Abstract
Pay-for-Performance (P4P) to better manage chronic conditions has yielded mixed results. A better understanding of the cost and benefit of P4P is needed to improve program assessment. To this end, we assessed the effect of a P4P program using a quasi-experimental intervention and control design. Two different intervention groups were used, one consisting of newly enrolled P4P patients, and another using P4P patients who have been enrolled since the beginning of the study. Patient-level data on clinical indicators, utilization and expenditures, linked with national death registry, were collected for diabetic patients at a large regional hospital in Taiwan between 2007 and 2013. Net value, defined as the value of life years gained minus the cost of care, is calculated and compared for the intervention group of P4P patients with propensity score-matched non-P4P samples. We found that Taiwan’s implementation of the P4P program for diabetic care yielded positive net values, ranging from $40,084 USD to $348,717 USD, with higher net values in the continuous enrollment model. Our results suggest that the health benefits from P4P enrollment may require a sufficient time frame to manifest, so a net value approach incorporating future predicted mortality risks may be especially important for studying chronic disease management. Future research on the mechanisms by which the Taiwan P4P program helped improve outcomes could help translate our findings to other clinical contexts.


Similar content being viewed by others
Notes
In our data, non-P4P patients with yearly laboratory reports had on average worse laboratory findings than those who did not have yearly reports (not shown).
References
James, J.: Health policy brief: pay-for-performance. Health Aff. 11, 2043–2050 (2012)
Eijkenaar, F., et al.: Effects of pay for performance in health care: a systematic review of systematic reviews. Health Policy 110(2–3), 115–130 (2013)
Figueroa, J.F., et al.: Association between the value-based purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ 353, i2214 (2016)
Grabowski, D.C., et al.: The Impact of nursing home pay-for-performance on quality and medicare spending: results from the nursing home value-based purchasing demonstration. Health Serv Res 52(4), 1387–1408 (2017)
Milstein, R., Schreyoegg, J.: Pay for performance in the inpatient sector: a review of 34 P4P programs in 14 OECD countries. Health Policy 120(10), 1125–1140 (2016)
Mullen, K.J., Frank, R.G., Rosenthal, M.B.: Can you get what you pay for? Pay-for-performance and the quality of healthcare providers. Rand J Econ 41(1), 64–91 (2010)
Ryan, A.M., et al.: Long-term evidence for the effect of pay-for-performance in primary care on mortality in the UK: a population study. Lancet 388(10041), 268–274 (2016)
Van Herck, P., et al.: Systematic review: effects, design choices, and context of pay-for-performance in health care. BMC Health Serv Res 10, 247 (2010)
Petersen, L.A., et al.: Does pay-for-performance improve the quality of health care? Ann Intern Med 145(4), 265–272 (2006)
Mendelson, A., et al.: The effects of pay-for-performance programs on health, health care use, and processes of care: a systematic review. Ann Intern Med 166(5), 341–353 (2017)
Peluso, A., Berta, P., Vinciotti, V.: Do pay-for-performance incentives lead to a better health outcome? Empirical Econ 56(6), 2167–2184 (2019)
