Abstract
Objective
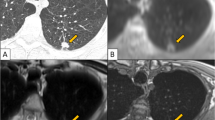
This study investigated ultrashort echo time (UTE) sequences in 1.5 T magnetic resonance imaging (MRI) for small lung nodule detection.
Materials and methods
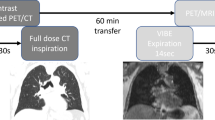
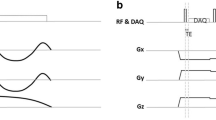
A total of 120 patients with 165 small lung nodules before video-associated thoracoscopic resection were enrolled. MRI sequences included conventional volumetric interpolated breath-hold examination (VIBE, scan time 16 s), spiral UTE (TE 0.05 ms) with free-breathing (scan time 3.5–5 min), and breath-hold sequences (scan time 20 s). Chest CT provided a standard reference for nodule size and morphology. Nodule detection sensitivity was evaluated on a lobe-by-lobe basis.
Results
The nodule detection rate was significantly higher in spiral UTE free-breathing (> 78%, p < 0.05) and breath-hold sequences (> 75%, p < 0.05) compared with conventional VIBE (> 55%), reaching 100% when nodule size was > 16 mm, and reaching 95% when nodules were in solid morphology, regardless of size. The inter-sequence reliability between free-breathing and breath-hold spiral UTE was good (κ > 0.80). Inter-reader agreement was also high (κ > 0.77) for spiral UTE sequences. Nodule size measurements were consistent between CT and spiral UTE MRI, with a minimal bias up to 0.2 mm.
Discussion
Spiral UTE sequences detect small lung nodules that warrant surgery, offers realistic scan times for clinical work, and could be implemented as part of routine lung MRI.





Similar content being viewed by others
References
National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365:395–409
Johnson KM, Fain SB, Schiebler ML, Nagle S (2013) Optimized 3D ultrashort echo time pulmonary MRI. Magn Reson Med 70:1241–1250
Ohno Y, Nishio M, Koyama H et al (2014) Pulmonary 3 T MRI with ultrashort TEs: influence of ultrashort echo time interval on pulmonary functional and clinical stage assessments of smokers. J Magn Reson Imaging 39:988–997
Wolfram F, Böttcher J, Lesser TG (2020) MR imaging of pulmonary lung nodules during one lung flooding: first morphological evaluation using an ex vivo human lung model. Magn Reson Mater Phy. https://doi.org/10.1007/s10334-020-00826-8
Yi CA, Jeon TY, Lee KS et al (2007) 3-T MRI: usefulness for evaluating primary lung cancer and small nodules in lobes not containing primary tumors. AJR Am J Roentgenol 189:386–392
Kumar S, Rai R, Stemmer A et al (2017) Feasibility of free breathing lung MRI for radiotherapy using non-Cartesian k-space acquisition schemes. Br J Radiol 90:20170037
Plathow C, Schoebinger M, Herth F, Tuengerthal S, Meinzer HP, Kauczor HU (2009) Estimation of pulmonary motion in healthy subjects and patients with intrathoracic tumors using 3D-dynamic MRI: initial results. Korean J Radiol 10:559–567
Wu LM, Xu JR, Hua J et al (2013) Can diffusion-weighted imaging be used as a reliable sequence in the detection of malignant pulmonary nodules and masses? Magn Reson Imaging 31:235–246
Biederer J, Ohno Y, Hatabu H et al (2017) Screening for lung cancer: does MRI have a role? Eur J Radiol 86:353–360
Dournes G, Grodzki D, Macey J et al (2016) Quiet submillimeter MR imaging of the lung is feasible with a PETRA sequence at 1.5 T. Radiology 279:328
Gai ND, Malayeri AA, Bluemke DA (2017) Long T2 suppression in native lung 3-D imaging using k-space reordered inversion recovery dual-echo ultrashort echo time MRI. Magn Reson Mater Phy 30:387–395
Ma W, Sheikh K, Svenningsen S et al (2015) Ultra-short echo-time pulmonary MRI: evaluation and reproducibility in COPD subjects with and without bronchiectasis. J Magn Reson Imaging 41:1465–1474
Wielputz MO, Lee HY, Koyama H et al (2018) Morphologic characterization of pulmonary nodules with ultrashort TE MRI at 3T. AJR Am J Roentgenol 210:1216–1225
Burris NS, Johnson KM, Larson PE et al (2016) Detection of small pulmonary nodules with ultrashort echo time sequences in oncology patients by using a PET/MR system. Radiology 278:239–246
Ohno Y, Koyama H, Yoshikawa T et al (2011) T2* measurements of 3-T MRI with ultrashort TEs: capabilities of pulmonary function assessment and clinical stage classification in smokers. AJR Am J Roentgenol 197:W279–W285
Cha MJ, Park HJ, Paek MY et al (2018) Free-breathing ultrashort echo time lung magnetic resonance imaging using stack-of-spirals acquisition: a feasibility study in oncology patients. Magn Reson Imaging 51:137–143
Elia S, Loprete S, De Stefano A et al (2019) Does aggressive management of solitary pulmonary nodules pay off? Breathe 15:15–23
Gould MK, Donington J, Lynch WR et al (2013) Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143:e93S–e120S
Chen CY, Chen CH, Shen TC et al (2016) Lung cancer screening with low-dose computed tomography: experiences from a tertiary hospital in Taiwan. J Formos Med Assoc 115:163–170
Lin MW, Tseng YH, Lee YF et al (2016) Computed tomography-guided patent blue vital dye localization of pulmonary nodules in uniportal thoracoscopy. J Thorac Cardiovasc Surg 152:535–544.e2
Lustig M, Pauly JM (2010) SPIRiT: iterative self-consistent parallel imaging reconstruction from arbitrary k-space. Magn Reson Med 64:457–471
