Abstract
Purpose
To examine the efficacy and feasibility of T2-weighted whole-spine sagittal magnetic resonance imaging (MRI) screening for all patients who undergo MRI of the lumbar spine for any indication.
Methods
A review of 1145 consecutive T2-weighted whole-spine sagittal MRI screening sequences performed for lumbar spine imaging was undertaken for the purposes of documenting the incidence and clinical significance of thoracic and cervical spine incidental findings, as well as to establish correlation between these pathologies and those found in the lumbar spine.
Results
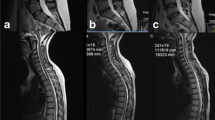
Out of the 1145 patients included in the study, 103 (9%) patients had incidental findings thought to be significant. These findings included cervical spinal stenosis (n = 85), thoracic disc herniation (n = 9), syrinx (n = 5), intradural tumor (n = 2), and signal changes within the spinal cord (n = 2). In follow-up exams, 35 patients had clinically significant findings which included cervical myelopathy (n = 25), thoracic myelopathy (n = 3), syrinx (n = 5) and intradural tumor (n = 2). Among the 172 patients presenting with lumbar spinal stenosis, 42 (24.4%) had such incidental findings, and of those 41 (23.8%) had cervical stenosis with spinal cord compression (p < 0.0001).
Conclusion
T2-weighted whole-spine sagittal screening is useful in demonstrating clinically relevant incidental findings in any patients undergoing MRI of the lumbar spine. There is a statistically significant correlation between lumbar spinal stenosis and cervical spinal stenosis with spinal cord compression.


Similar content being viewed by others
References
Schaefer DM, Flanders A, Northrup BE, Doan HT, Osterholm JL (1989) Magnetic resonance imaging of acute cervical spine trauma. Correlation with severity of neurologic injury. Spine (Phila Pa 1976) 14:1090–1095
Flanders AE, Spettell CM, Friedman DP, Marino RJ, Herbison GJ (1999) The relationship between the functional abilities of patients with cervical spinal cord injury and the severity of damage revealed by MR imaging. AJNR Am J Neuroradiol 20:926–934
Yamashita Y, Takahashi M, Matsuno Y et al (1990) Chronic injuries of the spinal cord: assessment with MR imaging. Radiology 175:849–854
Kanna RM, Kamal Y, Mahesh A, Venugopal P, Shetty AP, Rajasekaran S (2017) The impact of routine whole spine MRI screening in the evaluation of spinal degenerative diseases. Eur Spine J 26:1993–1998
Lian J, Levine N, Cho W (2018) A review of lumbosacral transitional vertebrae and associated vertebral numeration. Eur Spine J 27:995–1004
Althoff CE, Appel H, Rudwaleit M, Sieper J, Eshed I, Hermann KG (2007) Whole-body MRI as a new screening tool for detecting axial and peripheral manifestations of spondyloarthritis. Ann Rheum Dis 66:983–985
Green RA, Saifuddin A (2004) A Whole spine MRI in the assessment of acute vertebral body trauma. Skeletal Radiol 33:129–135
Kaila R, Malhi AM, Mahmood B, Saifuddin A (2007) The incidence of multiple level noncontiguous vertebral tuberculosis detected using whole spine MRI. J Spinal Disord Tech 20:78–81
Schmitz A, Kandyba J, Koenig R, Jaeger UE, Gieseke J, Schmitt O (2001) A new method of MR total spine imaging for showing the brace effect in scoliosis. J Orthop Sci 6:316–319
Nakanishi K, Kobayashi M, Nakaguchi K, Kyakuno M, Hashimoto N, Onishi H et al (2007) Whole-body MRI for detecting metastatic bone tumor: diagnostic value of diffusion-weighted images. Magn Reson Med Sci 6:147–155
Steinborn MM, Heuck AF, Tiling R, Bruegel M, Gauger L, Reiser MF (1999) Whole-body bone marrow MRI in patients with metastatic disease to the skeletal system. J Comput Assist Tomogr 23:123–129
Han IH, Suh SH, Kuh SU, Chin DK, Kim KS (2010) Types and prevalence of coexisting spine lesions on whole spine sagittal MR images in surgical degenerative spinal diseases. Yonsei Med J 51(3):414–420
Nagata K, Yoshimura N, Muraki S, Hashizume H, Ishimoto Y, Yamada H, Takiguchi N, Nakagawa Y, Oka H, Kawaguchi H, Nakamura K, Akune T, Yoshida M (2012) Prevalence of cervical cord compression and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study. Spine 37:1892–1898
Wagner SC, Morrison WB, Carrino JA, Schweitzer ME, Nothnagel H (2002) Picture archiving and communication system: effect on reporting of incidental findings. Radiology 225:500–505
Park HJ, Jeon YH, Rho MH, Lee EJ, Park NH, Park SI, Jo JH (2011) Incidental findings of the lumbar spine at MRI during herniated intervertebral disk disease evaluation. AJR Am J Roentgenol 196:1151–1155
Hilton B, Tempest-Mitchell J, Davies B, Kotter M (2018) Assessment of degenerative cervical myelopathy differs between specialists and may influence time to diagnosis and clinical outcomes. PLoS ONE 17:13
Milligan J, Ryan K, Fehlings M, Bauman C (2019) Degenerative cervical myelopathy: diagnosis and management in primary care. Can Fam Physician 65:619–624
Adamova B, Bednarik J, Andrasinova T, Kovalova I, Kopacik R, Jabornik M, Kerkovsky M, Jakubcova B, Jarkovsky J (2015) Does lumbar spinal stenosis increase the risk of spondylotic cervical spinal cord compression? Eur Spine J 24:2946–2953
Lee SH, Kim KT, Suk KS, Lee JH, Shin JH, So DH, Kwack YH (2010) Asymptomatic cervical cord compression in lumbar spinal stenosis patients: a whole spine magnetic resonance imaging study. Spine (Phila Pa 1976) 35:2057–2063
Bhandutia A, Brown L, Nash A, Bussey I, Shasti M, Koh E, Banagan K, Ludwig S, Gelb D (2019) Delayed diagnosis of tandem spinal stenosis: a retrospective institutional review. Int J Spine Surg 13:283–288
Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S (1990) Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am 72:1178–1184
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by YS, ST and TG. The first draft of the manuscript was written by YS and TG and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Due to the retrospective nature of the study, a waiver from informed consent was given by the IRB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smorgick, Y., Granek, T., Mirovsky, Y. et al. Routine sagittal whole-spine magnetic resonance imaging in finding incidental spine lesions. Magn Reson Mater Phy 34, 421–426 (2021). https://doi.org/10.1007/s10334-020-00882-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-020-00882-0