Rosenthal, M.B., et al.: Early experience with pay-for-performance: from concept to practice. JAMA 294(14), 1788–1793 (2005)
Pandya, A., et al.: Modelling the cost-effectiveness of pay-for-performance in primary care in the UK. BMC Med 16(1), 135 (2018)
Chen, Y.C., et al.: Impact of pay-for-performance on mortality in diabetes patients in Taiwan: a population-based study. Medicine (Baltimore) 95(27), e4197 (2016)
Lin, T.Y., et al.: The effectiveness of a pay for performance program on diabetes care in Taiwan: a nationwide population-based longitudinal study. Health Policy 120(11), 1313–1321 (2016)
Cutler, D.M., et al.: Are medical prices declining? Evidence from heart attack treatments. Q. J. Econ. 113(4), 991–1024 (1998)
Cheng, S.H., Lee, T.T., Chen, C.C.: A longitudinal examination of a pay-for-performance program for diabetes care: evidence from a natural experiment. Med Care 50(2), 109–116 (2012)
National Health Insurance Administration: Payment schemes for diabetes. Ministry of Health and Welfare (2019)
Eggleston, K., et al.: The net value of health care for patients with type 2 diabetes, 1997 to 2005. Ann Intern Med 151(6), 386–393 (2009)
Eggleston, K., et al.: Are quality-adjusted medical prices declining for chronic disease? Evidence from diabetes care in four health systems. Eur J Health Econ 21(5), 689–702 (2020)
Quan, J., et al.: Risk prediction scores for mortality, cerebrovascular, and heart disease among Chinese people with type 2 diabetes. J Clin Endocrinol Metab 104(12), 5823–5830 (2019)
Department of Statistics: Annual life table. Ministry of the Interior (2018)
Chiu, S.Y.H., Chen, Y.I., Lu, J.R., Kuo, S.F., Chen, C.H.: Developing predictive model on all-cause mortality risk for type 2 diabetes using hospital-based prospective cohort study. J Clin Med 10(20), 4779 (2020)
Cutler, D.M., Rosen, A.B., Vijan, S.: The value of medical spending in the United States, 1960–2000. N Engl J Med 355(9), 920–927 (2006)
Hsieh, H.M., et al.: Cost-effectiveness of a diabetes pay-for-performance program in diabetes patients with multiple chronic conditions. PLoS ONE 10(7), e0133163 (2015)
Allen, T., Mason, T., Whittaker, W.: Impacts of pay for performance on the quality of primary care. Risk Manage. Healthcare Policy 7, 113–120 (2014)
Gupta, N., Ayles, H.M.: Effects of pay-for-performance for primary care physicians on diabetes outcomes in single-payer health systems: a systematic review. Eur. J. Health Econ. 20(9), 1303–1315 (2019)
Kondo, K.K., et al.: Implementation processes and pay for performance in healthcare: a systematic review. J. Gen. Intern. Med. 31(1), 61–69 (2016)
Mathes, T., et al.: Pay for performance for hospitals. Cochrane Database Syst. Rev. (2019). https://doi.org/10.1002/14651858.CD011156.pub2
Van Herck, P., et al.: Systematic review: effects, design choices, and context of pay-for-performance in health care. BMC Health Serv. Res. 10(1), 247 (2010)
Zaresani, A., Scott, A.: Is the evidence on the effectiveness of pay for performance schemes in healthcare changing? Evidence from a meta-regression analysis. BMC Health Serv. Res. 21(1), 175 (2021)
Eijkenaar, F.: Key issues in the design of pay for performance programs. Eur. J. Health Econ. 14(1), 117–131 (2013)
The Commonwealth Fund. International health care system profiles: Taiwan. 2020 [cited 2022 April 18]. https://www.commonwealthfund.org/international-health-policy-center/countries/taiwan.
