Abstract
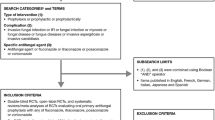
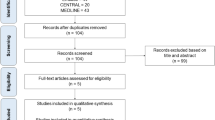
Acute leukemias are complex diseases to treat and have a high mortality rate. The immunosuppression caused by chemotherapy also causes the patient to become susceptible to a variety of infections, including invasive fungal infections. Protocols established in many countries attempt to prevent these infections through the use of pharmacological antifungal prophylaxis. This systematic review and meta-analysis investigates the existing evidence for the use of antifungal prophylaxis in patients undergoing induction chemotherapy for acute leukemia, and how prophylaxis can affect treatment response and mortality. Through the use of a population-variable-outcome strategy, keywords were utilized to search online databases. The included studies were selected and the data was collected to develop descriptive results for all studies, and, for studies that met the criteria, a meta-analysis of the Relative Risk (RR) was analyzed for infection rates, in-hospital mortality, and complete remission. A total of 33 studies were included in this systematic review, with most studies presenting positive results (n = 28/33) from the use of antifungal prophylaxis. Using a random effects model, the pooled results of the meta-analysis presented lower invasive fungal infections in AML (RR: 0.527 (95% CI: 0.391; 0.709). p < 0.001). p < 0.001) and ALL (RR: 0.753 (95% CI: 0.574; 0.988). p = 0.041). when antifungal prophylaxis was used. No discernible difference was encountered in the rate of complete remission when using prophylaxis. Antifungal prophylaxis provides a lower risk of invasive fungal infections and in-hospital mortality in acute leukemia patients undergoing induction chemotherapy.







Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics. CA Cancer J Clin Wiley. 2022;72:7–33.
Roloff GW, Odenike O, Bajel A, et al. Contemporary approach to acute myeloid leukemia therapy in 2022. Am Soc Clin Oncol Educ Book. 2022;42:1–16.
Elfaituri MK, Morsy S, Tawfik GM, et al. Incidence of Infection-related mortality in cancer patients: trend and survival analysis. Proc Am Soc Clin Oncol. 2019;37:e23095–e23095.
Zimmer AJ, Freifeld AG. Optimal management of neutropenic fever in patients with cancer. J Oncol Pract. 2019;15:19–24.
Mendonça A, Santos H, Franco-Duarte R, et al. Fungal infections diagnosis—past, present and future. Res Microbiol. 2022;173:103915.
Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54.
Auberger J, Lass-Flörl C, Ulmer H, et al. Significant alterations in the epidemiology and treatment outcome of invasive fungal infections in patients with hematological malignancies. Int J Hematol Int J Hematol. 2008;88:508–15.
Hammond SP, Marty FM, Bryar JM, et al. Invasive fungal disease in patients treated for newly diagnosed acute leukemia. Am J Hematol Am J Hematol. 2010;85:695–9.
Pagano L, Mayor S. Invasive fungal infections in high-risk patients: report from TIMM-8 2017. Future Sci OA. Future Science Group; 2018;4.
Maertens JA, Girmenia C, Brüggemann RJ, et al. European guidelines for primary antifungal prophylaxis in adult haematology patients: summary of the updated recommendations from the European conference on infections in leukaemia. J Antimicrob Chemother. 2018;73:3221–30.
Page MJ, McKenzie JE, Bossuyt PM, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. Br Med J. 2020;2021:372.
JBI Manual for Evidence Synthesis. JBI Manual for Evidence Synthesis. JBI; 2020.
Board PATE. Adult Acute Lymphoblastic Leukemia Treatment (PDQ®). Bethesda, MD. National Cancer Institute (US); 2021.
{Microsoft Corporation}. Microsoft excel. 2018.
Owen RK, Bradbury N, Xin Y, et al. MetaInsight: an interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Res Synth Methods. 2019;10(4):569–81.
The Endnote Team. Endnote. Philadelphia, PA: Clarivate; 2013.
Mattiuzzi GN, Estey E, Raad I, et al. Liposomal amphotericin B versus the combination of fluconazole and itraconazole as prophylaxis for invasive fungal infections during induction chemotherapy for patients with acute myelogenous leukemia and myelodysplastic syndrome. Cancer. 2003;97:450–6.
Mattiuzzi GN, Kantarjian H, O’Brien S, et al. Intravenous itraconazole for prophylaxis of systemic fungal infections in patients with acute myelogenous leukemia and high-risk myelodysplastic syndrome undergoing induction chemotherapy. Cancer. 2004;100:568–73.
Mattiuzzi GN, Alvarado G, Giles FJ, et al. Open-label, randomized comparison of itraconazole versus caspofungin for prophylaxis in patients with hematologic malignancies. Antimicrob Agents Chemother Antimicrob Agents Chemother. 2006;50:143–7.
