Abstract
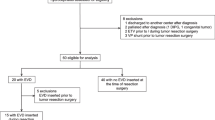
An external ventricular drain (EVD) is used to facilitate cerebrospinal fluid (CSF) removal in medulloblastoma patients suffering from hydrocephalus. It is essential to recognize that EVD management plays a crucial role in influencing the incidence of drain-related complications. However, the ideal method for EVD management remains undetermined. Our research sought to examine the safety of EVD placement and the impact of EVD on the incidences of intracranial infections, postresection hydrocephalus, and posterior fossa syndrome (PFS). We conducted a single-center observational study involving a cohort of 120 pediatric medulloblastoma patients who were treated from 2017 to 2020. The rates of intracranial infection, postresection hydrocephalus, and PFS were 9.2%, 18.3%, and 16.7%, respectively. EVD did not influence the occurrence of intracranial infection (p = 0.466), postresection hydrocephalus (p = 0.298), or PFS (p = 0.212). A gradual EVD weaning protocol correlated with an elevated incidence of postresection hydrocephalus (p = 0.033), whereas a rapid weaning approach resulted in 4.09 ± 0.44 fewer drainage days (p < 0.001) than the gradual weaning strategy. EVD placement (p = 0.010) and intracranial infection (p = 0.002) were linked to delayed speech return, whereas a longer duration of drainage was conducive to the recovery of language function (p = 0.010). EVD insertion was not correlated with the incidence of intracranial infection, postoperative hydrocephalus, or PFS. The optimal EVD management method should encompass a rapid EVD weaning strategy, followed by prompt drain closure. We have presented additional evidence to improve the safety of EVD insertion and management in neurosurgical patients to ultimately facilitate the establishment of standardized institutional/national implementation and management protocols.




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Srinivasan HL, Foster MT, van Baarsen K, Hennigan D, Pettorini B, Mallucci C (2020) Does pre-resection endoscopic third ventriculostomy prevent the need for post-resection CSF diversion after pediatric posterior fossa tumor excision? A historical cohort study and review of the literature. J Neurosurg Pediatr 1–10. https://doi.org/10.3171/2019.12.Peds19539
El-Ghandour NM (2011) Endoscopic third ventriculostomy versus ventriculoperitoneal shunt in the treatment of obstructive hydrocephalus due to posterior fossa tumors in children. Child’s Nerv Syst 27:117–126. https://doi.org/10.1007/s00381-010-1263-2
Di Rocco F, Jucá CE, Zerah M, Sainte-Rose C (2013) Endoscopic third ventriculostomy and posterior fossa tumors. World Neurosurg 79:S18.e15-19. https://doi.org/10.1016/j.wneu.2012.02.018
Fried HI, Nathan BR, Rowe AS, Zabramski JM, Andaluz N, Bhimraj A et al (2016) The insertion and management of external ventricular drains: an evidence-based consensus statement : a statement for healthcare professionals from the Neurocritical Care Society. Neurocrit Care 24:61–81. https://doi.org/10.1007/s12028-015-0224-8
Dakson A, Kameda-Smith M, Staudt MD, Lavergne P, Makarenko S, Eagles ME et al (2021) A nationwide prospective multicenter study of external ventricular drainage: accuracy, safety, and related complications. J Neurosurg 1–9. https://doi.org/10.3171/2021.7.Jns21421
Saad H, Bray DP, McMahon JT, Philbrick BD, Dawoud RA, Douglas JM et al (2021) Permanent cerebrospinal fluid diversion in adults with posterior fossa tumors: incidence and predictors. Neurosurgery 89:987–996. https://doi.org/10.1093/neuros/nyab341
Ashida R, Nazar N, Edwards R, Teo M (2021) Cerebellar mutism syndrome: an overview of the pathophysiology in relation to the cerebrocerebellar anatomy, risk factors, potential treatments, and outcomes. World Neurosurg 153:63–74. https://doi.org/10.1016/j.wneu.2021.06.065