Chang, R.-E., Lin, S.-P., Aron, D.C.: A pay-for-performance program in Taiwan improved care for some diabetes patients, but doctors may have excluded sicker ones. Health Aff. 31(1), 93–102 (2012)
Hsieh, H.-M., et al.: Effectiveness of pay-for-performance incentive designs on diabetes care. Med. Care 54(12), 1063–1069 (2016)
Huang, J., et al.: Impact of pay-for-performance on management of diabetes: a systematic review. J. Evid. Based Med. 6(3), 173–184 (2013)
Chen, J.Y., et al.: The effect of a PPO pay-for-performance program on patients with diabetes. Am. J. Manag. Care 16(1), e11–e19 (2010)
Chen, Y.-C., et al.: Impact of pay-for-performance on mortality in diabetes patients in Taiwan: a population-based study. Medicine 95(27), e4197–e4197 (2016)
Hsieh, H.-M., et al.: A diabetes pay-for-performance program and the competing causes of death among cancer survivors with type 2 diabetes in Taiwan. Int. J. Qual. Health Care 29(4), 512–520 (2017)
Hsieh, H.-M., et al.: A diabetes pay-for-performance program and risks of cancer incidence and death in patients with type 2 diabetes in Taiwan. Prev. Chronic Dis. 14, E88–E88 (2017)
Hsieh, H.-M., et al.: The association between participation in a pay-for-performance program and macrovascular complications in patients with type 2 diabetes in Taiwan: a nationwide population-based cohort study. Prev. Med. 85, 53–59 (2016)
Li, Y.-H., et al.: The effects of pay-for-performance on tuberculosis treatment in Taiwan. Health Policy Plan. 25(4), 334–341 (2010)
Lee, T.-T., et al.: A pay-for-performance program for diabetes care in Taiwan: a preliminary assessment. Am. J. Manag. Care 16(1), 65–69 (2010)
Sheen, Y.-J., et al.: Impact of the pay-for-performance program on lower extremity amputations in patients with diabetes in Taiwan. Medicine 97(41), e12759–e12759 (2018)
Chen, T.T., et al.: The unintended consequence of diabetes mellitus pay-for-performance (P4P) program in Taiwan: are patients with more comorbidities or more severe conditions likely to be excluded from the P4P program? Health Serv Res. 46(11), 47–60 (2011)
Lee, I.T., et al.: Pay-for-performance for shared care of diabetes in Taiwan. J. Formos. Med. Assoc. 118, S122–S129 (2019)
Hsieh, H.-M., et al.: Cost-effectiveness of diabetes pay-for-performance incentive designs. Med. Care 53(2), 106–115 (2015)
Chang Gung Medical Foundation. Sustainability report, 2020. (2021).
Department of Statistics. Statistics of Medical Care, National Health Insurance, 2020, M.o.H.a. Welfare, Editor. (2021).
Chen, T.-T., Oldenburg, B., Hsueh, Y.-S.: Chronic care model in the diabetes pay-for-performance program in Taiwan: benefits, challenges and future directions. World J. Diabetes 12(5), 578–589 (2021)
Cutler, D.M., et al.: A satellite account for health in the United States. Am. Econ. Rev. 112(2), 494–533 (2022)
Chang, R.E., Lin, S.P., Aron, D.C.: A pay-for-performance program in Taiwan improved care for some diabetes patients, but doctors may have excluded sicker ones. Health Aff (Millwood) 31(1), 93–102 (2012)
Funding
This study was supported by Ministry of SCIENCE and technology, Taiwan (104-2918-I-182-002, 100-2632-H-182-001-MY2), Freeman Spogli Institute for International Studies, Stanford University
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
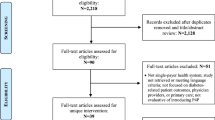
