Abstract
Background
The effects of tonsillectomy combined with steroid pulse (TSP) therapy for IgA nephropathy (IgAN) are little known. Therefore, we examined the effects of TSP therapy on the kidney outcomes of IgAN in a large, nationwide cohort study in Japan.
Methods
Between 2002 and 2004, 632 IgAN patients with ≥ 0.5 g/day proteinuria at diagnosis were divided into three groups with mild (0.50–0.99 g/day; n = 264), moderate (1.00–1.99 g/day, n = 216), or severe (≥ 2.00 g/day; n = 153). Decline in kidney function and urinary remission were compared among the three groups after TSP therapy, corticosteroid (ST) therapy, or conservative therapy during a mean follow-up of 6.2 ± 3.3 years. 10.6% and 5.9% of patients in the ST and conservative therapy group underwent tonsillectomy.
Results
The rate of urinary remission at the final observation was significantly higher in the TSP therapy group than in the ST or conservative therapy groups (mild proteinuria: 64%, 43%, and 41%; moderate proteinuria: 51%, 45%, and 28%; severe proteinuria: 48%, 30%, and 22%, respectively). In contrast, the rate of a 50% increase in serum creatinine was lower in groups TSP therapy, than ST or conservative therapy (mild proteinuria: 2.1%, 10.1% and 16.7%; moderate proteinuria: 4.8%, 8.8% and 27.7%; severe proteinuria: 12.0%, 28.9% and 43.1%, respectively). In multivariate analysis, TSP therapy significantly prevented a 50% increase in serum creatinine levels compared with conservative therapy in groups with moderate and severe proteinuria (hazard ratio, 0.12 and 0.22, respectively).
Conclusion
TSP significantly increased the rate of proteinuria disappearance and urinary remission in IgAN patients with mild-to-moderate urinary protein levels. It may also reduce the decline in kidney function in patients with moderate-to-severe urinary protein levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
IgA nephropathy (IgAN) is still the most frequent glomerular disease in the world since its initial report in 1969 [1, 2]. Even in Japan Renal Biopsy Registry (J-RBR) data, IgAN is the most common, accounting for about 30% of diagnosis by kidney biopsy [3, 4]. In Japan, the prognosis of IgAN is poor [5], with approximately 50% of patients developing kidney failure after 30 years [6]. The involvement of galactose-deficient IgA 1 (Gd-IgA1) molecules has been postulated as a cause of this disease, and the development and widespread use of specific treatments for this disease are expected [7].
The Kidney Disease Improving Global Outcomes (KDIGO) guidelines published in 2021 [8] emphasize the importance of blood pressure (BP) control and the administration of the maximum dose of renin–angiotensin system blockade (RAS-B) in the treatment of IgAN. They also stated the importance of discussing the individual risks and benefits of corticosteroid therapy. In addition, tonsillectomy can be considered for a specific population of Japanese patients.
In Japan, the combination of tonsillectomy and steroid pulse (TSP) therapy has been aggressively implemented since 2000 [9,10,11,12,13,14,15,16,17,18,19,20]. The palatine tonsil is assumed to be a site of an abnormal mucosal immune response in IgAN [21,22,23], based on the idea that removal of the palatine tonsil as a lesion is effective. Moreover, tonsillectomy is expected to have a synergistic effect with corticosteroid therapy to suppress the inflammation induced by Gd-IgA1 [24]. However, few studies have enrolled a sufficient number of patients to determine in which disease severity the therapeutic effect is best exerted.
In the present secondary study, we examined whether TSP was more effective than corticosteroid or conservative treatment in a nationwide multicenter retrospective cohort study [25] already conducted in Japan. In this study, we focused on differences in the amount of proteinuria at diagnosis as an indicator of disease severity. The efficacy of treatment was also examined not only in terms of remission in urinary findings but also in terms of worsening kidney function and end-stage kidney disease (ESKD).
Methods
Study design and participant selection
This study was conducted as a secondary study of a Japanese nationwide multicenter retrospective cohort study [25] conducted by the Ministry of Health, Labor and Welfare’s Research Group on Intractable Renal Diseases. The administrative office for this study was established at the St. Marianna Medical University, and the study plan was reviewed and approved by the university’s Ethics Committee (IRB No. 2101). Ethical reviews were conducted and approved by each collaborating institution (e.g., University of Miyazaki, IRB No. 2015-016). This study was conducted in compliance with the principles of the Declaration of Helsinki.
