Abstract
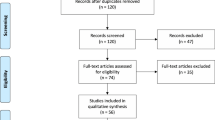
During lateral lumbar fusion, the trajectory of implant insertion approaches the great vessels anteriorly and the segmental arteries posteriorly, which carries the risk of vascular complications. We aimed to analyze vascular injuries for potential differences between oblique lateral interbody fusion (OLIF) and lateral lumbar interbody fusion (LLIF) procedures at our institution. This was coupled with a systematic literature review of vascular complications associated with lateral lumbar fusions. A retrospective chart review was completed to identify consecutive patients who underwent lateral access fusions. The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines were used for the systematic review with the search terms “vascular injury” and “lateral lumbar surgery.” Of 260 procedures performed at our institution, 211 (81.2%) patients underwent an LLIF and 49 (18.8%) underwent an OLIF. There were no major vascular complications in either group in this comparative study, but there were four (1.5%) minor vascular injuries (2 LLIF, 0.95%; 2 OLIF, 4.1%). Patients who experienced vascular injury experienced a greater amount of blood loss than those who did not (227.5 ± 147.28 vs. 59.32 ± 68.30 ml) (p = 0.11). In our systematic review of 63 articles, major vascular injury occurred in 0–15.4% and minor vascular injury occurred in 0–6% of lateral lumbar fusions. The systematic review and comparative study demonstrate an increased rate of vascular injury in OLIF when compared to LLIF. However, vascular injuries in either procedure are rare, and this study aids previous literature to support the safety of both approaches.


Similar content being viewed by others
Data availability
The results of this study are available upon request.
Code availability
Not applicable.
Abbreviations
- ASA:
-
American Society of Anesthesiology
- BMI:
-
Body mass index
- CCI:
-
Charlson Comorbidity Index
- DLIF:
-
Direct lateral interbody fusion
- EMG:
-
Electromyography
- LLIF:
-
Lateral lumbar interbody fusion
- min:
-
Minutes
- ml:
-
Milliliters
- OLIF:
-
Oblique lateral interbody fusion
- PRISMA:
-
Preferred Reporting Items for Systematic reviews and Meta-Analysis
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- XLIF:
-
Extreme lateral interbody fusion
References
Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, Kotani T, Akazawa T, Morinaga T, Fujiyoshi T, Hasue F, Yamagata M, Hashimoto M, Yamauchi T, Eguchi Y, Suzuki M, Hanaoka E, Inage K, Sato J, Fujimoto K, Shiga Y, Kanamoto H, Yamauchi K, Nakamura J, Suzuki T, Hynes RA, Aoki Y, Takahashi K, Ohtori S (2017) Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine (Phila Pa 1976) 42:55–62. https://doi.org/10.1097/brs.0000000000001650
Agarwal N, Faramand A, Alan N, Tempel ZJ, Hamilton DK, Okonkwo DO, Kanter AS (2018) Lateral lumbar interbody fusion in the elderly: a 10-year experience. J Neurosurg Spine 29:525–529. https://doi.org/10.3171/2018.3.Spine171147
Ahmadian A, Verma S, Mundis GM Jr, Oskouian RJ Jr, Smith DA, Uribe JS (2013) Minimally invasive lateral retroperitoneal transpsoas interbody fusion for L4–5 spondylolisthesis: clinical outcomes. J Neurosurg Spine 19:314–320. https://doi.org/10.3171/2013.6.Spine1340
Aichmair A, Fantini GA, Garvin S, Beckman J, Girardi FP (2015) Aortic perforation during lateral lumbar interbody fusion. J Spinal Disord Tech 28:71–75. https://doi.org/10.1097/bsd.0000000000000067
Alimi M, Hofstetter CP, Cong GT, Tsiouris AJ, James AR, Paulo D, Elowitz E, Härtl R (2014) Radiological and clinical outcomes following extreme lateral interbody fusion. J Neurosurg Spine 20:623–635. https://doi.org/10.3171/2014.1.Spine13569
Allison DW, Allen RT, Kohanchi DD, Skousen CB, Lee YP, Gertsch JH (2015) Vasculopathy, ischemia, and the lateral lumbar interbody fusion surgery: report of three cases. J Clin Neurophysiol 32:e41-45. https://doi.org/10.1097/wnp.0000000000000136
Anand N, Alayan A, Agrawal A, Kahwaty S, Nomoto E, Khandehroo B (2019) Analysis of spino-pelvic parameters and segmental lordosis with L5–S1 oblique lateral interbody fusion at the bottom of a long construct in circumferential minimally invasive surgical correction of adult spinal deformity. World Neurosurg 130:e1077–e1083. https://doi.org/10.1016/j.wneu.2019.07.091