Appendix 1. Analytical sample construction

Appendix 2. Weighted average net value and incremental program effect, Continuous Enrollment Model with 1:1 and 1:3 Nearest Neighbor Matching
Continuous Enrollment Model | ||||
|---|---|---|---|---|
PSM WITHOUT replacement Matched (1:1) sample | PSM WITH replacement Matched (1:3) sample | |||
Non-P4P | P4P | Non-P4P | P4P | |
N | 878 | 878 | 1286 | 1458 |
Survivors | 754 | 840 | 1115 | 1404 |
Decedents | 124 | 38 | 171 | 54 |
Weighted average spending | ||||
Baseline period (a) | $9756 | $7885 | $8322 | $9059 |
Final period (b) | $12,931 | $9477 | $12,200 | $9145 |
Percentage change ([b−a]/a) | 32.54% | 20.20% | 46.60% | 0.95% |
Weighted average net value | ||||
25 K | $10,933 | $43,546 | $11,499 | $46,417 |
50 K | $21,966 | $87,141 | $23,120 | $92,836 |
100 K | $44,032 | $174,333 | $46,362 | $185,675 |
150 K | $66,098 | $261,525 | $69,604 | $278,513 |
200 K | $88,164 | $348,717 | $92,846 | $371,352 |
Incremental program effect† | ||||
25 K | $32,613 | $34,918 | ||
50 K | $65,176 | $69,716 | ||
100 K | $130,301 | $139,313 | ||
150 K | $195,427 | $208,909 | ||
200 K | $260,552 | $278,506 | ||
Appendix 3. Robustness analyses for weighted net values in Continuous Enrollment Model and New Enrollment Model, considering different Cutler cutoffs and values of life
Continuous Enrollment Model | Incremental program effect | New Enrollment Model | Incremental program effect | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Non-P4P | P4P | Non-P4P | P4P | ||||||||
Survivors (N = 754) | Decedents (N = 124) | Survivors (N = 840) | Decedents (N = 38) | Survivors (N = 1,203) | Decedents (N = 138) | Survivors (N = 441) | Decedents (N = 6) | ||||
Cutler coefficient = 1 | |||||||||||
Average net value | |||||||||||
25 K | $51,488 | − $235,728 | $56,292 | − $238,085 | $49,291 | − $265,099 | $44,778 | − $305,501 | |||
95% CI | ($50,000 ~ $52,975) | (− $258,012 ~ − $213,445) | ($54,769 ~ $57,815) | (− $278,094 ~ − $198,076) | ($48,209 ~ $50,374) | (− $287,304 ~ − $242,894) | ($42,772 ~ $46,784) | (− $407,431 ~ − $203,572) | |||
50 K | $103,101 | − $471,512 | $112,637 | − $476,175 | $98,758 | − $529,965 | $89,689 | − $610,810 | |||
95% CI | ($100,124 ~ $106,078) | (− $516,080 ~ − $426,944) | ($109,591 ~ $115,683) | (− $556,217 ~ − $396,133) | ($96,591 ~ $100,925) | (− $574,371 ~ − $485,558) | ($85,676 ~ $93,701) | (− $814,828 ~ − $406,792) | |||
100 K | $206,328 | − $943,079 | $225,327 | − $952,355 | $197,691 | − $1,059,696 | $179,510 | − $1,221,428 | |||
95% CI | ($200,370 ~ $212,286) | (− $1,032,216 ~ -$853,942) | ($219,236 ~ $231,418) | (− $1,112,462 ~ − $792,247) | ($193,355 ~ $202,027) | (− $1,148,505 ~ − $970,886) | ($171,486 ~ $187,533) | (− $1,629,624 ~ − $813,232) | |||
150 K | $309,555 | − $1,414,645 | $338,017 | − $1,428,535 | $296,624 | − $1,589,427 | $269,331 | − $1,832,046 | |||
95% CI | ($300,616 ~ $318,495) | (− $1,548,352 ~ -$1,280,939) | ($328,881 ~ $347,153) | (− $1,668,707 ~ − $1,188,362) | ($290,120 ~ $303,129) | (− $1,722,639 ~ − $1,456,215) | ($257,295 ~ $281,366) | (− $2,444,420 ~ − $1,219,672) | |||
200 K | $412,782 | − $1,886,212 | $450,707 | − $1,904,714 | $395,558 | − $2,119,158 | $359,152 | − $2,442,664 | |||
95% CI | ($400,862 ~ $424,703) | (− $2,064,488 ~ − $1,707,937) | ($438,525 ~ $462,888) | (− $2,224,953 ~ − $1,584,476) | ($386,884 ~ $404,231) | (− $2,296,774 ~ − $1,941,543) | ($343,104 ~ $375,199) | (− $3,259,216 ~ − $1,626,112) | |||
