Abstract
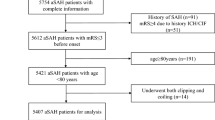
Aneurysmal subarachnoid hemorrhage (aSAH) is the most devastating form of stroke. Up to now, little is known about the effect of sex differences on complications and outcomes. We retrospectively reviewed aSAH patients admitted to our institution between January 2015 and December 2020. The functional outcomes at discharge and 90 days after discharge were assessed using the modified Rankin Scale (mRS). Baseline characteristics, in-hospital complications, and outcomes were compared after 1:1 propensity score matching (PSM). The area under the curve (AUC) in the receiver operating characteristic curve (ROC) analysis was calculated to measure each independent risk factor’s prediction ability. A total of 833 patients were included. After PSM, 109 male patients were compared with 109 female patients. Female patients had a higher incidence of anemia (47/109 [43.1%] vs. 30/109 [27.5%], p = 0.016) than male patients, while male patients had a higher incidence of pneumonia (36/109 [33.0%] vs. 19/109 [17.4%], p = 0.008) than female patients. No significant differences were found in the rate of unfavorable outcomes at discharge and 90-day outcomes (40/109 [36.7%] vs. 50/109 [45.9%], p = 0.169; 15/109 [13.8%] vs. 19/107 [17.8%], p = 0.420) between female and male patients. Pneumonia (AUC = 0.749, 95% confidence interval [CI] = 0.623–0.875, p < 0.001) and anemia (AUC = 0.753, 95% CI = 0.632–0.873, p = 0.002) showed good ability to predict 90-day unfavorable outcomes in male and female patients, respectively. Female patients had a higher incidence of anemia but a lower incidence of pneumonia during hospitalization. However, differences in in-hospital complications did not result in differences in outcomes between women and men. Clinical Trial Registration: NCT04785976. 2021/03/05, retrospectively registered.

Similar content being viewed by others
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Code availability
N/A.
References
Lovelock CE, Rinkel GJ, Rothwell PM (2010) Time trends in outcome of subarachnoid hemorrhage: Population-based study and systematic review. Neurology 74:1494–1501. https://doi.org/10.1212/WNL.0b013e3181dd42b3
Schatlo B, Fung C, Fathi AR, Sailer M, Winkler K, Daniel RT, Bijlenga P, Ahlborn P, Seule M, Zumofen D, Reinert M, Woernle C, Stienen M, Levivier M, Hildebrandt G, Mariani L, Bernays R, Fandino J, Raabe A, Keller E, Schaller K (2012) Introducing a nationwide registry: the Swiss study on aneurysmal subarachnoid haemorrhage (Swiss SOS). Acta Neurochir (Wien) 154:2173–2178; discussion 2178. https://doi.org/10.1007/s00701-012-1500-4
Duijghuisen JJ, Greebe P, Nieuwkamp DJ, Algra A, Rinkel GJ (2016) Sex-related differences in outcome in patients with aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis 25:2067–2070. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.04.018
Hamdan A, Barnes J, Mitchell P (2014) Subarachnoid hemorrhage and the female sex: analysis of risk factors, aneurysm characteristics, and outcomes. J Neurosurg 121:1367–1373. https://doi.org/10.3171/2014.7.JNS132318
Kongable GL, Lanzino G, Germanson TP, Truskowski LL, Alves WM, Torner JC, Kassell NF (1996) Gender-related differences in aneurysmal subarachnoid hemorrhage. J Neurosurg 84:43–48. https://doi.org/10.3171/jns.1996.84.1.0043
Nichols L, Stirling C, Otahal P, Stankovich J, Gall S (2018) Socioeconomic disadvantage is associated with a higher incidence of aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis 27:660–668. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.09.055
Rehman S, Chandra R, Zhou K, Tan D, Lai L, Asadi H, Froelich J, Thani N, Nichols L, Blizzard L, Smith K, Thrift A, Stirling C, Callisaya M, Breslin M, Reeves M, Gall S (2020) Sex differences in aneurysmal subarachnoid haemorrhage (aSAH): aneurysm characteristics, neurological complications, and outcome. Acta Neurochir 162:2271–2282. https://doi.org/10.1007/s00701-020-04469-5
Wang YX, He J, Zhang L, Li Y, Zhao L, Liu H, Yang L, Zeng XJ, Yang J, Peng GM, Ahuja A, Yang ZH (2016) A higher aneurysmal subarachnoid hemorrhage incidence in women prior to menopause: a retrospective analysis of 4,895 cases from eight hospitals in China. Quant Imaging Med Surg 6:151–156. https://doi.org/10.21037/qims.2016.01.06
Fuentes A, Stone McGuire L, Amin-Hanjani S (2022) Sex Differences in cerebral aneurysms and subarachnoid hemorrhage. Stroke 53:624–633. https://doi.org/10.1161/strokeaha.121.037147
