Abstract
Background
Dysphagia after esophagectomy, especially in the early postoperative period, remains a severe complication. The association between sarcopenia and dysphagia has received attention in geriatric non-cancer populations. This study aimed to determine the associations between sarcopenia parameters and early postoperative dysphagia after esophagectomy.
Methods
This retrospective observational study included 201 consecutive male patients undergoing thoracoscopic–laparoscopic esophagectomy (TLE) for esophageal cancer between October 2018 and December 2020. We used three sarcopenia parameters: handgrip strength (HGS), skeletal muscle index, and gait speed. Postoperative swallowing function was assessed by videofluoroscopy using the penetration–aspiration scale (PAS; range 1–8). Logistic regression analyses were used to predict factors associated with postoperative aspiration (PAS 6–8). Furthermore, we compared values in patients with symptomatic aspiration (PAS 6–7) and with silent aspiration (PAS 8).
Results
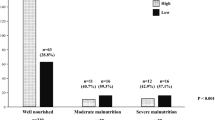
Aspiration occurred in 38 of 201 patients (18.9%). On multivariate analysis, significant predictors of aspiration included age [odds ratio (OR) 1.11; 95% confidence interval (CI) 1.05–1.17; p < 0.001], low HGS (OR 3.05; 95% CI 1.06–8.78; p = 0.039), upper third esophageal cancer (OR 2.79; 95% CI 1.03–7.54; p = 0.044) and recurrent laryngeal nerve palsy (OR 2.98; 95% CI 1.26–7.06; p = 0.013). Furthermore, among patients with aspiration (PAS 6–8), low HGS was significantly associated with silent aspiration (OR 6.43; 95% CI 1.06–39.00; p = 0.043).
Conclusions
Low HGS was significantly associated with early postoperative aspiration and impairment of airway protective reflexes after TLE.



Similar content being viewed by others
References
Easterling CS, Bousamra M 2nd, Lang IM, et al. Pharyngeal dysphagia in postesophagectomy patients: correlation with deglutitive biomechanics. Ann Thorac Surg. 2000;69:989–92.
Yasuda T, Yano M, Miyata H, et al. Evaluation of dysphagia and diminished airway protection after three-field esophagectomy and a remedy. World J Surg. 2013;37:416–23.
Lee SY, Cheon HJ, Kim SJ, Shim YM, Zo JI, Hwang JH. Clinical predictors of aspiration after esophagectomy in esophageal cancer patients. Support Care Cancer. 2016;24:295–9.
Mafune T, Mikami S, Otsubo T, et al. An investigation of factors related to food intake ability and swallowing difficulty after surgery for thoracic esophageal cancer. Dysphagia. 2019;34:592–9.
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21:300–7.
Simonsen C, de Heer P, Bjerre ED, et al. Sarcopenia and postoperative complication risk in gastrointestinal surgical oncology: a meta-analysis. Ann Surg. 2018;268:58–69.
Kurita D, Oguma J, Ishiyama K, Hirano Y, Kanamori J, Daiko H. Handgrip strength predicts postoperative pneumonia after thoracoscopic-laparoscopic esophagectomy for patients with esophageal cancer. Ann Surg Oncol. 2020;27:3173–81.
Zhao WT, Yang M, Wu HM, Yang L, Zhang XM, Huang Y. Systematic review and meta-analysis of the association between sarcopenia and dysphagia. J Nutr Health Aging. 2018;22:1003–9.
Fujishima I, Fujiu-Kurachi M, Arai H, et al. Sarcopenia and dysphagia: position paper by four professional organizations. Geriatr Gerontol Int. 2019;19:91–7.
Wakabayashi H, Takahashi R, Murakami T. The prevalence and prognosis of sarcopenic dysphagia in patients who require dysphagia rehabilitation. J Nutr Health Aging. 2019;23:84–8.
Yoshimura Y, Wakabayashi H, Bise T, et al. Sarcopenia is associated with worse recovery of physical function and dysphagia and a lower rate of home discharge in Japanese hospitalized adults undergoing convalescent rehabilitation. Nutrition. 2019;61:111–8.
