Abstract
Background
After laparoscopic fundoplication, 10–20% of patients experience symptom recurrence—often due to resurgence of the hiatal hernia. The standard surgical treatment for such cases remains laparoscopic revision fundoplication. However, there is little data on the time frame and anatomic patterns of failed fundoplications. Additionally, few large studies exist on the long-term efficacy and safety of laparoscopic revision fundoplication.
Methods
In a single-center, retrospective analysis of 194 consecutive revision fundoplications for recurrent reflux disease due to hiatal hernia, we collected data on time to failure and patterns of failure of the primary operation, as well as on the efficacy and safety of the revision.
Results
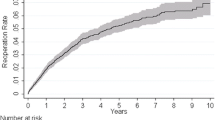
The median time to failure of the primary fundoplication was 3 years. Most hiatal defects were smaller than 5 cm and located anteriorly or concentric around the esophagus. Laparoscopic redo fundoplication was technically successful in all cases. The short-term complication rate was 9%, mainly dysphagia requiring endoscopic intervention. At a mean follow-up of 4.7 years, 77% of patients were symptom-free, 14% required daily PPI, and 9% underwent secondary revision. Cumulative failure rates were 9%, 23%, and 31% at 1, 5, and 10 years.
Conclusion
The majority of failed fundoplications occur within 3 years of primary surgery, with most patients exhibiting anterior or concentric defects. For these patients, laparoscopic revision fundoplication is a safe procedure with a low rate of short-term complications and satisfactory long-term results.




Similar content being viewed by others
References
Pessaux P, Arnaud J-P, Delattre J-F, Meyer C, Baulieux J, Mosnier H. Laparoscopic antireflux surgery: five-year results and beyond in 1340 patients. Arch Surg (Chicago, Ill: 1960). 2005;140(10):946–51. https://doi.org/10.1001/archsurg.140.10.946.
Al-Hashmi A-W, et al. A retrospective multicenter analysis on redo-laparoscopic anti-reflux surgery: Conservative or conversion fundoplication? Surg Endosc. 2019;33(1):243–51. https://doi.org/10.1007/s00464-018-6304-z.
Hunter JG, et al. Laparoscopic fundoplication failures: patterns of failure and response to fundoplication revision. Ann Surg. 1999;230(4):595–604. https://doi.org/10.1097/00000658-199910000-00015. (Discussion 604–6).
Hatch KF, Daily MF, Christensen BJ, Glasgow RE. Failed fundoplications. Am J Surg. 2004;188(6):786–91. https://doi.org/10.1016/j.amjsurg.2004.08.062.
Hoshino M, et al. Comparison of laparoscopic Nissen and Toupet fundoplication using a propensity score matching analysis. Surg Today. 2017;47(10):1195–200. https://doi.org/10.1007/s00595-017-1490-1.
Furnée EJB, Draaisma WA, Broeders IAMJ, Gooszen HG. Surgical reintervention after failed antireflux surgery: a systematic review of the literature. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2009;13(8):1539–49. https://doi.org/10.1007/s11605-009-0873-z.
Fuchs KH, Breithaupt W, Varga G, Babic B, Eckhoff J, Meining A. How effective is laparoscopic redo-antireflux surgery? Dis Esophagus Off J Int Soc Dis Esophagus. 2022. https://doi.org/10.1093/dote/doab091.
Watson DI, Baigrie RJ, Jamieson GG. A learning curve for laparoscopic fundoplication. Definable, avoidable, or a waste of time? Ann Surg. 1996;224(2):198–203. https://doi.org/10.1097/00000658-199608000-00013.
Yano F, et al. Outcomes of redo surgery for failed laparoscopic fundoplication. Esophagus. 2016;13(3):290–4. https://doi.org/10.1007/s10388-016-0532-x. (in En;en).