Assina R, Majmundar NJ, Herschman Y, Heary RF (2014) First report of major vascular injury due to lateral transpsoas approach leading to fatality. J Neurosurg Spine 21:794–798. https://doi.org/10.3171/2014.7.Spine131146
Balsano M, Carlucci S, Ose M, Boriani L (2015) A case report of a rare complication of bowel perforation in extreme lateral interbody fusion. Eur Spine J 24(Suppl 3):405–408. https://doi.org/10.1007/s00586-015-3881-6
Bergey DL, Villavicencio AT, Goldstein T, Regan JJ (2004) Endoscopic lateral transpsoas approach to the lumbar spine. Spine (Phila Pa 1976) 29:1681–1688. https://doi.org/10.1097/01.brs.0000133643.75795.ef
Berry CA, Thawrani DP, Makhoul FR (2021) Inclusion of L5–S1 in oblique lumbar interbody fusion-techniques and early complications-a single center experience. Spine J 21:418–429. https://doi.org/10.1016/j.spinee.2020.10.016
Blizzard DJ, Gallizzi MA, Isaacs RE, Brown CR (2016) Renal artery injury during lateral transpsoas interbody fusion: case report. J Neurosurg Spine 25:464–466. https://doi.org/10.3171/2016.2.Spine15785
Buric J, Bombardieri D (2016) Direct lesion and repair of a common iliac vein during XLIF approach. Eur Spine J 25(Suppl 1):89–93. https://doi.org/10.1007/s00586-015-4134-4
Chang J, Kim JS, Jo H (2017) Ventral dural injury after oblique lumbar interbody fusion. World Neurosurg 98:881.e881-881.e884. https://doi.org/10.1016/j.wneu.2016.11.028
Cheng C, Wang K, Zhang C, Wu H, Jian F (2021) Clinical results and complications associated with oblique lumbar interbody fusion technique. Ann Transl Med 9:16. https://doi.org/10.21037/atm-20-2159
Chung NS, Jeon CH, Lee HD (2018) Use of an alternative surgical corridor in oblique lateral interbody fusion at the L5–S1 segment: a technical report. Clin Spine Surg 31:293–296. https://doi.org/10.1097/bsd.0000000000000584
Chung NS, Jeon CH, Lee HD, Kweon HJ (2017) Preoperative evaluation of left common iliac vein in oblique lateral interbody fusion at L5–S1. Eur Spine J 26:2797–2803. https://doi.org/10.1007/s00586-017-5176-6
Chung NS, Lee HD, Jeon CH (2021) Vascular anatomy and surgical approach in oblique lateral interbody fusion at lumbosacral transitional vertebrae. J Orthop Sci 26:358–362. https://doi.org/10.1016/j.jos.2020.04.008
Cui JM, Wang JR, Zheng ZM, Liu H, Wang H, Li ZM (2021) Lateral-anterior lumbar interbody fusion (LaLIF) for lumbar degenerative disease: technical notes, surgical system, and mid-term outcomes. J Orthop Translat 28:12–20. https://doi.org/10.1016/j.jot.2020.12.001
Dakwar E, Cardona RF, Smith DA, Uribe JS (2010) Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus 28:E8. https://doi.org/10.3171/2010.1.Focus09282
DiGiorgio AM, Edwards CS, Virk MS, Mummaneni PV, Chou D (2017) Stereotactic navigation for the prepsoas oblique lateral lumbar interbody fusion: technical note and case series. Neurosurg Focus 43:E14. https://doi.org/10.3171/2017.5.Focus17168
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384. https://doi.org/10.1136/jech.52.6.377
Epstein NE (2016) Extreme lateral lumbar interbody fusion: Do the cons outweigh the pros? Surg Neurol Int 7:S692–S700. https://doi.org/10.4103/2152-7806.191079
Formica M, Berjano P, Cavagnaro L, Zanirato A, Piazzolla A, Formica C (2014) Extreme lateral approach to the spine in degenerative and post traumatic lumbar diseases: selection process, results and complications. Eur Spine J 23(Suppl 6):684–692. https://doi.org/10.1007/s00586-014-3545-y
Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, Nagashima H, Nakamura M, Sairyo K, Takemasa R, Iwasaki M (2017) Complications associated with lateral interbody fusion: nationwide survey of 2998 cases during the first 2 years of its use in Japan. Spine (Phila Pa 1976) 42:1478–1484. https://doi.org/10.1097/brs.0000000000002139
Gragnaniello C, Seex K (2016) Anterior to psoas (ATP) fusion of the lumbar spine: evolution of a technique facilitated by changes in equipment. J Spine Surg 2:256–265. https://doi.org/10.21037/jss.2016.11.02