Renne B, Radic J, Agrawal D, Albrecht B, Bonfield CM, Cohrs G et al (2020) Cerebellar mutism after posterior fossa tumor resection in children: a multicenter international retrospective study to determine possible modifiable factors. Child’s Nerv Syst 36:1159–1169. https://doi.org/10.1007/s00381-019-04058-7
Khan RB, Patay Z, Klimo P, Huang J, Kumar R, Boop FA et al (2021) Clinical features, neurologic recovery, and risk factors of postoperative posterior fossa syndrome and delayed recovery: a prospective study. Neuro Oncol 23:1586–1596. https://doi.org/10.1093/neuonc/noab030
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet (London, England) 370:1453–1457. https://doi.org/10.1016/s0140-6736(07)61602-x
Kahle KT, Kulkarni AV, Limbrick DD Jr, Warf BC (2016) Hydrocephalus in children. Lancet (London, England) 387:788–799. https://doi.org/10.1016/s0140-6736(15)60694-8
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332. https://doi.org/10.1016/j.ajic.2008.03.002
Gudrunardottir T, Morgan AT, Lux AL, Walker DA, Walsh KS, Wells EM et al (2016) Consensus paper on post-operative pediatric cerebellar mutism syndrome: the Iceland Delphi results. Child’s Nerv Syst 32:1195–1203. https://doi.org/10.1007/s00381-016-3093-3
Wickenhauser ME, Khan RB, Raches D, Ashford JM, Robinson GW, Russell KM, Conklin HM (2020) Characterizing posterior fossa syndrome: a survey of experts. Pediatr Neurol 104:19–22. https://doi.org/10.1016/j.pediatrneurol.2019.11.007
Chang CH, Housepian EM, Herbert C Jr (1969) An operative staging system and a megavoltage radiotherapeutic technic for cerebellar medulloblastomas. Radiology 93:1351–1359. https://doi.org/10.1148/93.6.1351
Yu YL, Lee MS, Juan CJ, Hueng DY (2013) Calculating the tumor volume of acoustic neuromas: comparison of ABC/2 formula with planimetry method. Clin Neurol Neurosurg 115:1371–1374. https://doi.org/10.1016/j.clineuro.2012.12.029
Lescher S, Schniewindt S, Jurcoane A, Senft C, Hattingen E (2014) Time window for postoperative reactive enhancement after resection of brain tumors: less than 72 hours. Neurosurg Focus 37:E3. https://doi.org/10.3171/2014.9.Focus14479
Peduzzi P, Concato J, Feinstein AR, Holford TR (1995) Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol 48:1503–1510. https://doi.org/10.1016/0895-4356(95)00048-8
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49:1373–1379. https://doi.org/10.1016/s0895-4356(96)00236-3
Sáenz A, Badaloni E, Grijalba M, Villalonga JF, Argañaraz R, Mantese B (2021) Risk factors for surgical site infection in pediatric posterior fossa tumors. Child’s Nerv Syst 37:3049–3056. https://doi.org/10.1007/s00381-021-05256-y
Kourbeti IS, Vakis AF, Ziakas P, Karabetsos D, Potolidis E, Christou S, Samonis G (2015) Infections in patients undergoing craniotomy: risk factors associated with post-craniotomy meningitis. J Neurosurg 122:1113–1119. https://doi.org/10.3171/2014.8.Jns132557
Hosainey SAM, Lykkedrang BL, Meling TR (2022) Long-term risk of shunt failure after brain tumor surgery. Neurosurg Rev 45:1589–1600. https://doi.org/10.1007/s10143-021-01648-5
Won SY, Dubinski D, Behmanesh B, Bernstock JD, Seifert V, Konczalla J et al (2020) Management of hydrocephalus after resection of posterior fossa lesions in pediatric and adult patients-predictors for development of hydrocephalus. Neurosurg Rev 43:1143–1150. https://doi.org/10.1007/s10143-019-01139-8
Sun T, Gao L, Li F, Shi Y, Xie F, Wang J et al (2017) Workplace violence, psychological stress, sleep quality and subjective health in Chinese doctors: a large cross-sectional study. BMJ Open 7:e017182. https://doi.org/10.1136/bmjopen-2017-017182