Wetzstein GA, George TJ, Sharifi M, et al. Comparable efficacy and safety with voriconazole or posaconazole as primary antifungal prophylaxis in acute myeloid leukemia (AML) patients receiving induction chemotherapy. Blood Am Soc Hematol. 2009;114:2059–2059.
Vehreschild JJ, Rüping MJGT, Wisplinghoff H, et al. Clinical effectiveness of posaconazole prophylaxis in patients with acute myelogenous leukaemia (AML): a 6 year experience of the Cologne AML cohort. J Antimicrob Chemother J Antimicrob Chemother. 2010;65:1466–71.
Girmenia C, Frustaci AM, Gentile G, et al. Posaconazole prophylaxis during front-line chemotherapy of acute myeloid leukemia: a single center real life experience. Haematologica. 2011;96:110.
Mattiuzzi GN, Cortes J, Alvarado G, et al. Efficacy and safety of intravenous voriconazole and intravenous itraconazole for antifungal prophylaxis in patients with acute myelogenous leukemia or high-risk myelodysplastic syndrome. Support Care Cancer Support Care Cancer. 2011;19:19–26.
Michallet M, Sobh M, Morisset S, et al. Risk factors for invasive aspergillosis in acute myeloid leukemia patients prophylactically treated with posaconazole. Med Mycol. 2011;49:681–7.
Fisher BT, Kavcic M, Li Y, et al. Antifungal prophylaxis associated with decreased induction mortality rates and resources utilized in children with new-onset acute myeloid leukemia. Clin Infect Dis. 2014;58:502–8.
Minetto P, Guolo F, Pastori G, et al. Posaconazole as primary prophylaxis reduces invasive fungal infections in AML patients: a single centre matched paired analysis. Haematologica. 2015;100:717–8.
Cho SY, Lee DG, Choi SM, et al. Posaconazole for primary antifungal prophylaxis in patients with acute myeloid leukaemia or myelodysplastic syndrome during remission induction chemotherapy: a single-centre retrospective study in Korea and clinical considerations. Mycoses. 2015;58:565–71.
Devanlay C, Tavernier-Tardy E, Bourmaud A, et al. Impact of fluconazole versus posaconazole prophylaxis on the incidence of fungal infections in patients receiving induction chemotherapy for acute myeloid leukemia. Biomed J. 2015;38:235–43.
Schrenk KG, Schnetzke U, Stegemann K, et al. Efficacy of antifungal prophylaxis with oral suspension posaconazole during induction chemotherapy of acute myeloid leukemia. J Cancer Res Clin Oncol. 2015;141:1661–8.
Dahlén T, Kalin M, Cederlund K, et al. Decreased invasive fungal disease but no impact on overall survival by posaconazole compared to fluconazole prophylaxis: a retrospective cohort study in patients receiving induction therapy for acute myeloid leukaemia/myelodysplastic syndromes. Eur J Haematol Eur J Haematol. 2016;96:175–80.
Venton G, Adam H, Colle J, et al. Micafungin as primary antifungal prophylaxis in patients presenting with acute myeloid leukemia. Med Mal Infect Med Mal Infect. 2016;46:226–9.
Shah A, Ganesan P, Radhakrishnan V, et al. Voriconazole is a safe and effective anti-fungal prophylactic agent during induction therapy of acute myeloid leukemia. Indian J Med Paediatr Oncol. 2016;37:53.
Bansal D, Seth T, Kumar R, et al. Efficacy of posaconazole prophylaxis in patients with acute myeloid leukemia undergoing induction chemotherapy: an observational study in resource limited settings. Indian J Hematol Blood Transfus. 2018;34:460.
Chen T-C, Wang RC, Lin Y-H, et al. Posaconazole for the prophylaxis of invasive aspergillosis in acute myeloid leukemia: Is it still useful outside the clinical trial setting? Ther Adv Hematol. 2020;11:2040620720965846–2040620720965846.
Hsu A, Matera R, Reagan JL, et al. Survival benefits from antifungal prophylaxis and a dedicated inpatient malignant hematology service during induction chemotherapy for acute myeloid leukemia. Blood. 2019;134:3436.
Hsu A, Matera R, Vieira K, et al. Antifungal prophylaxis during 7 + 3 induction chemotherapy for acute myeloid leukemia is associated with improved survival, in a setting with low incidence of invasive mold infections. Support Care Cancer. 2020;29:707–12.
Mishra P, Agrawal N, Bhurani D, et al. Invasive fungal infections in patients with acute myeloid leukemia undergoing intensive chemotherapy. Indian J Hematol Blood Transfus. 2020;36:64–70.
