Abstract
Background
With the rapid aging of populations worldwide, the number of vulnerable patients with liver metastasis from colorectal cancer has increased. This study aimed to examine the association between vulnerability and clinical outcomes in patients with colorectal liver metastasis (CRLM).
Methods
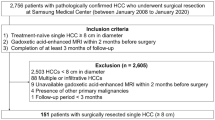
Consecutive 101 patients undergoing upfront hepatectomy for CRLM between 2004 and 2020 were included. The preoperative vulnerability was assessed using the Clinical Frailty Scale (CFS) score ranging from one (very fit) to nine (terminally ill), and frailty was defined as a CFS score of ≥ 4. A multivariable Cox proportional hazard regression model was utilized to investigate associations of frailty with disease-free survival (DFS), overall survival (OS), and cancer-specific survival (CSS).
Results
Of the 101 patients, 12 (12%) had frailty. Associations between frailty and surgical outcomes, namely, the incidence of 90-day mortality and postoperative complications, were not statistically significant (P > 0.05). In the multivariable analyses, after adjusting for clinical risk scores calculated using six factors (timing of liver metastasis, primary tumor lymph node status, number of liver tumors, size of the largest tumor, extrahepatic metastatic disease, and carbohydrate antigen 19–9 level) to predict recurrence following hepatectomy for CRLM, preoperative frailty was found to be an independent risk factor for DFS (hazard ratio [HR]:2.37, 95% confidence interval [CI] 1.06–4.72, P = 0.036), OS (HR:4.17, 95% CI 1.43–10.89, P = 0.011), and CSS (HR:3.49, 95% CI 1.09–9.60, P = 0.036).
Conclusion
Preoperative frailty was associated with worse DFS, OS, and CSS after upfront hepatectomy for CRLM. Assessment and improvement of patient vulnerability may provide a favorable prognosis for patients with CRLM.

Similar content being viewed by others
References
Xi Y, Xu P (2021) Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol 14(10):101174. https://doi.org/10.1016/j.tranon.2021.101174
Tsilimigras DI, Brodt P, Clavien PA et al (2021) Liver metastases Nat Rev Dis Primers 7(1):27. https://doi.org/10.1038/s41572-021-00261-6
Horino T, Tokunaga R, Miyamoto Y et al (2023) The impact of the advanced lung cancer inflammation index on the outcomes of patients with metastatic colorectal cancer who receive chemotherapy. Int J Clin Oncol 28(3):400–408. https://doi.org/10.1007/s10147-023-02293-2
Ignatavicius P, Oberkofler CE, Chapman WC et al (2020) Choices of Therapeutic Strategies for Colorectal Liver Metastases Among Expert Liver Surgeons: A Throw of the Dice? Ann Surg 272(5):715–722. https://doi.org/10.1097/SLA.0000000000004331
Ellis J, Petersen M, Chang S et al (2023) Health care professionals’ experiences of dealing with cancer cachexia. Int J Clin Oncol 28(4):592–602. https://doi.org/10.1007/s10147-023-02300-6
Kato R, Miyamoto Y, Ouchi M et al (2023) The Geriatric Nutritional Risk Index is a prognostic marker in patients with metastatic colorectal cancer. Int J Clin Oncol. https://doi.org/10.1007/s10147-023-02338-6
Corbaux P, Terret C, Cropet C et al (2023) Association of chemotherapy and comorbidities with overall survival in elderly patients with early breast cancer: a French population-based propensity score-matched analysis. Int J Clin Oncol 28(3):371–381. https://doi.org/10.1007/s10147-023-02296-z
Sedrak MS, Freedman RA, Cohen HJ et al (2021) Older adult participation in cancer clinical trials: A systematic review of barriers and interventions. CA Cancer J Clin 71(1):78–92. https://doi.org/10.3322/caac.21638
