Abstract
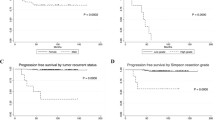
This study aimed to assess the risk factors for the recurrence of WHO grade I intracranial meningiomas using the Brain Tumor Registry of Japan (BTRJ) database. We extracted the data of 4641 patients with intracranial WHO grade I meningiomas treated only by surgical resection between 2001 and 2008. We conducted complete data analysis (n = 3690) and multiple imputation analysis (n = 4641) to adjust for missing data on tumor size. The influence of factors including age, sex, size, extent of resection, location, and preoperative symptoms on PFS was assessed. Univariate analyses of the complete data set showed that age did not affect PFS; however, male sex (p < 0.001), tumor size ≥ 30 mm (p < 0.001), low extent of resection, tumor location at the skull base (p < 0.001), and the presence of preoperative symptoms (p < 0.001) were risk factors for a significantly shorter PFS. Multivariate analysis demonstrated that male sex (p < 0.001) and presence of preoperative symptoms (p = 0.027) were independent risk factors for shorter PFS alongside large tumor size (p < 0.001) and non-gross total resection (p < 0.001). These results were confirmed for the imputed dataset. While most previous large nationwide studies of meningiomas have evaluated overall survival, progression-free survival has yet to be thoroughly examined. This study suggests that even histologically benign meningiomas may have a sex difference in postoperative behavior. This observation may provide clues to understanding the mechanism of meningioma cell proliferation.


Similar content being viewed by others
Data availability
The de-identified participant data presented in this study are available upon request from a qualified investigator to replicate the results.
References
Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS (2018) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro-Oncol 20:iv1–iv86. https://doi.org/10.1093/neuonc/noy131
Goldbrunner R, Stavrinou P, Jenkinson MD, Sahm F, Mawrin C, Weber DC, Preusser M, Minniti G, Lund-Johansen M, Lefranc F, Houdart E, Sallabanda K, Rhun EL, Nieuwenhuizen D, Tabatabai G, Soffietti R, Weller M (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro-Oncol 23:1821–1834. https://doi.org/10.1093/neuonc/noab150
National Comprehensive Cancer Network. NCCN: NCCN guide-lines: central nervous system cancers. NCCN.org (http://www.nccn.org/). Accessed 25 June 2022.
Hasseleid BF, Meling TR, Rønning P, Scheie D, Helseth E (2012) Surgery for convexity meningioma: Simpson Grade I resection as the goal. J Neurosurg 117:999–1006. https://doi.org/10.3171/2012.9.jns12294
Oya S, Kawai K, Nakatomi H, Saito N (2012) Significance of Simpson grading system in modern meningioma surgery: integration of the grade with MIB-1 labeling index as a key to predict the recurrence of WHO Grade I meningiomas: Clinical article. J Neurosurg 117:121–128. https://doi.org/10.3171/2012.3.jns111945
Sughrue ME, Kane AJ, Shangari G, Rutkowski MJ, McDermott MW, Berger MS, Parsa AT (2010) The relevance of Simpson Grade I and II resection in modern neurosurgical treatment of World Health Organization Grade I meningiomas: Clinical article. J Neurosurg 113:1029–1035. https://doi.org/10.3171/2010.3.jns091971
Amsbaugh M, Ugiliweneza B, Burton E, Skirboll S, Woo S, Boakye M (2016) Patterns of care and outcomes of adjuvant radiotherapy for meningiomas: a Surveillance, Epidemiology, and End Results and Medicare linked analysis. Cureus 8:e567. https://doi.org/10.7759/cureus.567