Schlottmann F, Laxague F, Angeramo CA, Sadava EE, Herbella FAM, Patti MG. Outcomes of laparoscopic redo fundoplication in patients with failed antireflux surgery: a systematic review and meta-analysis. Ann Surg. 2021;274(1):78–85. https://doi.org/10.1097/SLA.0000000000004639.
Suppiah A, Sirimanna P, Vivian SJ, O’Donnell H, Lee G, Falk GL. Temporal patterns of hiatus hernia recurrence and hiatal failure: quality of life and recurrence after revision surgery. Dis Esophagus Off J Int Soc Dis Esophagus. 2017;30(4):1–8. https://doi.org/10.1093/dote/dow035.
Granderath FA, Schweiger UM, Pointner R. Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc. 2007;21(4):542–8. https://doi.org/10.1007/s00464-006-9041-7.
Clavien PA, et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. https://doi.org/10.1097/SLA.0b013e3181b13ca2.
Kato K, Doki Y, Ogata T, et al. First-line nivolumab plus ipilimumab or chemotherapy versus chemotherapy alone in advanced esophageal squamous cell carcinoma: a Japanese subgroup analysis of open-label, phase 3 trial (CheckMate 648/ONO-4538-50). Esophagus. 2023;20:291–301. https://doi.org/10.1007/s10388-022-00970-1.
Motoyama S, Maeda E, Yano M, et al. Esophagectomy performed at institutes certified by the Japan esophageal society provide long-term survival advantages to esophageal cancer patients: second report analyzing 4897 cases with propensity score matching. Esophagus. 2020;17:141–8. https://doi.org/10.1007/s10388-019-00712-w.
Zhang M, Liang M, Chen S, et al. Novel physiologic nomogram discriminates symptom outcome in patients with erosive esophagitis. Esophagus. 2021;18:407–15. https://doi.org/10.1007/s10388-020-00793-y.
Awais O, et al. Reoperative antireflux surgery for failed fundoplication: an analysis of outcomes in 275 patients. Ann Thorac Surg. 2011;92(3):1083–9. https://doi.org/10.1016/j.athoracsur.2011.02.088. (Discussion 1089–90).
Smith CD, McClusky DA, Rajad MA, Lederman AB, Hunter JG. When fundoplication fails: Redo? Ann Surg. 2005;241(6):861–9. https://doi.org/10.1097/01.sla.0000165198.29398.4b. (Discussion 869–71).
Schlottmann F, Strassle PD, Patti MG. Antireflux surgery in the USA: Influence of surgical volume on perioperative outcomes and costs-time for centralization? World J Surg. 2018;42(7):2183–9. https://doi.org/10.1007/s00268-017-4429-1.
Granderath FA, Schweiger UM, Kamolz T, Asche KU, Pointner R. Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg. 2005;140(1):40–8. https://doi.org/10.1001/archsurg.140.1.40.
Aiolfi A, et al. Patient-tailored algorithm for laparoscopic cruroplasty standardization: comparison with hiatal surface area and medium-term outcomes. Langenbecks Arch Surg. 2022;407(6):2537–45. https://doi.org/10.1007/s00423-022-02556-y.
Moten AS, et al. In vivo measurement of esophageal hiatus surface area using MDCT: description of the methodology and clinical validation. Abdom Radiol. 2020;45(9):2656–62. https://doi.org/10.1007/s00261-019-02279-7.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Björn Siemssen and Marius Ibach performed material preparation, data collection, and analysis. Marius Ibach wrote the first draft of the manuscript, and all authors commented on previous versions of the manuscript. All authors—Björn Siemssen, Florian Hentschel, and Marius Ibach—read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
Dr. Ibach, Dr. Siemssen, and Dr. Hentschel declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Siemssen, B., Hentschel, F. & Ibach, M.J. Long-term results after laparoscopic revision fundoplication: a retrospective, single-center analysis in 194 patients with recurrent hiatal hernia. Esophagus (2024). https://doi.org/10.1007/s10388-024-01060-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10388-024-01060-0