Abstract
Background
Postoperative pneumonia is the most common complication after esophagectomy and is closely associated with swallowing dysfunction and silent aspiration. Silent aspiration in the elderly is associated with decreased secretion of substance P (SP), which controls the swallowing and cough reflexes. The majority of patients with esophageal cancer are elderly. We hypothesized that surgical stress would decrease SP secretion, thereby increasing the risk of postoperative aspiration after esophagectomy, and prospectively investigated.
Methods
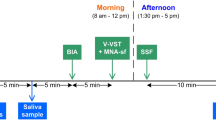
Thirty patients with esophageal cancer scheduled to undergo esophagectomy were enrolled in the study. Plasma and salivary SP concentrations and cough reflex sensitivity were measured before surgery and on postoperative days 2 and 7 to examine the association with postoperative aspiration.
Results
Postoperative silent aspiration was observed in 6 patients, 4 of whom developed pneumonia. Plasma SP concentration did not change significantly during the perioperative period. Salivary SP concentration and cough reflex sensitivity could not be measured in nearly one-third of patients because of postoperative dry mouth and unwillingness of patients to undergo measurement, respectively; thus, these perioperative changes could not be assessed. Preoperative plasma and salivary SP concentrations had a significant association with postoperative aspiration on univariate analysis and multivariate logistic regression analysis using variables selected by stepwise forward selection identified preoperative plasma SP concentration as the only significant risk factor for postoperative aspiration (p = 0.023).
Conclusion
Definitive results supporting our hypothesis could not be obtained. However, multivariate analysis suggested that decreased preoperative plasma SP concentration is likely associated with postoperative silent aspiration after esophagectomy.


Similar content being viewed by others
References
Ferguson MK, Durkin AE. Preoperative prediction of the risk of pulmonary complications after esophagectomy for cancer. J Thorac Cardiovasc Surg. 2002;123:661–9.
Atkins BZ, Shah AS, Hutcheson KA, et al. Reducing hospital morbidity and mortality following esophagectomy. Ann Thorac Surg. 2004;78:1170–6.
Berry MF, Atkins BZ, Tong BC, Harpole DH, D’Amico TA, Onaitis MW. A comprehensive evaluation for aspiration after esophagectomy reduces the incidence of postoperative pneumonia. J Thorac Cardiovasc Surg. 2010;140:1266–71.
Biere SSA, Henegouwen MIB, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicenter, open-label, randomized controlled trial. Lancet. 2012;379:1887–92.
Whooley BP, Law S, Murthy SC, Alexandrou A, Wong J. Analysis of reduced death and complication rates after esophageal resection. Ann Surg. 2001;233:338–44.
Pikus L, Levine MS, Yang YX, et al. Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. Am J Roentgenol. 2003;180:1613–6.
Leder SB, Bayar S, Sasaki CT, Salem RR. Fiberoptic endoscopic evaluation of swallowing in assessing aspiration after transhiatal esophagectomy. J Am Coll Surg. 2007;205:581–5.
Heitmiler RF, Jones B. Transient diminished airway protection after transhiatal esophagectomy. Am J Surg. 1991;162:442–6.
Easterling CS, Bousamra M II, Lang IM, et al. Pharyngeal dysphagia in postesophagectomy patients; correlation with deglutitive biomechanics. Ann Thorac Surg. 2000;69:989–92.
Hambraeus GM, Ekberg O, Fletcher R. Pharyngeal dysfunction after total and subtotal oesophagectomy. Acta Radiol. 1987;28:409–13.
Yasuda T, Yano M, Miyata H, et al. Evaluation of dysphagia and diminished airway protection after three-field esophagectomy and a remedy. World J Surg. 2013;37:416–23.
Nakazawa H, Sekizawa K, Ujiie Y, Sasaki H, Takishima T. Risk of aspiration pneumonia in the elderly. Chest. 1993;103:1636–7.
Field LH, Weiss CJ. Dysphagia with head injury. Brain Inj. 1989;3:19–26.
Arai T, Yoshimi N, Fujiwara H, Sekizawa K. Serum substance P concentrations and silent aspiration in elderly patients with stroke. Neurology. 2003;61:1625–6.
Nakagawa T, Ohrui T, Sekizawa K, Sasaki H. Sputum substance P in aspiration pneumonia. Lancet. 1995;345:1447.
Sasaki H, Sekizawa K, Yanai M, Arai H, Yamaya M, Ohrui T. New strategies for aspiration pneumonia. Intern Med. 1997;36:851–5.
Yamaya M, Yanai M, Ohrui T, Arai H, Sasaki H. Interventions to prevent pneumonia among older adults. J Am Gariatr Soc. 2001;49:85–90.
Ohrui T. Preventive strategies for aspiration pneumonia in elderly disabled persons. Tohoku J Exp Med. 2005;207:3–12.