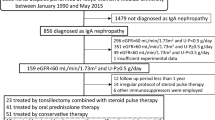
The study population consisted of 1,174 patients aged 18 years or older diagnosed with IgAN by percutaneous kidney biopsy at 42 cooperating institutions nationwide from 2002 to 2004. The last follow-up date for this study was January 31, 2014. Anonymized data with urinary findings or kidney function deficits at diagnosis and the last observation were excluded [25]. The present study focused on proteinuria at diagnosis as an indicator of disease severity. Patients with urinary protein levels less than 0.5 g/day at diagnosis (n = 446) were excluded for a separate study of prognostic factors [26]. Finally, 632 patients were included in this study.
Based on the severity of urinary protein levels, patients were divided into three treatment groups: mild (0.50–0.99 g/day, n = 264), moderate (1.00–1.99 g/day, n = 216), and severe (≥ 2.00 g/day, n = 152). The mean observation period for patients in the current study was 6.2 ± 3.3 years. Figure 1 shows a flowchart of the study design.
Evaluation of clinical findings
Data on age, sex, body mass index (BMI), BP, urinary dip-stick findings and sediment, 24-h proteinuria, urinary protein–creatinine ratio (UP/UCr), estimated GFR (mL/min/1.73 m2) and serological findings of creatinine (sCr), blood urea nitrogen (BUN), uric acid, albumin, total cholesterol, triglyceride, IgA, and C3 at diagnosis and initial treatment were collected from medical records. Information on kidney function (sCr, eGFR) and serological and urinary findings was collected every 3 months during follow-up and final observation. Hypertension was defined as systolic BP > 140 mmHg and/or diastolic BP > 90 mmHg, or use of antihypertensive drugs before diagnosis. The qualitative findings of urinary protein (UP) and urinary occult blood (UOB) were each scored as follows: − and ± as 0; 1+ as 1; 2+ as 2; 3+ as 3. The severity of the histological findings was arbitrarily collected at the discretion of each institution.
Classification of initial treatments
In the nationwide multicenter retrospective cohort study [25], initial treatment (initiated within 1 year after kidney biopsy) was categorized by tonsillectomy and corticosteroid therapy into six categories: tonsillectomy and corticosteroids with pulse therapy (T1S2), tonsillectomy and corticosteroids without pulse therapy (T1S1), tonsillectomy without corticosteroids (T1S0), corticosteroids with pulse therapy (T0S2), corticosteroids without pulse therapy (T0S1), and conservative therapy such as RAS-B without tonsillectomy and corticosteroids (T0S0). In this study, the initial treatment was divided into three groups: TSP therapy (T1S2; n = 114), corticosteroid (ST) therapy (T1S1; n = 26, T0S2; n = 102, and T0S1; n = 118), and conservative therapy (T1S0; n = 16, T0S0; n = 256). In the conservative therapy group, RAS-B was administered in 196 (72.1%) patients and tonsillectomy was performed in 16 (5.9%) patients. The treatment efficacy of the TSP group was compared with that of the other two treatment groups.
Definition of clinical remission and study outcomes
The primary outcome was a decline in kidney function with a 50% increase in sCr from baseline or ESKD with dialysis initiation and preemptive kidney transplantation. The secondary outcome was clinical remission (CR), which was defined as the disappearance of hematuria and proteinuria. The disappearance of hematuria was defined as < 5/HPF of red blood cells in sediment or (–) or (±) in the dip-stick test. The disappearance of proteinuria was also defined as < 0.3 g/day of protein in 24-h urine, a UP/UCr ratio of < 0.3 in spot urine or (–) or (±) in the dip-stick test.