Huang M, Wang J, Ni X, Chen G, Kong L (2016) Neurocritical care in china: past, present, and future. World Neurosurg 95:502–506. https://doi.org/10.1016/j.wneu.2016.06.102
[Anonymous] (2010) Chinese doctors are under threat. Lancet (London, England) 376: 657. https://doi.org/10.1016/s0140-6736(10)61315-3
Braddock CH 3rd (2010) The emerging importance and relevance of shared decision making to clinical practice. Med Decis Mak 30:5s–7s. https://doi.org/10.1177/0272989x10381344
Chung DY, Thompson BB, Kumar MA, Mahta A, Rao SS, Lai JH et al (2022) Association of external ventricular drain wean strategy with shunt placement and length of stay in subarachnoid hemorrhage: a prospective multicenter study. Neurocrit Care 36:536–545. https://doi.org/10.1007/s12028-021-01343-9
Olson DM, Zomorodi M, Britz GW, Zomorodi AR, Amato A, Graffagnino C (2013) Continuous cerebral spinal fluid drainage associated with complications in patients admitted with subarachnoid hemorrhage. J Neurosurg 119:974–980. https://doi.org/10.3171/2013.6.Jns122403
Rao SS, Chung DY, Wolcott Z, Sheriff F, Khawaja AM, Lee H et al (2019) Intermittent CSF drainage and rapid EVD weaning approach after subarachnoid hemorrhage: association with fewer VP shunts and shorter length of stay. J Neurosurg 132:1583–1588. https://doi.org/10.3171/2019.1.Jns182702
Mead PA, Safdieh JE, Nizza P, Tuma S, Sepkowitz KA (2014) Ommaya reservoir infections: a 16-year retrospective analysis. J Infect 68:225–230. https://doi.org/10.1016/j.jinf.2013.11.014
Szvalb AD, Raad II, Weinberg JS, Suki D, Mayer R, Viola GM (2014) Ommaya reservoir-related infections: clinical manifestations and treatment outcomes. J Infect 68:216–224. https://doi.org/10.1016/j.jinf.2013.12.002
Lang SS, Zhang B, Yver H, Palma J, Kirschen MP, Topjian AA et al (2019) Reduction of ventriculostomy-associated CSF infection with antibiotic-impregnated catheters in pediatric patients: a single-institution study. Neurosurg Focus 47:E4. https://doi.org/10.3171/2019.5.Focus19279
Pople I, Poon W, Assaker R, Mathieu D, Iantosca M, Wang E et al (2012) Comparison of infection rate with the use of antibiotic-impregnated vs standard extraventricular drainage devices: a prospective, randomized controlled trial. Neurosurgery 71:6–13. https://doi.org/10.1227/NEU.0b013e3182544e31
Zabramski JM, Whiting D, Darouiche RO, Horner TG, Olson J, Robertson C, Hamilton AJ (2003) Efficacy of antimicrobial-impregnated external ventricular drain catheters: a prospective, randomized, controlled trial. J Neurosurg 98:725–730. https://doi.org/10.3171/jns.2003.98.4.0725
Ortolano F, Carbonara M, Stanco A, Civelli V, Carrabba G, Zoerle T, Stocchetti N (2017) External ventricular drain causes brain tissue damage: an imaging study. Acta Neurochir 159:1981–1989. https://doi.org/10.1007/s00701-017-3291-0
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Zaiyu Zhang, Yuxin Wu, and Xueling Zhao. The first draft of the manuscript was written by Zaiyu Zhang. Yuxin Wu, Xueling Zhao, Jianju Zhou, Xuan Zhai, Lusheng Li, and Ping Liang revised it critically for important intellectual content. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Children's Hospital of Chongqing Medical University (No. 2021405).
Consent to participate
Written informed consent was obtained from the patients or their parents.
Consent to publish
This manuscript did not contain any individual person's data in any form (including any individual details, images, or videos).
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Z., Wu, Y., Zhao, X. et al. The insertion and management of an external ventricular drain in pediatric patients with hydrocephalus associated with medulloblastoma. Neurosurg Rev 46, 170 (2023). https://doi.org/10.1007/s10143-023-02080-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02080-7