Brodbelt AR, Barclay ME, Greenberg D, Williams M, Jenkinson MD, Karabatsou K (2019) The outcome of patients with surgically treated meningioma in England: 1999–2013. A cancer registry data analysis. Brit J Neurosurg 33:1–7. https://doi.org/10.1080/02688697.2019.1661965
Cahill KS, Claus EB (2011) Treatment and survival of patients with nonmalignant intracranial meningioma: results from the Surveillance, Epidemiology, and End Results Program of the National Cancer Institute: Clinical article. J Neurosurg 115:259–267. https://doi.org/10.3171/2011.3.jns101748
Corell A, Thurin E, Skoglund T, Farahmand D, Henriksson R, Rydenhag B, Gulati S, Bartek J, Jakola AS (2019) Neurosurgical treatment and outcome patterns of meningioma in Sweden: a nationwide registry-based study. Acta Neurochir (Wien) 161:333–341. https://doi.org/10.1007/s00701-019-03799-3
Reddy AK, Ryoo JS, Denyer S, McGuire LS, Mehta AI (2019) Determining the role of adjuvant radiotherapy in the management of meningioma: a Surveillance, Epidemiology, and End Results analysis. Neurosurg Focus 46:E3. https://doi.org/10.3171/2019.3.focus1971
Narita Y, Shibui S, Society OB of the C of BTR of JS by the JN (2015) Trends and outcomes in the treatment of gliomas based on data during 2001–2004 from the Brain Tumor Registry of Japan. Neurol Med Chir (Tokyo) 55:286–295. https://doi.org/10.2176/nmc.ra.2014-0348
Committee of Brain Tumor Registry of Japan Supported by the Japan Neurosurgical Society (1977) Report of Brain Tumor Registry of Japan 1969 and 1974. 1:1–45.
Committee of Brain Tumor Registry of Japan Supported by the Japan Neurosurgical Society (2014) Brain Tumor Registry of Japan (2001–2004). Neurol Med Chir (Tokyo) 1–102.
Committee of Brain Tumor Registry of Japan Supported by the Japan Neurosurgical Society (2017) Brain Tumor Registry of Japan (2005–2008). Neurol Med-chir 57:9–102. https://doi.org/10.2176/nmc.sup.2017-0001
Yoshimoto K, Kada A, Kuga D, Hatae R, Murata H, Akagi Y, Nishimura K, Kurogi R, Nishimura A, Hata N, Mizoguchi M, Sayama T, Iihara K (2016) Current trends and healthcare resource usage in the in hospital treatment of primary malignant brain tumor in Japan: a national survey using the diagnostic procedure combination database (J-ASPECT Study-Brain Tumor). Neurol Med Chir (Tokyo) 56:664–673. https://doi.org/10.2176/nmc.oa.2016-0172
Driver J, Hoffman SE, Tavakol S, Woodward E, Maury EA, Bhave V, Greenwald NF, Nassiri F, Aldape K, Zadeh G, Choudhury A, Vasudevan HN, Magill ST, Raleigh DR, Abedalthagafi M, Aizer AA, Alexander BM, Ligon KL, Reardon DA, Wen PY, Al-Mefty O, Ligon AH, Dubuc AM, Beroukhim R, Claus EB, Dunn IF, Santagata S, Bi WL (2021) A molecularly integrated grade for meningioma. Neuro-Oncol 24:796–808. https://doi.org/10.1093/neuonc/noab213
Maillo A, Orfao A, Espinosa AB, Sayagués JM, Merino M, Sousa P, Lara M, Tabernero MD (2007) Early recurrences in histologically benign/grade I meningiomas are associated with large tumors and coexistence of monosomy 14 and del(1p36) in the ancestral tumor cell clone. Neuro-Oncol 9:438–446. https://doi.org/10.1215/15228517-2007-026
Brokinkel B, Spille DC, Brokinkel C, Hess K, Paulus W, Bormann E, Stummer W (2020) The Simpson grading: defining the optimal threshold for gross total resection in meningioma surgery. Neurosurg Rev 9:35974–35978. https://doi.org/10.1007/s10143-020-01369-1
Gousias K, Schramm J, Simon M (2016) The Simpson grading revisited: aggressive surgery and its place in modern meningioma management. J Neurosurg 125:551–560. https://doi.org/10.3171/2015.9.jns15754