Statistical analysis
All continuous variables are presented as means ± standard deviation (SD). The clinical parameters of the three groups were compared using single-factor analysis of variance (ANOVA) for normally distributed continuous variables or the Kruskal–Wallis test for non-normally distributed continuous variables. Cumulative probabilities of 50% increase in sCr from baseline or ESKD with dialysis initiation were analyzed using the Kaplan–Meier method, and differences in curves were compared using the log-rank test. The effect of multiple covariates on the rate of the primary endpoints was assessed using a Cox proportional hazards model. All independent variables used in multivariate analyses were either categorical (coded as 0/1) or quantitative. Treatments with TSP and ST therapy were considered categorical variables. Age, BMI, systolic BP, eGFR, serum albumin, uric acid, and total cholesterol levels were quantitative variables. The results of the multivariate analysis were expressed as hazard ratios (HR) for 50% increase in sCr from baseline with 95% confidence intervals (CI). A p value of < 0.05 was considered significant for all data, which were statistically analyzed using IBM SPSS Advance Statistical Version 27.0.
Results
Clinical findings at diagnosis and initial treatment
Table 1 shows the basic background information of the patients at diagnosis and initial treatment. The mean UP values in the mild, moderate, and severe groups were 0.71, 1.37, and 3.45 g/day, respectively. As the severity of proteinuria increased, the BP, sCr, and serum uric acid levels increased significantly, whereas the eGFR and serum albumin levels decreased significantly. During the initial treatment, the TSP percentage did not change significantly and ranged from 16.4 to 19.4% among the three groups. However, as the severity of proteinuria increased, the percentage of patients receiving ST therapy increased and the percentage receiving conservative therapy decreased. The percentage of patients who received RAS-B increased significantly from 56.8 to 75.7% as the severity of proteinuria increased.
Remission rates of urinary findings at final observation
Figure 2 shows the percentage of disappearance of UP and UOB and remission of urinary findings (CR) at the last observation in each group according to the treatment modality. The percentage of UP disappearance was significantly higher in all severity groups, in the order of TSP, ST, and conservative therapy (mild proteinuria, 76.6% vs. 54.4% vs. 48.5%; moderate proteinuria, 57.1% vs. 52.7% vs. 34.9%; and severe proteinuria, 48.0% vs. 39.5% vs. 27.5%, respectively). However, the percentage of UOB disappearance did not differ between the treatment modalities. The number of patients with negative UOB before treatment was 4 (3.5%), 3 (1.2%), and 36 (13.2%) in the TSP, ST, and conservative therapy groups, respectively (p < 0.001). The percentage of CR was significantly higher with TSP therapy than with ST or conservative therapy (mild proteinuria, 63.8% vs. 43.0% vs. 41.3%; moderate proteinuria, 50.5% vs. 45.1% vs. 27.7%; and severe proteinuria, 48.0% vs. 30.3% vs. 21.6%, respectively).
Kidney function at final observation
Of all patients, 112 (17.7%) had a 50% increase in sCr from baseline at the last observation. Based on severity, 32 (12.1%), 33 (15.3%), and 47 (30.9%) patients in the mild, moderate, and severe groups, respectively, achieved a 50% increase in sCr. TSP, ST, and conservative therapy led to a 50% increase in sCr in 6 (5.3%), 38 (15.4%), and 68 (25.0%) patients, respectively. The rate of a 50% increase in sCr was lower in groups TSP therapy, than ST or conservative therapy (mild proteinuria: 2.1%, 10.1% and 16.7%; moderate proteinuria: 4.8%, 8.8% and 27.7%; severe proteinuria: 12.0%, 28.9% and 43.1%, respectively). In addition, 49 (7.8%) patients developed ESKD (39 patients with hemodialysis initiation, 9 patients with peritoneal dialysis initiation, one patient with preemptive kidney transplantation) at the last observation. TSP, ST, and conservative therapy led to ESKD in 2 (1.8%), 20 (8.1%), and 27 (9.9%) patients, respectively, and this outcome was significantly less common with TSP than the other treatments (p < 0.001, Chi-square test). Figures 3 and 4 show the Kaplan–Meier curves for a 50% increase in sCr and ESKD with dialysis initiation, respectively, in the urinary protein severity groups. In all patients, the 50% increase in sCr and ESKD differed significantly between the TSP, ST, and conservative therapy groups (p < 0.001 and p = 0.041 by log-rank test). In particular, in all groups, TSP significantly suppressed the 50% increase in sCr, especially when compared with conservative therapy. On the other hand, comparison of the TSP and ST groups showed no significant difference in the 50% increase in sCr and ESKD occurrence in the stratified urine protein group. The 10-year kidney survival rates were 97.0%, 87.0%, and 78.7% for TSP, ST, and conservative therapy, respectively.