Ohno Y, Koyama H, Yoshikawa T et al (2017) Standard-, reduced-, and no-dose thin-section radiologic examinations: comparison of capability for nodule detection and nodule type assessment in patients suspected of having pulmonary nodules. Radiology 284:562–573
Bae K, Jeon KN, Hwang MJ et al (2019) Comparison of lung imaging using three-dimensional ultrashort echo time and zero echo time sequences: preliminary study. Eur Radiol 29:2253–2262
Sommer G, Tremper J, Koenigkam-Santos M et al (2014) Lung nodule detection in a high-risk population: comparison of magnetic resonance imaging and low-dose computed tomography. Eur J Radiol 83:600–605
Herrmann KH, Krämer M, Reichenbach JR (2016) Time efficient 3D radial UTE sampling with fully automatic delay compensation on a clinical 3T MR scanner. PLoS ONE 11:e0150371
Qian Y, Williams AA, Chu CR et al (2012) High-resolution ultrashort echo time (UTE) imaging on human knee with AWSOS sequence at 3.0 T. J Magn Reson Imaging 35:204–210
Shin T, Lustig M, Nishimura DG, Hu BS (2014) Rapid single-breath-hold 3D late gadolinium enhancement cardiac MRI using a stack-of-spirals acquisition. J Magn Reson Imaging 40:1496–1502
Koyama H, Ohno Y, Seki S et al (2013) Magnetic resonance imaging for lung cancer. J Thorac Imaging 28:138–150
Cieszanowski A, Lisowska A, Dabrowska M et al (2016) MR imaging of pulmonary nodules: detection rate and accuracy of size estimation in comparison to computed tomography. PLoS ONE 11:e0156272
Meier-Schroers M, Homsi R, Skowasch D et al (2018) Lung cancer screening with MRI: results of the first screening round. J Cancer Res Clin Oncol 144:117–125
Callister ME, Baldwin DR, Akram AR et al (2015) British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax 70(Suppl 2):ii1–ii54
MacMahon H, Naidich DP, Goo JM et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology 284:228–243
Chang EY, Du J, Chung CB (2015) UTE imaging in the musculoskeletal system. J Magn Reson Imaging 41:870–883
Jin S, Zhang B, Zhang L et al (2018) Lung nodules assessment in ultra-low-dose CT with iterative reconstruction compared to conventional dose CT. Quant Imaging Med Surg 8:480–490
Bianchi A, Dufort S, Lux F et al (2013) Quantitative biodistribution and pharmacokinetics of multimodal gadolinium-based nanoparticles for lungs using ultrashort TE MRI. Magn Reson Mater Phys Biol Med 27:303–316
Koenigkam-Santos M, Optazaite E, Sommer G et al (2015) Contrast-enhanced magnetic resonance imaging of pulmonary lesions: description of a technique aiming clinical practice. Eur J Radiol 84:185–192
Hirsch FW, Sorge I, Vogel-Claussen J et al (2020) The current status and further prospects for lung magnetic resonance imaging in pediatric radiology. Pediatr Radiol 50:734–749
Takahashi M, Togao O, Obara M et al (2010) Ultra-short echo time (UTE) MR imaging of the lung: comparison between normal and emphysematous lungs in mutant mice. J Magn Reson Imaging 32:326–333
Ciet P, Tiddens H, Wielopolski PA et al (2015) Magnetic resonance imaging in children: common problems and possible solutions for lung and airways imaging. Pediatr Radiol 45:1901–1915
Oudkerk M, Devaraj A, Vliegenthart R et al (2017) European position statement on lung cancer screening. Lancet Oncol 18:e754–e766
Acknowledgements
We would like to acknowledge Joseph Pfeuffer (Siemens Healthcare) for his contributions to the development of the Spiral UTE VIBE sequence. We are thankful to the doctors, nurses, healthcare providers, and other sources of health information who contributed to this study.
Funding
This work was supported by the Ministry of Science and Technology Taiwan (Grant Number: Contract No. MST 107-2314-B-002-225-MY2) and the National Taiwan University Hospital (grant number: NTUH107-M4007, NTUH 108-N4353, NTUH 109-N4547).
Author information
Authors and Affiliations
Contributions
Y-SH: study conception and design, acquisition of data, formal analysis, funding acquisition, methodology, drafting of manuscript. EN: acquisition of data, formal analysis, investigation, methodology, drafting of manuscript. M-YMS: interpretation of data, investigation, software. TB: formal analysis, software. H-HH: investigation, methodology. J-YS: methodology, project administration. J-SC: conceptualization, critical revision, resources, supervision, validation. Y-CC: conceptualization, funding acquisition, investigation, methodology, resources, writing—review and editing, critical revision.
Corresponding author
Ethics declarations
Conflict of interest
Emi Niisato and Thomas Benkert are employees of Siemens. There was no direct or indirect funding support from Siemens during the study for the prototype ultrashort echo time sequences. The other authors indicate no potential conflicts of interest.
Ethical approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by National Taiwan University Hospital Research Ethics Committee (approval number: 201707032RINB).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, YS., Niisato, E., Su, MY.M. et al. Detecting small pulmonary nodules with spiral ultrashort echo time sequences in 1.5 T MRI. Magn Reson Mater Phy 34, 399–409 (2021). https://doi.org/10.1007/s10334-020-00885-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-020-00885-x