Weighted average net value | |||||||||||
2 5 K | $10,933 | $43,546 | $32,613 | $16,941 | $40,084 | $23,144 | |||||
50 K | $21,966 | $87,141 | $65,176 | $34,062 | $80,302 | $46,239 | |||||
100 K | $44,032 | $174,333 | $130,301 | $68,306 | $160,737 | $92,431 | |||||
150 K | $66,098 | $261,525 | $195,427 | $102,550 | $241,172 | $138,622 | |||||
200 K | $88,164 | $348,717 | $260,552 | $136,793 | $321,607 | $184,814 | |||||
Continuous Enrollment Model | Incremental program effect | New Enrollment Model | Incremental program effect | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Non-P4P | P4P | Non-P4P | P4P | ||||||||
Survivors (N = 754) | Decedents (N = 124) | Survivors (N = 840) | Decedents (N = 38) | Survivors (N = 1203) | Decedents (N = 138) | Survivors (N = 441) | Decedents (N = 6) | ||||
Cutler coefficient = 0.5 | |||||||||||
Average net value | |||||||||||
25 K | $25,681 | − $117,836 | $28,120 | − $119,040 | $24,017 | − $143,771 | $21,319 | − $203,732 | |||
95% CI | ($24,937 ~ $26,425) | (− $128,978 ~ − $106,695) | ($27,358 ~ $28,882) | (− $139,033 ~ − $99,047) | ($24,017 ~ $25,099) | (− $143,771 ~ − $121,562) | ($21,319 ~ $23,326) | (− $203,732 ~ − $101,961) | |||
50 K | $51,488 | − $235,728 | $56,292 | − $238,085 | $48,209 | − $287,304 | $42,772 | − $407,431 | |||
95% CI | ($50,000 ~ $52,975) | (− $258,012 ~ − $213,445) | ($54,769 ~ $57,815) | (− $278,094 ~ − $198,076) | ($48,209 ~ $50,374) | (− $287,304 ~ − $242,894) | ($42,772 ~ $46,784) | (− $407,431 ~ − $203,572) | |||
100 K | $103,101 | − $471,512 | $112,637 | − $476,175 | $96,591 | − $574,371 | $85,676 | − $814,828 | |||
95% CI | ($100,124 ~ $106,078) | (− $516,080 ~ − $426,944) | ($109,591 ~ $115,683) | (− $556,217 ~ − $396,133) | ($96,591 ~ $100,925) | (− $574,371 ~ − $485,558) | ($85,676 ~ $93,701) | (− $814,828 ~ − $406,792) | |||
150 K | $154,715 | − $707,295 | $168,982 | − $714,265 | $144,973 | − $861,438 | $128,581 | − $1,222,226 | |||
95% CI | ($150,247 ~ $159,182) | (− $774,148 ~ − $640,443) | ($164,414 ~ $173,550) | (− $834,339 ~ − $594,190) | ($144,973 ~ $151,476) | (− $861,438 ~ − $728,222) | ($128,581 ~ $140,617) | (− $1,222,226 ~ − $610,012) | |||
200 K | $206,328 | − $943,079 | $225,327 | − $952,355 | $193,355 | − $1,148,505 | $171,486 | − $1,629,624 | |||
95% CI | ($200,370 ~ $212,286) | (− $1,032,216 ~ − $853,942) | ($219,236 ~ $231,418) | (− $1,112,462 ~ − $792,247) | ($193,355 ~ $202,027) | (− $1,148,505 ~ − $970,886) | ($171,486 ~ $187,533) | (− $1,629,624 ~ − $813,232) | |||
Weighted average net value | |||||||||||
25 K | $5416 | $21,748 | $16,331 | $8380 | $19,976 | $11,596 | |||||
50 K | $10,933 | $43,546 | $32,613 | $16,941 | $40,084 | $23,144 | |||||
100 K | $21,966 | $87,141 | $65,176 | $34,062 | $80,302 | $46,239 | |||||
150 K | $32,999 | $130,737 | $97,738 | $51,184 | $120,520 | $69,335 | |||||
200 K | $44,032 | $174,333 | $130,301 | $68,306 | $160,737 | $92,431 | |||||
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lu, Jf.R., Chen, Y.I., Eggleston, K. et al. Assessing Taiwan’s pay-for-performance program for diabetes care: a cost–benefit net value approach. Eur J Health Econ 24, 717–733 (2023). https://doi.org/10.1007/s10198-022-01504-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-022-01504-3