Analysis of factors contributing to renal outcome
The Cox proportional hazards model was used to evaluate the effects of clinical findings and the modality of initial treatment on the 50% increase in sCr from baseline. The major risk factors for IgAN progression, including TSP, ST, and conservative therapy, were selected as imperative independent variables in the model (Table 2). Age in the mild group; sex, BMI, eGFR, serum albumin level, and serum total cholesterol level in the moderate group; and eGFR level in the severe group were poor prognostic factors. TSP significantly reduced the decline in kidney function compared with conservative therapy in the moderate and severe groups (HR, 0.119; 95% CI 0.025–0.569 and HR, 0.221; 95% CI 0.058–0.839, respectively). In contrast, in the mild group, it had no significant effect on kidney function.
Adverse events of each treatment
65 adverse events were observed in 47 patients in this study: 5 events in the TSP therapy group, 42 in the ST therapy group, and 18 in the conservative therapy group. Infections occurred in eight cases, including four cases of pneumonia, in five patients in the ST-treated group, but none in the TSP group. Diabetes occurred in 8 patients in the ST therapy group. In the TSP therapy group, one patient of gastric ulcer, one patient of pancreatitis, and three patients of complications related to tonsillectomy occurred, but no serious adverse events were observed.
Discussion
The primary nationwide multicenter cohort study [25] analyzed 1,065 of 1,174 registered patients with IgAN. The group that underwent tonsillectomy (n = 252) was compared with the group that did not undergo tonsillectomy (n = 813). The primary outcome (50% increase in sCr from baseline or ESKD) was significantly reduced in the tonsillectomy group (HR, 0.43; 95% CI, 0.20–0.85), which was similar after 1:1 propensity score matching and inverse probability of treatment weighted estimation (IPTW) matching. The rate of additional treatment within 1 year of diagnosis was also significantly lower (HR, 0.37; 95% CI, 0.20–0.63). This study included 632 patients with urinary protein levels of 0.5 g/day or higher, and treatment efficacy was compared between TSP therapy (T1S2), ST therapy (T1S1 and T0S2 and T0S1), and conservative therapy (T1S0 and T0S0). The CR rate was significantly higher in the TSP group than in the conservative therapy group, regardless of the urinary protein level at diagnosis. The incidence of the primary outcome (a 50% increase in sCr from baseline or ESKD with dialysis initiation) was also significantly reduced.
Studies comparing TSP with other treatments using the percentage of CR in IgAN as an outcome have been conducted mainly in Japan [9,10,11,12,13,14,15,16,17,18,19,20]. These results show an association between the proteinuria severity before treatment and the CR rate after treatment. Concretely, at pretreatment proteinuria levels of 0.5–1.0 g/day, 1.0–1.5 g/day, and 1.5–2.0 g/day, proteinuria disappeared at estimated rates of 70%, 60%, and 50%, respectively. However, most of these were small, single-center cohort studies. The present study was based on a large multicenter cohort, and the percentages of disappearance of proteinuria with TSP in the mild (0.50–0.99 g/day), moderate (1.00–1.99 g/day), and severe groups (≥ 2.00 g/day) were 76.6%, 57.1%, and 48.0%, respectively. These results are consistent with those of previous studies.
There have been only a few reports on the effect of TSP on IgAN in reducing kidney function decline [20, 27,28,29]. These studies reported that TSP significantly reduced kidney function decline compared with other treatments; however, outcome measures varied, including ESKD, doubling of sCr, and a 25% decrease in eGFR. Hoshino et al. [29], in a study of 1,127 patients with IgAN at four hospitals, found that when UP levels were 1.0 g/day or higher, TSP was significantly more effective than RAS-B treatment in suppressing the ESKD progression. In contrast, in patients with UP levels less than 1.0 g/day, there was no difference in the efficacy between TSP, corticosteroid therapy, and RAS-B. This is consistent with the results of the current study, in which the primary outcome was a 50% increase in sCr levels from baseline or dialysis initiation. The effect of TSP on kidney function decline in the mild group could not be statistically demonstrated in multivariate analysis. A nationwide secondary cohort study of patients with urinary protein < 0.5 g/day at diagnosis [26] also found no effect of tonsillectomy or corticosteroid therapy on reducing kidney function decline. This may be partly due to the small number of primary endpoints that occurred in patients with mild IgAN during the limited observation period.