Marciscano AE, Stemmer-Rachamimov AO, Niemierko A, Larvie M, Curry WT, Barker FG, Martuza RL, McGuone D, Oh KS, Loeffler JS, Shih HA (2015) Benign meningiomas (WHO Grade I) with atypical histological features: correlation of histopathological features with clinical outcomes. J Neurosurg 124:106–114. https://doi.org/10.3171/2015.1.jns142228
Nanda A, Bir SC, Maiti TK, Konar SK, Missios S, Guthikonda B (2016) Relevance of Simpson grading system and recurrence-free survival after surgery for World Health Organization Grade I meningioma. J Neurosurg 126:1–11. https://doi.org/10.3171/2016.1.jns151842
Voß KM, Spille DC, Sauerland C, Molina ES, Brokinkel C, Paulus W, Stummer W, Holling M, Jeibmann A, Brokinkel B (2017) The Simpson grading in meningioma surgery: does the tumor location influence the prognostic value? J Neuro-oncol 133:641–651. https://doi.org/10.1007/s11060-017-2481-1
Winther TL, Torp SH (2017) Significance of the extent of resection in modern neurosurgical practice of World Health Organization grade I meningiomas. World Neurosurg 99:104–110. https://doi.org/10.1016/j.wneu.2016.11.034
Claus EB, Calvocoressi L, Bondy ML, Wrensch M, Wiemels JL, Schildkraut JM (2013) Exogenous hormone use, reproductive factors, and risk of intracranial meningioma in females: Clinical article. J Neurosurg 118:649–656. https://doi.org/10.3171/2012.9.jns12811
Khalid H (1994) Immunohistochemical study of estrogen receptor-related antigen, progesterone and estrogen receptors in human intracranial meningiomas. Cancer 74:679–685. https://doi.org/10.1002/1097-0142(19940715)74:2%3c679::aid-cncr2820740221%3e3.0.co;2-f
Pravdenkova S, Al-Mefty O, Sawyer J, Husain M (2006) Progesterone and estrogen receptors: opposing prognostic indicators in meningiomas. J Neurosurg 105:163–173. https://doi.org/10.3171/jns.2006.105.2.163
Kane AJ, Sughrue ME, Rutkowski MJ, Shangari G, Fang S, McDermott MW, Berger MS, Parsa AT (2011) Anatomic location is a risk factor for atypical and malignant meningiomas. Cancer 117:1272–1278. https://doi.org/10.1002/cncr.25591
Mahmood A, Qureshi NH, Malik GM (1994) Intracranial meningiomas: analysis of recurrence after surgical treatment. Acta Neurochir (Wien) 126:53–58. https://doi.org/10.1007/bf01476410
Rohringer M, Sutherland GR, Louw DF, Sima AAF (1989) Incidence and clinicopathological features of meningioma. J Neurosurg 71:665–672. https://doi.org/10.3171/jns.1989.71.5.0665
Silva JM, Wippel HH, Santos MDM, Verissimo DCA, Santos RM, Nogueira FCS, Passos GAR, Sprengel SL, Borba LAB, Carvalho PC, Fischer de da JSG (2020) Proteomics pinpoints alterations in grade I meningiomas of male versus female patients. Sci Rep 10:10335. https://doi.org/10.1038/s41598-020-67113-3
Commins DL, Atkinson RD, Burnett ME (2007) Review of meningioma histopathology. Neurosurg Focus 23:E3. https://doi.org/10.3171/foc-07/10/e3
Perry A (2007) World Health Organization classification of tumours of the central nervous system
Schildkraut JM, Calvocoressi L, Wang F, Wrensch M, Bondy ML, Wiemels JL, Claus EB (2014) Endogenous and exogenous hormone exposure and the risk of meningioma in men: clinical article. J Neurosurg 120:820–826. https://doi.org/10.3171/2013.12.jns131170
Englot DJ, Magill ST, Han SJ, Chang EF, Berger MS, McDermott MW (2016) Seizures in supratentorial meningioma: a systematic review and meta-analysis. J Neurosurg 124:1552–1561. https://doi.org/10.3171/2015.4.jns142742
Oya S, Ikawa F, Ichihara N, Wanibuchi M, Akiyama Y, Nakatomi H, Mikuni N, Narita Y (2020) Nation-wide brain tumor registry-based study of intracranial meningioma in Japan: analysis of surgery-related risks. Neurol Med Chir (Tokyo) oa.2020–0304. https://doi.org/10.2176/nmc.oa.2020-0304