Wakabayashi H, Matsushima M, Uwano R, Watanabe N, Oritsu H, Shimizu Y. Skeletal muscle mass is associated with severe dysphagia in cancer patients. J Cachexia Sarcopenia Muscle. 2015;6:351–7.
Ben-David K, Fullerton A, Rossidis G, et al. Prospective comprehensive swallowing evaluation of minimally invasive esophagectomies with cervical anastomosis: silent versus vocal aspiration. J Gastrointest Surg. 2015;19:1748–52.
Kitagawa Y, Uno T, Oyama T, et al. Esophageal cancer practice guidelines 2017 edited by the Japan esophageal society: part 2. Esophagus. 2019;16:25–43.
Hirano Y, Fujita T, Sato K, et al. Totally mechanical collard technique for cervical esophagogastric anastomosis redues stricture formation compared with circular stapled anastomosis. World J Surg. 2020;44:4175–83.
Gomez-Perez SL, Haus JM, Sheean P, et al. Measuring abdominal circumference and skeletal muscle from a single cross-sectional computed tomography image. A step-by-step guide for clinicians using National Institutes of Health ImageJ. J Parenter Enteral Nutr. 2016;40:308–18.
Nishikawa H, Shiraki M, Hiramatsu A, Moriya K, Hino K, Nishiguchi. Japan Society of Hepatology guidelines for sarcopenia in liver disease (1st edition): Recommendation from the working group for creation of sarcopenia assessment criteria. Hepatol Res. 2016;46:951–63.
Maggio M, Ceda GP, Ticinesi A, et al. Instrumental and non-instrumental evaluation of 4-meter walking speed in older individuals. PLoS ONE. 2016;11: e0153583.
Speyer R, Baijens L, Heijnen M, Zwijnenberg I. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia. 2010;25:40–65.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85:1001–5.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Morita M, Nakanoko T, Kubo N, et al. Two-stage operation for high-risk patients with thoracic esophageal cancer: an old operation revisited. Ann Surg Oncol. 2011;18:2613–21.
Daiko H, Oguma J, Fujiwara H, et al. Novel universally applicable technique for performing bilateral transcervical mediastinoscopic-assisted transhiatal laparoscopic esophagectomy: a truly minimally invasive procedure. Surg Endosc. 2021;35:5186–92.
Wakabayashi H. Presbyphagia and sarcopenic dysphagia: Association between aging, sarcopenia, and deglutition disorders. J Frailty Aging. 2014;3:97–103.
Manini TM, Clark BC. Dynapenia and aging: an update. J Gerontol A Biol Sci Med Sci. 2012;67:28–40.
Yasuda T, Nakamori Y, Shiraishi O, et al. Decreased preoperative plasma substance P concentration is likely associated with postoperative silent aspiration after esophagectomy. Esophagus. 2014;11:99–107.
Leder SB, Sasaki CT, Burrell MI. Fiberoptic endoscopic evaluation of dysphagia to identify silent aspiration. Dysphagia. 1998;13:19–21.
Boden I, Skinner EH, Browning L, et al. Preoperative physiotherapy for the prevention of respiratory complications after upper abdominal surgery: pragmatic, double blinded, multicentre randomised controlled trial. BMJ. 2018;360: j5916.
Yokoi A, Ekuni D, Yamanaka R, Hata H, Shirakawa Y, Morita M. Change in tongue pressure and the related factors after esophagectomy: a short-term, longitudinal study. Esophagus. 2019;16:300–8.
Acknowledgements
We thank Jane Charbonneau, DVM, from Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript.
Funding
This study was not supported by any funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
The National Cancer Center Institutional Review Board approved the current observational study (approval number: 2017–061), and the need for informed consent was waived owing to the retrospective nature of the study.
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kurita, D., Utsunomiya, D., Kubo, K. et al. Handgrip strength predicts early postoperative dysphagia after thoracoscopic–laparoscopic esophagectomy in male patients with esophageal cancer. Esophagus 19, 586–595 (2022). https://doi.org/10.1007/s10388-022-00925-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-022-00925-6