A large prospective cohort study was also conducted in Japan (Japan IgA Nephropathy Prospective Cohort Study: J-IGACS) [30], in which 1,130 patients with IgAN were enrolled between 2005 and 2015. Finally, 941 patients were included in the analysis, and the efficacy of treatment was compared among three groups: corticosteroid plus tonsillectomy, corticosteroid therapy, and non-corticosteroid therapy. Corticosteroid therapy and corticosteroid plus tonsillectomy significantly reduced primary outcomes (50% increase in sCr from baseline or dialysis initiation) compared with non-corticosteroid therapy. Furthermore, corticosteroid plus tonsillectomy reduced the rate of the primary outcomes significantly more than corticosteroid therapy (HR 0.40, 95% CI 0.18–0.91).
These results suggest that TSP may lead to better CR in mild IgAN. In contrast, if performed in patients with moderate-to-severe IgAN, it is expected to preserve kidney function over the medium to long term.
Abnormalities in the mucosal–bone axis may be involved in the pathogenesis of IgAN [31]. This indicates an increased production of Gd-IgA1 in IgAN in the early stages according to the multi-hit theory [32], which is a tentative theory of the pathogenesis of IgAN. Whether the gut-associated lymphoid tissue (GALT) or nasal-associated lymphoid tissue (NALT) is the primary site of mucosal immune abnormalities is debatable. The efficacy of intestinal-selective corticosteroids in the NEFIGAN trial [33] indicates that GALT may be important in the pathogenesis of IgAN. Meanwhile, the production of Gd-IgA1 from tonsil cells in patients with IgAN [21] and the decrease in serum Gd-IgA1 levels after tonsillectomy [22] suggested that NALT may contribute to the production of Gd-IgA1. Tonsillectomy may prevent the progression and relapse of IgAN by eliminating abnormal sites of mucosal immunity. Liu et al. also reported the benefit of tonsillectomy for CR and suppression of ESKD progression in a meta-analysis of 14 studies [34]. In addition, in the primary nationwide multicenter cohort study, tonsillectomy was relatively safe, with complications occurring in only seven of 252 patients (2.8%) [25]. Recently, a series of therapies specific to the pathogenesis of IgAN have been developed, such as anti-B cell and anti-plasmacytoid therapies targeting Gd-IgA1 and regulators of complement activity [7]. In the future, these drugs will become the mainstay of treatment; however, until then, tonsillectomy will be an effective treatment for eliminating Gd-IgA1.
The current study has several limitations. First, although this was a large multicenter cohort study, it focused on initial treatment and did not adequately examine treatment during the course of the study. Second, the initial treatment in this study took place between 2002 and 2004, and the treatment methods, such as the percentage of RAS-B administered, may have changed. In fact, in a questionnaire survey conducted in 2021 among members of the Japanese Society of Nephrology, 88.6% of patients with IgAN with urinary protein of 1.0 g/day or more responded that they would receive RAS-B [35]. Third, this study did not consider the detailed methods of steroid pulse therapy. There are two major methods of steroid pulse therapy: the Pozzi method and the Hotta method [9, 36]. In this study, the treatment advantage of the TSP group over the ST group was very limited when analyzed stratified by urinary protein level. It is possible that this was due to differences in the modalities of steroid pulse therapy. In contrast, a secondary national multicenter cohort study reported that the number of steroid pulse courses did not affect kidney prognosis [37]. Future detailed studies are needed to consider more definite indications for TSP therapy. Fourth, in the present study, we performed a multivariate analysis of prognostic factors, stratified by severity based on the amount of proteinuria. Therefore, statistical analyses such as propensity score matching and IPTW matching were not performed, which may not have adequately controlled for confounding factors and selection bias of the initial treatment. Fifth, histopathological factors were not included in the prognostic analysis in the present study because information on histological severity was not made a mandatory registration at the study design stage. Finally, all participants in the present study were adult Japanese, and it is unclear whether similar results can be obtained in other racial groups.
In conclusion, TSP significantly increased the rate of proteinuria disappearance and CR in patients with IgAN, regardless of the amount of proteinuria at diagnosis. It may also reduce the decline in kidney function in patients with moderate-to-severe urinary protein levels.