Mima K, Nakagawa S, Miyata T et al (2023) Frailty and surgical outcomes in gastrointestinal cancer: Integration of geriatric assessment and prehabilitation into surgical practice for vulnerable patients. Ann Gastroenterol Surg 7(1):27–41. https://doi.org/10.1002/ags3.12601
Nakajima H, Yamaguchi J, Takami H et al (2023) Impact of skeletal muscle mass on the prognosis of patients undergoing neoadjuvant chemotherapy for resectable or borderline resectable pancreatic cancer. Int J Clin Oncol 28(5):688–697. https://doi.org/10.1007/s10147-023-02321-1
Rockwood K, Song X, MacKnight C et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173(5):489–495. https://doi.org/10.1503/cmaj.050051
Mima K, Miyanari N, Morito A et al (2020) Frailty is an independent risk factor for recurrence and mortality following curative resection of stage I-III colorectal cancer. Ann Gastroenterol Surg 4(4):405–412. https://doi.org/10.1002/ags3.12337
Mima K, Hayashi H, Nakagawa S et al (2021) Frailty is associated with poor prognosis after resection for pancreatic cancer. Int J Clin Oncol 26(10):1938–1946. https://doi.org/10.1007/s10147-021-01983-z
Rostoft S, O’Donovan A, Soubeyran P et al (2021) Geriatric Assessment and Management in Cancer. J Clin Oncol 39(19):2058–2067. https://doi.org/10.1200/JCO.21.00089
Church S, Rogers E, Rockwood K et al (2020) A scoping review of the Clinical Frailty Scale. BMC Geriatr 20(1):393. https://doi.org/10.1186/s12877-020-01801-7
Beppu T, Sakamoto Y, Hasegawa K et al (2012) A nomogram predicting disease-free survival in patients with colorectal liver metastases treated with hepatic resection: multicenter data collection as a Project Study for Hepatic Surgery of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci 19(1):72–84. https://doi.org/10.1007/s00534-011-0460-z
Beppu T, Yamamura K, Sakamoto K et al (2022) Validation study of the JSHBPS nomogram for patients with colorectal liver metastases who underwent hepatic resection in the recent era - a nationwide survey in Japan. J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.1256
Beppu T, Miyamoto Y, Sakamoto Y et al (2014) Chemotherapy and targeted therapy for patients with initially unresectable colorectal liver metastases, focusing on conversion hepatectomy and long-term survival. Ann Surg Oncol 21(Suppl 3):S405–S413. https://doi.org/10.1245/s10434-014-3577-x
Mima K, Beppu T, Chikamoto A et al (2013) Hepatic resection combined with radiofrequency ablation for initially unresectable colorectal liver metastases after effective chemotherapy is a safe procedure with a low incidence of local recurrence. Int J Clin Oncol 18(5):847–855. https://doi.org/10.1007/s10147-012-0471-z
Imai K, Yamashita YI, Miyamoto Y et al (2019) Implication of primary tumor location for the indication of preoperative chemotherapy in patients with colorectal liver metastases. HPB (Oxford) 21(4):405–412. https://doi.org/10.1016/j.hpb.2018.08.012
Kanemitsu Y, Shimizu Y, Mizusawa J et al (2021) Hepatectomy Followed by mFOLFOX6 Versus Hepatectomy Alone for Liver-Only Metastatic Colorectal Cancer (JCOG0603): A Phase II or III Randomized Controlled Trial. J Clin Oncol 39(34):3789–3799. https://doi.org/10.1200/JCO.21.01032
Hasegawa K, Saiura A, Takayama T et al (2016) Adjuvant Oral Uracil-Tegafur with Leucovorin for Colorectal Cancer Liver Metastases: A Randomized Controlled Trial. PLoS ONE 11(9):e0162400. https://doi.org/10.1371/journal.pone.0162400
Ruspi L, Cananzi FCM, Aymerito F et al (2022) Measuring the impact of complications after surgery for retroperitoneal sarcoma: Is comprehensive complication index better than Clavien-Dindo Classification? Eur J Surg Oncol 48(5):978–984. https://doi.org/10.1016/j.ejso.2021.12.010