Sekizawa K, Ujiie Y, Itabashi S, Sasaki H, Takishima T. Lack of cough reflex in aspiration pneumonia. Lancet. 1990;335:1228–9.
Jia XY, Sekizawa K, Ohrui T, Nakayama K, Sasaki H. Dopamine D1 receptor antagonist inhibits swallowing reflex in guinea pigs. Am J Physiol. 1998;274:76–80.
Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
Shiozaki H, Yano M, Tsujinaka M, et al. Lymph node metastasis along the recurrent nerve chain is an indication for cervical lymph node dissection in thoracic esophageal cancer. Dis Esophagus. 2001;14:191–6.
Takeyama M, Mori K, Takayama F, Kondo K, Kitagawa K, Fujii N. Enzyme immunoassay of a substance P-like immunoreactive substance in human plasma and saliva. Chem Pharm Bull. 1990;38:3494–6.
Morice AH, Fontana GA, Belvisi MG, et al. ERS guidelines on the assessment of cough. Eur Respir J. 2007;29:1256–76.
Ebihara S, Saito H, Kanda A, et al. Impaired efficacy of cough in patients with parkinson disease. Chest. 2003;124:1009–15.
Nakagawa T, Sekizawa K, Arai H, Kikuchi R, Manabe K, Sasaki H. High incidence of pneumonia in elderly patients with basal ganglia infarction. Arch Intern Med. 1997;157:321–4.
Nakagawa T, Sekizawa K, Nakajoh K, Tanji H, Arai H, Sasaki H. Silent cerebral infarction: a potential risk for pneumonia in the elderly. J Intern Med. 2000;247:255–9.
Graybiel AM. Neurotransmitters and neuromodulators in the basal ganglia. Trends Neurosci. 1990;13:244–54.
Katsumata U, Sekizawa K, Ebihara T, Sasaki H. Aging effects on cough reflex. Chest. 1995;107:290–1.
Kobayashi H, Sekizawa K, Sasaki H. Aging effects on swallowing reflex. Chest. 1997;111:1446.
Ebihara S, Ebihara T, Kanezaki M, et al. Aging deteriorated perception of urge-to-cough without changing cough reflex threshold to citric acid in female never-smoker. Cough. 2011;7:3.
Ozawa S, Tachimori Y, Baba H, et al. Comprehensive registry of esophageal cancer in Japan, 2003. The Registration committee for esophageal cancer, the Japan Esophageal Society. 2011 Esophagus;8:9–29.
Uehara T, Tabuchi M, Mori E. Risk factors for silent cerebral infarcts in subcortical white matter and basal ganglia. Stroke. 1999;30:378–82.
Ebihara S, Ebihara T, Kohzuki M. Effect of aging on cough and swallowing reflexes: implications for preventing aspiration pneumonia. Lung. 2012;190:29–33.
Malandraki GA, Perlman AL, Karampinos DC, Sutton BP. Reduced somatosensory activations in swallowing with age. Hum Brain Mapp. 2011;32:730–43.
Sekizawa K, Matsui T, Nakagawa T, Nakayama K, Sasaki H. ACE inhibitors and pneumonia. Lancet. 1998;352:1069.
Arai T, Yasuda Y, Toshima S, Yoshimi N, Kashiki Y. ACE inhibitors and pneumonia in elderly people. Lancet. 1998;352:1937–8.
Ebihara T, Sekizawa K, Nakazawa H, Sasaki H. Capsaicin and swallowing reflex. Lancet. 1993;341:432.
Nakagawa T, Wada H, Sekizawa K, Arai H, Sasaki H. Amantadine and pneumonia. Lancet. 1999;353:1157.
Yamaya M, Yanai M, Ohrui T, Arai H, Sekizawa K, Sasaki H. Antithrombotic therapy for prevention of pneumonia. J Am Geriatr Soc. 2001;49:687–8.
Acknowledgments
This work was supported as a Grant-in-Aid for Scientific Research (C) by Japan Society for Promotion of Science (JSPS) KAKENHI Grant Number 21591716. The authors thank lecturer Yasutaka Chiba from the division of Biostatics, Clinical Research Center, Kinki University Faculty of Medicine for advice regarding statistical analysis.
Ethical Statement
This study was approved by the Institutional Review Board of Ethics Committee and was conducted in accordance with Helsinki Declaration of 1975, as revised in 2000 and 2008, and informed consent was obtained from all patients. Those were involved in the prerequisites for publication in the certification form as No. 5 item and all authors certified and put their own signatures on the form.
Conflict of interest
There are no financial or other relations that could lead to a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yasuda, T., Nakamori, Y., Shiraishi, O. et al. Decreased preoperative plasma substance P concentration is likely associated with postoperative silent aspiration after esophagectomy. Esophagus 11, 99–107 (2014). https://doi.org/10.1007/s10388-014-0415-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-014-0415-y