References
D’Amico G. The commonest glomerulonephritis in the world: IgA nephropathy. Q J Med. 1987;64:709–27.
Julian BA, Waldo FB, Rifai A, Mestecky J. IgA nephropathy, the most common glomerulonephritis worldwide. A neglected disease in the United States? Am J Med. 1988;84:129–32.
Sugiyama H, Yokoyama H, Sato H, Saito T, Kohda Y, Nishi S, Tsuruya K, Kiyomoto H, Iida H, Sasaki T, Higuchi M, Hattori M, Oka K, Kagami S, Nagata M, Kawamura T, Honda M, Fukasawa Y, Fukatsu A, Morozumi K, Yoshikawa N, Yuzawa Y, Matsuo S, Kiyohara Y, Joh K, Taguchi T, Makino H, Committee for Standardization of Renal Pathological Diagnosis, Working Group for Renal Biopsy Database, Japanese Society of Nephrology. Japan Renal Biopsy Registry: the first nationwide, web-based, and prospective registry system of renal biopsies in Japan. Clin Exp Nephrol. 2011;15:493–503.
Komatsu H, Fujimoto S, Yoshikawa N, Kitamura H, Sugiyama H, Yokoyama H. Clinical manifestations of Henoch-Schӧnlein purpura nephritis and IgA nephropathy: comparative analysis of data from the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol. 2016;20:552–60.
Pitcher D, Braddon F, Hendry B, Mercer A, Osmaston K, Saleem MA, Steenkamp R, Wong K, Turner AN, Wang K, Gale DP, Barratt J. Long-term outcomes in IgA nephropathy. Clin J Am Soc Nephrol. 2023;18:727–38.
Moriyama T, Tanaka K, Iwasaki C, Oshima Y, Ochi A, Kataoka H, Itabashi M, Takei T, Uchida K, Nitta K. Prognosis in IgA nephropathy: 30-year analysis of 1,012 patients at a single center in Japan. PLoS ONE. 2014;9: e91756.
El Karoui K, Fervenza FC, De Vriese AS. Treatment of IgA nephropathy: a rapidly evolving field. J Am Soc Nephrol. 2024;35:103–16.
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO. Clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;2021(100):S1–276.
Hotta O, Miyazaki M, Furuta T, Tomioka S, Chiba S, Horigome I, Abe K, Taguma Y. Tonsillectomy and steroid pulse therapy significantly impact on clinical remission in patients with IgA nephropathy. Am J Kidney Dis. 2001;38:736–43.
Miyazaki M, Hotta O, Komatsuda A, Nakai S, Shoji T, Yasunaga C, Taguma Y, Japanese Multicenter Study Group on Treatment of IgA Nephropathy (JST-IgAN). A multicenter prospective cohort study of tonsillectomy and steroid therapy in Japanese patients with IgA nephropathy: a 5-year report. Contrib Nephrol. 2007; 157:94–8.
Komatsu H, Fujimoto S, Hara S, Sato Y, Yamada K, Kitamura K. Effect of tonsillectomy plus steroid pulse therapy on clinical remission of IgA nephropathy: a controlled study. Clin J Am Soc Nephrol. 2008;3:1301–7.
Kawaguchi T, Ieiri N, Yamazaki S, Hayashino Y, Gillespie B, Miyazaki M, Taguma Y, Fukuhara S, Hotta O. Clinical effectiveness of steroid pulse therapy combined with tonsillectomy in patients with immunoglobulin A nephropathy presenting glomerular haematuria and minimal proteinuria. Nephrology (Carlton). 2010;15:116–23.
Nakagawa N, Kabara M, Matsuki M, Chinda J, Fujino T, Hirayama T, Takahara M, Harabuchi Y, Kikuchi K, Hasebe N. Retrospective comparison of the efficacy of tonsillectomy with and without steroid-pulse therapy in IgA nephropathy patients. Intern Med. 2012;51:1323–8.
Ochi A, Moriyama T, Takei T, Uchida K, Nitta K. Comparison between steroid pulse therapy alone and in combination with tonsillectomy for IgA nephropathy. Int Urol Nephrol. 2013;45:469–76.