Tanaka T, Suda K, Inaba K et al (2019) Impact of Frailty on Postoperative Outcomes for Laparoscopic Gastrectomy in Patients Older than 80 Years. Ann Surg Oncol 26(12):4016–4026. https://doi.org/10.1245/s10434-019-07640-0
Yamada S, Shimada M, Morine Y et al (2021) Significance of Frailty in Prognosis After Hepatectomy for Elderly Patients with Hepatocellular Carcinoma. Ann Surg Oncol 28(1):439–446. https://doi.org/10.1245/s10434-020-08742-w
Takamoto T, Hashimoto T, Miyata A et al (2020) Repeat Hepatectomy After Major Hepatectomy for Colorectal Liver Metastases. J Gastrointest Surg 24(2):380–387. https://doi.org/10.1007/s11605-019-04154-8
Valenzuela CD, Moaven O, Gawdi R et al (2022) Outcomes after repeat hepatectomy for colorectal liver metastases from the colorectal liver operative metastasis international collaborative (COLOMIC). J Surg Oncol. https://doi.org/10.1002/jso.27056
Fried LP, Cohen AA, Xue QL et al (2021) The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging 1(1):36–46. https://doi.org/10.1038/s43587-020-00017-z
Zitvogel L, Pietrocola F, Kroemer G (2017) Nutrition, inflammation and cancer. Nat Immunol 18(8):843–850. https://doi.org/10.1038/ni.3754
Hiam-Galvez KJ, Allen BM, Spitzer MH (2021) Systemic immunity in cancer. Nat Rev Cancer 21(6):345–359. https://doi.org/10.1038/s41568-021-00347-z
Tanaka S, Ueno M, Iida H et al (2018) Preoperative assessment of frailty predicts age-related events after hepatic resection: a prospective multicenter study. J Hepatobiliary Pancreat Sci 25(8):377–387. https://doi.org/10.1002/jhbp.568
Ishihara A, Tanaka S, Ueno M et al (2021) Preoperative Risk Assessment for Delirium After Hepatic Resection in the Elderly: a Prospective Multicenter Study. J Gastrointest Surg 25(1):134–144. https://doi.org/10.1007/s11605-020-04562-1
Kaibori M, Ishizaki M, Matsui K et al (2016) Geriatric assessment as a predictor of postoperative complications in elderly patients with hepatocellular carcinoma. Langenbecks Arch Surg 401(2):205–214. https://doi.org/10.1007/s00423-016-1388-1
Kaibori M, Matsushima H, Ishizaki M et al (2021) Perioperative Geriatric Assessment as A Predictor of Long-Term Hepatectomy Outcomes in Elderly Patients with Hepatocellular Carcinoma. Cancers (Basel). https://doi.org/10.3390/cancers13040842
Acknowledgements
We would like to thank Editage (www.editage.cn) for editing this manuscript.
Funding
This study was funded by the Takeda Science Foundation, the Kobayashi Foundation for Cancer Research, and the Japanese Foundation For Multidisciplinary Treatment of Cancer.
Author information
Authors and Affiliations
Contributions
Study concepts: KM. Study design: KM. Data acquisition: YA, TT, TO, KK, DO, SY, TM, RI, YK, SN, HO. Quality control of data and algorithms: KM, HH. Data analysis and interpretation: KM, HH, HB. Statistical analysis: KM. Manuscript preparation: KM. Manuscript editing: KM, HH. Manuscript review: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest for this article.
Ethics statement
This study was approved by the Human Ethics Review Committee of Kumamoto University Hospital, Kumamoto, Japan (institutional ethics committee number: 2220). The requirement for written informed consent was waived owing to the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Mima, K., Hayashi, H., Adachi, Y. et al. Patient vulnerability is associated with poor prognosis following upfront hepatectomy for colorectal liver metastasis. Int J Clin Oncol 29, 47–54 (2024). https://doi.org/10.1007/s10147-023-02429-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-023-02429-4