Signorelli J, Lei M, Lam J, et al. Incidence of invasive fungal infections in acute myeloid leukemia without antifungal prophylaxis. Clin Lymphoma Myeloma Leuk. 2020;20:e883–9.
Bekadja MA, Michallet M, Benzineb B, et al. Evaluation of posaconazole for primary prophylaxis of IFI in acute myeloid leukemia under intensive induction chemotherapy comparative real life study with fluconazole in two hematological centers in Algeri. Asian Pac J Cancer Biol. 2021;6:249–54.
Bose P, McCue D, Wurster S, et al. Isavuconazole as primary antifungal prophylaxis in patients with acute myeloid leukemia or myelodysplastic syndrome: an open-label, prospective, phase 2 study. Clin Infect Dis Clin Infect Dis. 2021;72:1755–63.
Yang E, Choi EJ, Park HS, et al. Comparison of invasive fungal diseases between patients with acute myeloid leukemia receiving posaconazole prophylaxis and those not receiving prophylaxis: a single-center, observational, case-control study in South {Korea}. Medicine (Baltimore). 2021;100:e25448.
Cornely O, Leguay T, Maertens J, et al. A double-blind, multicentre, randomised, placebo-controlled study to assess the efficacy, safety and tolerability of prophylactic liposomal amphotericin B (AmBisome®) for the prevention of invasive fungal infections in subjects receiving remission-induction chemotherapy for acute lymphoblastic leukaemia (AmBiGuard trial). Blood Am Soc Hematol. 2014;124:3646–3646.
Cornely OA, Leguay T, Maertens J, et al. Randomized comparison of liposomal amphotericin B versus placebo to prevent invasive mycoses in acute lymphoblastic leukaemia. J Antimicrob Chemother J Antimicrob Chemother. 2017;72:2359–67.
Zhang T, Bai J, Huang M, et al. Posaconazole and fluconazole prophylaxis during induction therapy for pediatric acute lymphoblastic leukemia. J Microbiol Immunol Infect. 2021;54:1139–46.
Chabrol A, Cuzin L, Huguet F, et al. Prophylaxis of invasive aspergillosis with voriconazole or caspofungin during building work in patients with acute leukemia. Haematologica. 2010;95:996–1003.
Cattaneo C, Monte S, Algarotti A, et al. A randomized comparison of caspofungin versus antifungal prophylaxis according to investigator policy in acute leukaemia patients undergoing induction chemotherapy ({PROFIL}-{C} study). J Antimicrob Chemother. 2011;66:2140–5.
Mandhaniya S, Swaroop C, Thulkar S, et al. Oral voriconazole versus intravenous low dose amphotericin B for primary antifungal prophylaxis in pediatric acute leukemia induction: a prospective, randomized, clinical study. J Pediatr Hematol Oncol. 2011;33(8):e333–41.
Epstein DJ, Seo SK, Huang YT, et al. Micafungin versus posaconazole prophylaxis in acute leukemia or myelodysplastic syndrome: a randomized study. J Infect J Infect. 2018;77:227–34.
Park H, Youk J, Shin DY, et al. Micafungin prophylaxis for acute leukemia patients undergoing induction chemotherapy. BMC Cancer. 2019;19:358.
Teh BW, Yeoh DK, Haeusler GM, et al. Consensus guidelines for antifungal prophylaxis in haematological malignancy and haemopoietic stem cell transplantation. Intern Med J. 2021;51(7):67–88.
Young AY, Leiva Juarez MM, Evans SE. Fungal pneumonia in patients with hematologic malignancy and hematopoietic stem cell transplantation. Clin Chest Med Clin Chest Med. 2017;38:479–91.
Stemler J, Cornely OA. Antifungal prophylaxis in acute myeloid leukemia: new drugs new challenges? Hemasphere. Ovid Technol. 2022;6:e742.
Busca A, Lessi F, Verga L, et al. SEIFEM 2010-{E}: economic evaluation of posaconazole for antifungal prophylaxis in patients with acute myeloid leukemia receiving induction chemotherapy. Leuk Lymphoma. 2017;58:2859–64.
Schonfeld W, Wang Cheng J, Tong KB, et al. Cost-effectiveness analysis of antifungal prophylaxis in patients undergoing hematopoietic stem cell transplantation. Clin Ther. 2008;30:964–73.
Özen M, Yılmaz G, Coşkun B, et al. A quasi-experimental study analyzing the effectiveness of portable high-efficiency particulate absorption filters in preventing infections in hematology patients during construction. Turk J Hematol. 2016;33:41.
Spernovasilis N, Kofteridis DP. Pre-existing liver disease and toxicity of antifungals. J Fungi. 2018;4(4):133.
