Abstract
Background
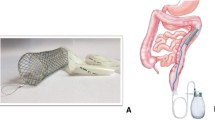
Currently, the only clinically valid method to prevent morbidity and mortality related to colorectal anastomotic leaks is by construction of a protective ileostomy. Intraluminal bypass might also be a possible way to proctect the anastomosis. The aim of the present study was to evaluate the CG-100 intraluminal bypass device for the reduction of anastomosis-related morbidity and stoma creation in cases of rectal resection.
Methods
A prospective study was conducted on patients having sphincter-preserving rectal resection who were treated with the CG-100 device at Soroka University Medical Center, Beer Sheva, Israel between May 2015 and February 2017. The device was implanted during surgery and removed after 10 ± 1 days. All patients underwent a radiologic leak test with water-soluble contrast prior to removal of the device. Patients were followed for 30 days. Information about adverse events, anastomotic leaks, device usability and tolerance were collected.
Results
Forty-seven patients participated in the study. Most patients were operated on due to cancer 44 (93.6%). Four (9%) patients received a primary protective stoma on top of the CG-100 device as part of the learning curve of the surgical team and none required a stoma after device removal. Five (9%) serious adverse events were reported, but only 2 (4%) were classified as related to the device. One was a transient enterocutaneous fistula after removal of the device. The second was an asymptomatic radiologic leak in 1 (2.1%) patient which was treated by keeping the device in place and antibiotic treatment for another 10 days without creation of diverting ileostomy.
Conclusions
CG-100 may provide a safe method for fecal diversion over a newly created anastomosis without the complications related to stoma creation and closure. A larger prospective randomized study in patients originally scheduled to receive diverting stoma is needed to confirm these findings.



Similar content being viewed by others
References
Tilney HS et al (2008) A national perspective on the decline of abdominoperineal resection for rectal cancer. Ann Surg 247:77–84
Alves A, Panis Y, Pocard M, Regimbeau JM, Valleur P (1999) Management of anastomotic leakage after nondiverted large bowel resection. J Am Coll Surg 189:554–559
Platell C, Barwood N, Dorfmann G, Makin G (2007) The incidence of anastomotic leaks in patients undergoing colorectal surgery. Colorectal Dis 9:71–79
Placer C et al (2014) Preventing complications in colorectal anastomosis: results of a randomized controlled trial using bioabsorbable staple line reinforcement for circular stapler. Dis Colon Rectum 57:1195–1201
Jafari MD et al (2015) Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): a multi-institutional study. J Am Coll Surg 220:82.e1–92.e1
Masoomi H et al (2013) Compression anastomosis ring device in colorectal anastomosis: a review of 1, 180 patients. Am J Surg 205:447–451
Shogan BD et al (2015) Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci Transl Med 7(286):286ra68. https://doi.org/10.1126/scitranslmed.3010658
Van Praagh JB et al (2016) Intestinal microbiota and anastomotic leakage of stapled colorectal anastomoses: a pilot study. Surg Endosc 30:2259–2265
Boni L et al (2015) Indocyanine green-enhanced fluorescence to assess bowel perfusion during laparoscopic colorectal resection. Surg Endosc. https://doi.org/10.1007/s00464-015-4540-z
Huh JW, Kim HR, Kim YJ (2010) Anastomotic leakage after laparoscopic resection of rectal cancer: the impact of fibrin glue. Am J Surg 199:435–441
Beck DE et al (2003) A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum 46:1310–1319
Matthiessen P, Hallböök O, Rutegård J, Simert G, Sjödahl R (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 246:207–214
Emmanuel A et al (2018) Defunctioning stomas result in significantly more short-term complications following low anterior resection for rectal cancer. World J. Surg. https://doi.org/10.1007/s00268-018-4672-0
Willenz U, Wasserberg N, Botero-Anug AM, Greenberg R (2016) Feasibility of an intraluminal bypass device in low colorectal anastomosis. Surg Innov 23:298–304
Pisarska M et al (2018) Defunctioning ileostomy reduces leakage rate in rectal cancer surgery—systematic review and meta-analysis. Oncotarget 9:20816–20825
Gessler B, Haglind E, Angenete E (2014) A temporary loop ileostomy affects renal function. Int J Colorectal Dis 29:1131–1135
Ihnát P et al (2016) Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc Other Interv Tech 30:4809–4816
Hallböök O, Matthiessen P, Leinsköld T, Nyström P-O, Sjödahl R (2002) Safety of the temporary loop ileostomy. Colorectal Dis 4:361–364
Danielsen AK et al (2017) Early closure of a temporary ileostomy in patients with rectal cancer. Ann Surg 265:284–290
Menahem B, Lubrano J, Vallois A, Alves A (2018) Early closure of defunctioning loop ileostomy: is it beneficial for the patient? A meta-analysis. World J Surg 42:3171–3178
Manzenreiter L et al (2018) A proposal for a tailored approach to diverting ostomy for colorectal anastomosis. Minerva Chir 73:29–35
Miedema BW, Astudillo JA, Sporn E, Thaler K (2008) NOTES techniques: present and future. Eur Surg Acta Chir Austriaca 40:103–110
Ravo B et al (1987) The treatment of perforated diverticulitis by one-stage intracolonic bypass procedure. Surgery 102:771–776
Rosati C et al (1992) Primary colorectal anastomosis with the intracolonic bypass tube. Surgery 112:618–622 (discussion 622–623)
Yoon WH, Song I, Chang ES (1994) Intraluminal bypass technique using a condom for protection of coloanal anastomosis. Dis Colon Rectum 37:1046–1047
Ye F, Chen D, Wang D, Lin J, Zheng S (2014) Use of valtrac TM-secured intracolonic bypass in laparoscopic rectal cancer resection. Medicine 93:1–7
Bakker IS et al (2017) Randomized clinical trial of biodegradable intraluminal sheath to prevent anastomotic leak after stapled colorectal anastomosis. Br J Surg 104:1010–1019
Author information
Authors and Affiliations
Contributions
All authors were involved in study design, patient recruitment, data collection and writing or reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest and funding
Study was sponsored by Colospan Ltd.; none of the authors have any direct involvement with the company. Data collection was done by the company, but the analysis was done independent of any company involvement.
Ethical approval
All procedures performed in the study involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reshef, A., Ben-Arie, G. & Pinsk, I. Protection of colorectal anastomosis with an intraluminal bypass device for patients undergoing an elective anterior resection: a pilot study. Tech Coloproctol 23, 565–571 (2019). https://doi.org/10.1007/s10151-019-02015-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-019-02015-9