Kawamura T, Yoshimura M, Miyazaki Y, Okamoto H, Kimura K, Hirano K, Matsushima M, Utsunomiya Y, Ogura M, Yokoo T, Okonogi H, Ishii T, Hamaguchi A, Ueda H, Furusu A, Horikoshi S, Suzuki Y, Shibata T, Yasuda T, Shirai S, Imasawa T, Kanozawa K, Wada A, Yamaji I, Miura N, Imai H, Kasai K, Soma J, Fujimoto S, Matsuo S, Tomino Y, Special IgA Nephropathy Study Group. A multicenter randomized controlled trial of tonsillectomy combined with steroid pulse therapy in patients with immunoglobulin A nephropathy. Nephrol Dial Transplant. 2014; 29:1546–53.
Miyamoto T, Nishino T, Nakata T, Sato Y, Komatsu H, Uramatsu T, Ishimatsu N, Ishida K, Serino R, Otsuji Y, Miyazaki M, Tomo T, Tamura M, Fujimoto S. Impact of tonsillectomy combined with steroid pulse therapy on immunoglobulin A nephropathy depending on histological classification: a multicenter study. Clin Exp Nephrol. 2016;20:50–7.
Komatsu H, Sato Y, Miyamoto T, Tamura M, Nakata T, Tomo T, Nishino T, Miyazaki M, Fujimoto S. Significance of tonsillectomy combined with steroid pulse therapy for IgA nephropathy with mild proteinuria. Clin Exp Nephrol. 2016;20:94–102.
Hoshino Y, Moriyama T, Uchida K, Tsuchiya K, Nitta K. Comparison of oral steroids with tonsillectomy plus steroid pulse therapy in patients with IgA nephropathy. Clin Exp Nephrol. 2017;21:617–23.
Ogura S, Moriyama T, Miyabe Y, Karasawa K, Nitta K. Evaluation of appropriate treatment for IgA nephropathy with mild proteinuria and normal renal function. Clin Exp Nephrol. 2021;25:1103–10.
Kumon S, Moriyama T, Kamiyama T, Karasawa K, Nitta K. The impact of tonsillectomy combined with steroid pulse therapy in patients with advanced IgA nephropathy and impaired renal function. Clin Exp Nephrol. 2020;24:295–306.
Inoue T, Sugiyama H, Hiki Y, Takiue K, Morinaga H, Kitagawa M, Maeshima Y, Fukushima K, Nishizaki K, Akagi H, Narimatsu Y, Narimatsu H, Makino H. Differential expression of glycogenes in tonsillar B lymphocytes in association with proteinuria and renal dysfunction in IgA nephropathy. Clin Immunol. 2010;136:447–55.
Nakata J, Suzuki Y, Suzuki H, Sato D, Kano T, Yanagawa H, Matsuzaki K, Horikoshi S, Novak J, Tomino Y. Changes in nephritogenic serum galactose-deficient IgA1 in IgA nephropathy following tonsillectomy and steroid therapy. PLoS ONE. 2014;9: e89707.
Suzuki Y, Matsuzaki K, Suzuki H, Okazaki K, Yanagawa H, Ieiri N, Sato M, Sato T, Taguma Y, Matsuoka J, Horikoshi S, Novak J, Hotta O, Tomino Y. Serum levels of galactose-deficient immunoglobulin (Ig) A1 and related immune complex are associated with disease activity of IgA nephropathy. Clin Exp Nephrol. 2014;18:770–7.
Hotta O. Use of corticosteroids, other immunosuppressive therapies, and tonsillectomy in the treatment of IgA nephropathy. Semin Nephrol. 2004;24:244–55.
Hirano K, Matsuzaki K, Yasuda T, Nishikawa M, Yasuda Y, Koike K, Maruyama S, Yokoo T, Matsuo S, Kawamura T, Suzuki Y. Association between tonsillectomy and outcomes in patients with immunoglobulin A nephropathy. JAMA Netw Open. 2019;2: e194772.
Shirai S, Yasuda T, Kumagai H, Matsunobu H, Ichikawa D, Shibagaki Y, Yasuda Y, Matsuzaki K, Hirano K, Kawamura T, Suzuki Y, Maruyama S. Prognostic factors of IgA nephropathy presenting with mild proteinuria at the time of diagnosis (a multicenter cohort study). Clin Exp Nephrol. 2023;27:340–8.