Li R, Lin F, Chen Y, Lu J, Han H, Ma L, Zhao Y, Yan D, Li R, Yang J, He S, Li Z, Zhang H, Yuan K, Wang K, Hao Q, Ye X, Wang H, Li H, Zhang L, Shi G, Zhou J, Zhao Y, Zhang Y, Li Y, Wang S, Chen X, Zhao Y (2022) A 90-day prognostic model based on the early brain injury indicators after aneurysmal subarachnoid hemorrhage: the TAPS Score. Transl Stroke Res. https://doi.org/10.1007/s12975-022-01033-4
Li R, Lin F, Chen Y, Lu J, Han H, Yan D, Li R, Yang J, Li Z, Zhang H, Yuan K, Jin Y, Hao Q, Li H, Zhang L, Shi G, Zhou J, Zhao Y, Zhang Y, Li Y, Wang S, Chen X, Zhao Y (2021) In-hospital complication-related risk factors for discharge and 90-day outcomes in patients with aneurysmal subarachnoid hemorrhage after surgical clipping and endovascular coiling: a propensity score-matched analysis. Journal of neurosurgery:1–12. https://doi.org/10.3171/2021.10.Jns211484
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL, Kirkness CJ, Naidech AM, Ogilvy CS, Patel AB, Thompson BG, Vespa P, American Heart Association Stroke C, Council on Cardiovascular Radiology and Intervention, Council on Cardiovascular N, Council on Cardiovascular Surgery and Anesthesia, Council on Clinical C (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke 43:1711–1737. https://doi.org/10.1161/STR.0b013e3182587839
de Rooij N, Rinkel G, Dankbaar J, Frijns C (2013) Delayed cerebral ischemia after subarachnoid hemorrhage: a systematic review of clinical, laboratory, and radiological predictors. Stroke 44:43–54. https://doi.org/10.1161/strokeaha.112.674291
Dhar R, Diringer M (2008) The burden of the systemic inflammatory response predicts vasospasm and outcome after subarachnoid hemorrhage. Neurocrit Care 8:404–412. https://doi.org/10.1007/s12028-008-9054-2
Dorhout Mees SM, van Dijk GW, Algra A, Kempink DR, Rinkel GJ (2003) Glucose levels and outcome after subarachnoid hemorrhage. Neurology 61:1132–1133. https://doi.org/10.1212/01.wnl.0000090466.68866.02
Duan W, Pan Y, Wang C, Wang Y, Zhao X, Wang Y, Liu L, Investigators C (2018) Risk factors and clinical impact of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage: analysis from the China National Stroke Registry. Neuroepidemiology 50:128–136. https://doi.org/10.1159/000487325
English SW, Chasse M, Turgeon AF, Lauzier F, Griesdale D, Garland A, Fergusson D, Zarychanski R, van Walraven C, Montroy K, Ziegler J, Dupont-Chouinard R, Carignan R, Dhaliwal A, Mallick R, Sinclair J, Boutin A, Pagliarello G, Tinmouth A, McIntyre L, Canadian Critical Care Trials G (2018) Anemia prevalence and incidence and red blood cell transfusion practices in aneurysmal subarachnoid hemorrhage: results of a multicenter cohort study. Crit Care 22:169. https://doi.org/10.1186/s13054-018-2089-7
Germans MR, Jaja BNR, de Oliviera Manoel AL, Cohen AH, Macdonald RL (2018) Sex differences in delayed cerebral ischemia after subarachnoid hemorrhage. J Neurosurg 129:458–464. https://doi.org/10.3171/2017.3.JNS162808
Nieuwkamp DJ, Vaartjes I, Algra A, Bots ML, Rinkel GJ (2013) Age- and gender-specific time trend in risk of death of patients admitted with aneurysmal subarachnoid hemorrhage in the Netherlands. Int J Stroke 8(Suppl A100):90–94. https://doi.org/10.1111/ijs.12006
Rehman S, Chandra RV, Zhou K, Tan D, Lai L, Asadi H, Froelich J, Thani N, Nichols L, Blizzard L, Smith K, Thrift AG, Stirling C, Callisaya ML, Breslin M, Reeves MJ, Gall S (2020) Sex differences in aneurysmal subarachnoid haemorrhage (aSAH): aneurysm characteristics, neurological complications, and outcome. Acta Neurochir (Wien) 162:2271–2282. https://doi.org/10.1007/s00701-020-04469-5
Sheehan JP, Polin RS, Sheehan JM, Baskaya MK, Kassell NF (1999) Factors associated with hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurgery 45:1120–1127; discussion 1127–1128. https://doi.org/10.1097/00006123-199911000-00021
Yu W (2022) Vasospasm and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage: recent advances and future directions in translational research. Transl Stroke Res. https://doi.org/10.1007/s12975-022-01028-1
Wu M, Chen Y, Li Z, Gu H, Yang K, Xiong Y, Wang Y, Wang C (2022) Dysphagia screening and pneumonia after subarachnoid hemorrhage: findings from the Chinese stroke center alliance. CNS Neurosci Ther 28:913–921. https://doi.org/10.1111/cns.13822