Michallet M, Sobh M, Morisset S, et al. Validation of positive effect of posaconazole prophylaxis during induction chemotherapy in AML: study of invasive aspergillosis incidence and of risk factors on short and long-term survival. Blood. 2009;114:4124.
Maciej S, Becker FG, Cleary M, et al. Management of acute leukemias. In: Balint G, Antala B, Carty C, Mabieme JMA, Amar IB, Kaplanova A, editors., et al., Uniwersytet śląski. UK: Wolters Kluwer Health Pharma Solutions Europe Ltd; 2018. p. 1743–63.
Fisher MC, Alastruey-Izquierdo A, et al. Tackling the emerging threat of antifungal resistance to human health. Nat Rev Microbiol. 2022;20(9):557–71.
Pagano L, Busca A, Candoni A, et al. Risk stratification for invasive fungal infections in patients with hematological malignancies: SEIFEM recommendations. Blood Rev Blood Rev. 2017;31:17–29.
Ostrosky-Zeichner L, Marr KA, Rex JH, et al. Amphotericin B: time for a new “gold standard.” Clin Infect Dis Clin Infect Dis. 2003;37:415–25.
Cronin S, Chandrasekar PH. Safety of triazole antifungal drugs in patients with cancer. J Antimicrob Chemother J Antimicrob Chemother. 2010;65:410–6.
Vazquez L. Antifungal prophylaxis in immunocompromised patients. Mediterr J Hematol Infect Dis Catholic University in Rome. 2016;8:2016040.
Rabaan AA, Alfaraj AH, Alshengeti A, et al. Antibodies to combat fungal infections: development strategies and progress. Microorganisms 2023, Vol 11, Page 671 [Internet]. Multidisciplinary Digital Publishing Institute; 2023 [cited 2023 Mar 21];11:671. Available from: https://www.mdpi.com/2076-2607/11/3/671/htm
Xin H, Rosario-Colon JA, Eberle K. Novel Intravenous Immunoglobulin Therapy for the Prevention and Treatment of Candida auris and Candida albicans Disseminated Candidiasis. mSphere [Internet]. mSphere; 2023 [cited 2023 Mar 21];8. Available from: https://pubmed.ncbi.nlm.nih.gov/36688668/
Vacca A, Melaccio A, Sportelli A, et al. Subcutaneous immunoglobulins in patients with multiple myeloma and secondary hypogammaglobulinemia: a randomized trial. Clin Immunol [Internet]. Clin Immunol; 2018 [cited 2023 Mar 21];191:110–5. Available from: https://pubmed.ncbi.nlm.nih.gov/29191714/
Kaya Z, Gursel T, Kocak U, et al. Invasive fungal infections in pediatric leukemia patients receiving fluconazole prophylaxis. Pediatr Blood Cancer Pediatr Blood Cancer. 2009;52:470–5.
Pagano L, Caira M, Nosari A, et al. Fungal infections in recipients of hematopoietic stem cell transplants: results of the SEIFEM B-2004 study—sorveglianza epidemiologica infezioni fungine nelle emopatie maligne. Clin Infect Dis. 2007;45:1161–70.
Koeffler HP, Leong G. Preleukemia: one name, many meanings. Leukemia 2017 31:3 [Internet]. Nature Publishing Group; 2016 [cited 2023 Mar 22];31:534–42. Available from: https://www.nature.com/articles/leu2016364
Minetto P, Guolo F, Mikulska M, et al. Posaconazole for primary antifungal Prophylaxis in AML patients: a real life single center experience and a comparison with the Historical cohort. Blood [Internet]. Am J Hematol. 2014;124:5255. Available from: https://ashpublications.org/blood/article/124/21/5255/92439/Posaconazole-for-Primary-Antifungal-Prophylaxis-in.
Michallet M, Sobh M, Morisset S, et al. Antifungal Prophylaxis in AML patients receiving intensive induction chemotherapy: a prospective observational study from the acute leukaemia french association (ALFA) group. Clin Lymphoma Myeloma Leuk [Internet]. Clin Lymphoma Myeloma Leuk. 2022;22:311–8. Available from: https://pubmed.ncbi.nlm.nih.gov/34895843/.
Acknowledgements
To the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and the Graduate Program in Immunology and Applied Parasitology at the Federal University of Uberlândia, Brazil.
Funding
A scholarship was provided by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES Foundation).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Data collection was performed by Luiz RS, YNBC, and MJBS. Data analyses were performed by LRS. The first draft of the manuscript was written by LRS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Soldi, L.R., Coelho, Y.N.B., Paranhos, L.R. et al. The impact of antifungal prophylaxis in patients diagnosed with acute leukemias undergoing induction chemotherapy: a systematic review and meta-analysis. Clin Exp Med 23, 3231–3249 (2023). https://doi.org/10.1007/s10238-023-01062-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01062-9