Ding Y, Qiu L, Xu Q, Song L, Yang S, Yang T (2014) Relationships between tumor microenvironment and clinicopathological parameters in meningioma. Int J Clin Exp Pathol 7:6973–6979
Proctor DT, Huang J, Lama S, Albakr A, Marle GV, Sutherland GR (2019) Tumor-associated macrophage infiltration in meningioma. Neurooncology Adv 1:vdz018. https://doi.org/10.1093/noajnl/vdz018
Sahm F, Schrimpf D, Stichel D, Jones DTW, Hielscher T, Schefzyk S, Okonechnikov K, Koelsche C, Reuss DE, Capper D, Sturm D, Wirsching H-G, Berghoff AS, Baumgarten P, Kratz A, Huang K, Wefers AK, Hovestadt V, Sill M, Ellis HP, Kurian KM, Okuducu AF, Jungk C, Drueschler K, Schick M, Bewerunge-Hudler M, Mawrin C, Seiz-Rosenhagen M, Ketter R, Simon M, Westphal M, Lamszus K, Becker A, Koch A, Schittenhelm J, Rushing EJ, Collins VP, Brehmer S, Chavez L, Platten M, Hänggi D, Unterberg A, Paulus W, Wick W, Pfister SM, Mittelbronn M, Preusser M, Herold-Mende C, Weller M, von Deimling A (2017) DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol 18:682–694. https://doi.org/10.1016/s1470-2045(17)30155-9
Oya S, Kim SH, Sade B, Lee JH (2011) The natural history of intracranial meningiomas: Clinical article. J Neurosurg 114:1250–1256. https://doi.org/10.3171/2010.12.jns101623
Löfgren D, Valachis A, Olivecrona M (2022) Older meningioma patients: a retrospective population-based study of risk factors for morbidity and mortality after neurosurgery. Acta Neurochir (Wien) 164(11):2987–2997. https://doi.org/10.1007/s00701-022-05336-1
Acknowledgements
The authors thank all members of the Japan Neurosurgical Society for their cooperation in regularly registering their data and keeping the BTRJ up to date.
Author information
Authors and Affiliations
Contributions
Conception and design: SO. Acquisition of data: SO and FI. Data analysis and interpretation: SO, FI, and NI. Drafting of the article: SO. Critical revision of the article: all authors. Reviewed submitted version of the manuscript: all authors. All the authors approved the final version of the manuscript. Statistical analysis: SO and NI. Administrative technical/material support: MW, YA, HN, and NM. Study supervision: YN.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study was approved by the institutional review board of Saitama Medical Center, Saitama Medical University (No. 1527-IV), and by the Japan Neurosurgical Society (No. 2019007). The requirement for written informed consent from patients was waived by the above-mentioned boards owing to the use of retrospective anonymized data.
Consent for publication
The requirement for written informed consent from patients for publication was waived owing to the use of retrospective anonymous data. Patients were given the opportunity to opt out of the study on our hospital website.
Human and animal ethics
All reported analyses involving human participants in this study were performed in accordance with the ethical standards established in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous presentations: None.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oya, S., Ikawa, F., Ichihara, N. et al. Male sex and presence of preoperative symptoms are associated with early recurrence of WHO grade I meningiomas after surgical resection: analysis from the nationwide Brain Tumor Registry of Japan. Neurosurg Rev 46, 10 (2023). https://doi.org/10.1007/s10143-022-01907-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-022-01907-z