Cinotti R, Dordonnat-Moynard A, Feuillet F, Roquilly A, Rondeau N, Lepelletier D, Caillon J, Asseray N, Blanloeil Y, Rozec B, Asehnoune K (2014) Risk factors and pathogens involved in early ventilator-acquired pneumonia in patients with severe subarachnoid hemorrhage. Eur J Clin Microbiol Infect Dis 33:823–830. https://doi.org/10.1007/s10096-013-2020-8
Chen Y, Lian B, Peng L, Ding C, Lin Y, Yu L, Wang D, Kang D (2020) Neutrophil to lymphocyte ratio is a prognosis factor for post-operative pneumonia in aneurysmal subarachnoid hemorrhage patients. Chin Med J 134:682–689. https://doi.org/10.1097/cm9.0000000000001304
Zhang X, Zhang S, Wang C, Liu R, Li A (2022) High neutrophil-to-albumin ratio predicts postoperative pneumonia in aneurysmal subarachnoid hemorrhage. Front Neurol 13:840858. https://doi.org/10.3389/fneur.2022.840858
Ayling OGS, Ibrahim GM, Alotaibi NM (2018) Anemia after aneurysmal subarachnoid hemorrhage is associated with poor outcome and death. Stroke: A J Cereb Circ 49:1859–1865
Asare K (2008) Anemia of critical illness. Pharmacotherapy 28:1267–1282. https://doi.org/10.1592/phco.28.10.1267
Al-Mufti F, Amuluru K, Damodara N, Dodson V, Roh D, Agarwal S, Meyers PM, Connolly ES Jr, Schmidt MJ, Claassen J, Park S (2019) Admission neutrophil-lymphocyte ratio predicts delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. J Neurointerv Surg 11:1135–1140. https://doi.org/10.1136/neurintsurg-2019-014759
Al-Mufti F, Misiolek KA, Roh D, Alawi A, Bauerschmidt A, Park S, Agarwal S, Meyers PM, Connolly ES, Claassen J, Schmidt JM (2019) White blood cell count improves prediction of delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. Neurosurgery 84:397–403. https://doi.org/10.1093/neuros/nyy045
Behrouz R, Godoy DA, Topel CH, Birnbaum LA, Caron JL, Grandhi R, Johnson JN, Misra V, Seifi A, Urbansky K (2016) Early hypoalbuminemia is an independent predictor of mortality in aneurysmal subarachnoid hemorrhage. Neurocrit Care 25:1–7
Claassen J, Vu A, Kreiter KT, Kowalski RG, Du EY, Ostapkovich N, Fitzsimmons BF, Connolly ES, Mayer SA (2004) Effect of acute physiologic derangements on outcome after subarachnoid hemorrhage. Crit Care Med 32:832–838. https://doi.org/10.1097/01.ccm.0000114830.48833.8a
Baldwin ME, Macdonald RL, DRL Huo (2004) Early Vasospasm on admission angiography in patients with aneurysmal subarachnoid hemorrhage is a predictor for in-hospital complications and poor outcome. Stroke 35
Terao Y, Takada M, Tanabe T, Ando Y, Sumikawa K (2007) Microalbuminuria is a prognostic predictor in aneurysmal subarachnoid hemorrhage. Intensive Care Med 33:1000
Acknowledgements
We thank all the staff and participants for their contribution to this study.
Funding
This study was supported by the National Key Research and Development Program of China (Grant No. 2021YFC2501101 and 2020YFC2004701) and the National Natural Science Foundation of China (Grant No. 82071296, 81671129 and 81471210).
Author information
Authors and Affiliations
Contributions
Conception and design: Xiaolin Chen, Yuanli Zhao. Acquisition of data: Runting Li, Fa Lin, Yu Chen, Junlin Lu, Heze Han, Li Ma, Yahui Zhao, Debin Yan, Ruinan Li, Jun Yang, Shihao He, Zhipeng Li, Haibin Zhang, Kexin Yuan, Ke Wang, Hongliang Li, Linlin Zhang. Analysis and interpretation of data: All authors. Drafting the article: Runting Li. Reviewed submitted version of manuscript: Xiaolin Chen, Yuanli Zhao. Statistical analysis: Runting Li, Fa Lin, Yu Chen, Junlin Lu, Qiang Hao. Administrative/technical/material support: Youxiang Li, Shuo Wang, Guangzhi Shi, Jianxin Zhou. Study supervision: Xiaolin Chen, Yuanli Zhao.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the Institutional Review Board of Beijing Tiantan Hospital (KY 2021–008-01). All the analysis was performed according to the Declaration of Helsinki and the local ethics policies.
Consent to participate
Informed consent for clinical analysis was obtained from all individual participants or their authorized representatives.
Consent for publication
All authors read and approved the final manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, R., Lin, F., Chen, Y. et al. The effect of sex differences on complications and 90-day outcomes after aneurysmal subarachnoid hemorrhage: a propensity score-matched analysis. Neurosurg Rev 45, 3339–3347 (2022). https://doi.org/10.1007/s10143-022-01836-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-022-01836-x