Sato M, Hotta O, Tomioka S, Horigome I, Chiba S, Miyazaki M, Noshiro H, Taguma Y. Cohort study of advanced IgA nephropathy: efficacy and limitations of corticosteroids with tonsillectomy. Nephron Clin Pract. 2003;93:c137–45.
Yamamoto Y, Hiki Y, Nakai S, Yamamoto K, Takahashi K, Koide S, Murakami K, Tomita M, Hasegawa M, Kawashima S, Sugiyama S, Yuzawa Y. Comparison of effective impact among tonsillectomy alone, tonsillectomy combined with oral corticosteroid and with steroid pulse therapy on long-term outcome of immunoglobulin A nephropathy. Clin Exp Nephrol. 2013;17:218–24.
Hoshino J, Fujii T, Usui J, Fujii T, Ohashi K, Takaichi K, Suzuki S, Ubara Y, Yamagata K. Renal outcome after tonsillectomy plus corticosteroid pulse therapy in patients with immunoglobulin A nephropathy: results of a multicenter cohort study. Clin Exp Nephrol. 2016;20:618–27.
Kawamura T, Hirano K, Koike K, Nishikawa M, Shimizu A, Joh K, Katafuchi R, Hashiguchi A, Matsuzaki K, Maruyama S, Tsuboi N, Narita I, Yano Y, Yokoo T, Suzuki Y. Associations of corticosteroid therapy and tonsillectomy with kidney survival in a multicenter prospective study for IgA nephropathy. Sci Rep. 2023;13:18455.
Suzuki Y, Tomino Y. Potential immunopathogenic role of the mucosa-bone marrow axis in IgA nephropathy: insights from animal models. Semin Nephrol. 2008;28:66–77.
Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA. The pathophysiology of IgA nephropathy. J Am Soc Nephrol. 2011;22:1795–803.
Wimbury D, Muto M, Bhachu JS, Scionti K, Brown J, Molyneux K, Seikrit C, Maixnerová D, Pérez-Alós L, Garred P, Floege J, Tesař V, Fellstrom B, Coppo R, Barratt J. Targeted-release budesonide modifies key pathogenic biomarkers in immunoglobulin A nephropathy: insights from the NEFIGAN trial. Kidney Int. 2024; 105:381–8. S0085–2538(23)00778–0.
Liu LL, Wang LN, Jiang Y, Yao L, Dong LP, Li ZL, Li XL. Tonsillectomy for IgA nephropathy: a meta-analysis. Am J Kidney Dis. 2015;65:80–7.
Matsuzaki K, Suzuki H, Kikuchi M, Koike K, Komatsu H, Takahashi K, Narita I, Okada H, Committee of Clinical Practical Guideline for IgA Nephropathy 2020. Current treatment status of IgA nephropathy in Japan: a questionnaire survey. Clin Exp Nephrol. 2023;27:1032–41.
Pozzi C, Bolasco PG, Fogazzi GB, Andrulli S, Altieri P, Ponticelli C, Locatelli F. Corticosteroids in IgA nephropathy: a randomised controlled trial. Lancet. 1999;353:883–7.
Moriyama T, Kataoka H, Nitta K, Hirano K, Matsuzaki K, Yasuda T, Yasuda Y, Koike K, Maruyama S, Yokoo T, Matsuo S, Kawamura T, Suzuki Y. Impact of the number of steroid pulses in tonsillectomy combined with steroid pulse therapy: a nationwide retrospective study in Japan. Clin Exp Nephrol. 2021;25:19–27.
Acknowledgements
This study was presented in part at Kidney Week 2015, the annual meeting of the American Society of Nephrology, November 4–6, 2015, in San Diego, California, USA. The primary study [25] of this sub-analysis was supported in part by a Grant-in Aid for Progressive Renal Disease Research, Research on Intractable Disease, from Ministry of Health, Labour and Welfare of Japan. We thank Editage (http://www.editage.jp) for editing this manuscript.
Funding
Open access funding provided by University of Miyazaki.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have declared no competing interest.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Komatsu, H., Fujimoto, S., Sato, Y. et al. Effect of tonsillectomy combined with steroid pulse therapy upon IgA nephropathy depending on proteinuria status at diagnosis: a nationwide multicenter cohort study in Japan. Clin Exp Nephrol (2024). https://doi.org/10.1007/s10157-024-02530-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10157-024-02530-6