remodeling after surgical therapy for aortic stenosis: correlation to Renin-Angiotensin system gene expression. Circulation. 106(12 Suppl 1):I23–I26, 2002.
Giannini, C., A. S. Petronio, M. De Carlo, F. Guarracino, L. Conte, F. Fiorelli, et al. Integrated reverse left and right ventricular remodelling after MitraClip implantation in functional mitral regurgitation: an echocardiographic study. Eur. Heart J. Cardiovasc. Imaging. 15(1):95–103, 2014. https://doi.org/10.1093/ehjci/jet141.
Campbell, K. S., P. M. L. Janssen, and S. G. Campbell. Force-dependent recruitment from the myosin off state contributes to length-dependent activation. Biophys. J. 115(3):543–553, 2018. https://doi.org/10.1016/j.bpj.2018.07.006.
Mojumder, J., J. S. Choy, S. Leng, L. Zhong, G. S. Kassab, and L. C. Lee. Mechanical stimuli for left ventricular growth during pressure overload. Exp. Mech. 61(1):131–146, 2021. https://doi.org/10.1007/s11340-020-00643-z.
Gebauer, A. M., M. R. Pfaller, F. A. Braeu, C. J. Cyron, and W. A. Wall. A homogenized constrained mixture model of cardiac growth and remodeling: analyzing mechanobiological stability and reversal. Biomech. Model Mechanobiol. 2023. https://doi.org/10.1007/s10237-023-01747-w.
Washio, T., S. Sugiura, J. I. Okada, and T. Hisada. Using systolic local mechanical load to predict fiber orientation in ventricles. Front Physiol. 11:467, 2020. https://doi.org/10.3389/fphys.2020.00467.
Acknowledgments
Support for this research was provided by National Institutes of Health grants R01 HL163977 and U01 HL133359.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Additional information
Associate Editor Arash Kheradvar oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharifi, H., Mehri, M., Mann, C.K. et al. Multiscale Finite Element Modeling of Left Ventricular Growth in Simulations of Valve Disease. Ann Biomed Eng (2024). https://doi.org/10.1007/s10439-024-03497-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10439-024-03497-x