Grimm BD, Leas DP, Poletti SC, Johnson DR 2nd (2016) Postoperative complications within the first year after extreme lateral interbody fusion: experience of the first 108 patients. Clin Spine Surg 29:E151-156. https://doi.org/10.1097/bsd.0000000000000121
Hah R, Kang HP (2019) Lateral and oblique lumbar interbody fusion—current concepts and a review of recent literature. Curr Rev Musculoskelet Med 12:305–310. https://doi.org/10.1007/s12178-019-09562-6
Hu ZJ, Fang XQ, Zhao FD, Zhang JF, Zhao X, Fan SW (2021) Anteroinferior psoas technique for oblique lateral lumbar interbody fusion: technical note and case series. Orthop Surg 13:466–473. https://doi.org/10.1111/os.12890
Isaacs RE, Hyde J, Goodrich JA, Rodgers WB, Phillips FM (2010) A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976) 35:S322-330
Isaacs RE, Sembrano JN, Tohmeh AG (2016) Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: Part II: Radiographic findings. Spine (Phila Pa 1976) 41(Supp 8):S133-144. https://doi.org/10.1097/brs.0000000000001472
Jin C, Jaiswal MS, Jeun SS, Ryu KS, Hur JW, Kim JS (2018) Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J Orthop Surg Res 13:38. https://doi.org/10.1186/s13018-018-0740-2
Krieg SM, Bobinski L, Albers L, Meyer B (2019) Lateral lumbar interbody fusion without intraoperative neuromonitoring: a single-center consecutive series of 157 surgeries. J Neurosurg Spine:1–7. https://doi.org/10.3171/2018.9.Spine18588
Kueper J, Fantini GA, Walker BR, Aichmair A, Hughes AP (2015) Incidence of vascular complications during lateral lumbar interbody fusion: an examination of the mini-open access technique. Eur Spine J 24:800–809. https://doi.org/10.1007/s00586-015-3796-2
Lee CW, Yoon KJ, Ha SS (2017) Which approach is advantageous to preventing development of adjacent segment disease? Comparative analysis of 3 different lumbar interbody fusion techniques (ALIF, LLIF, and PLIF) in L4–5 spondylolisthesis. World Neurosurg 105:612–622. https://doi.org/10.1016/j.wneu.2017.06.005
Li HM, Zhang RJ, Shen CL (2019) Differences in radiographic and clinical outcomes of oblique lateral interbody fusion and lateral lumbar interbody fusion for degenerative lumbar disease: a meta-analysis. BMC Musculoskelet Disord 20:582. https://doi.org/10.1186/s12891-019-2972-7
Li J, Wang X, Sun Y, Zhang F, Gao Y, Li Z, Ding W, Shen Y, Zhang W (2019) Safety analysis of two anterior lateral lumbar interbody fusions at the initial stage of learning curve. World Neurosurg 127:e901–e909. https://doi.org/10.1016/j.wneu.2019.03.294
Liu C, Zhai J, Yuan Q, Zhang Y, Xu H (2020) A patient with left-sided inferior vena cava who received oblique lumbar interbody fusion surgery: a case report. J Med Case Rep 14:21. https://doi.org/10.1186/s13256-020-2342-y
Liu J, Feng H (2020) Oblique Lateral interbody fusion (OLIF) with supplemental anterolateral screw and rod instrumentation: a preliminary clinical study. World Neurosurg 134:e944–e950. https://doi.org/10.1016/j.wneu.2019.11.046
Malham GM, Parker RM, Blecher CM, Chow FY, Seex KA (2016) Choice of approach does not affect clinical and radiologic outcomes: a comparative cohort of patients having anterior lumbar interbody fusion and patients having lateral lumbar interbody fusion at 24 months. Global Spine J 6:472–481. https://doi.org/10.1055/s-0035-1569055
Manning J, Wang E, Varlotta C, Woo D, Ayres E, Eisen L, Bendo J, Goldstein J, Spivak J, Protopsaltis TS, Passias PG, Buckland AJ (2020) The effect of vascular approach surgeons on perioperative complications in lateral transpsoas lumbar interbody fusions. Spine J 20:313–320. https://doi.org/10.1016/j.spinee.2019.10.013
Mayer HM (1997) A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976) 22:691–699; discussion 700. https://doi.org/10.1097/00007632-199703150-00023
Mehren C, Mayer HM, Zandanell C, Siepe CJ, Korge A (2016) The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res 474:2020–2027. https://doi.org/10.1007/s11999-016-4883-3
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. Journal of spine surgery (Hong Kong) 1:2–18. https://doi.org/10.3978/j.issn.2414-469X.2015.10.05
Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Aoki Y, Nakamura J, Ishikawa T, Miyagi M, Kamoda H, Suzuki M, Kubota G, Sakuma Y, Oikawa Y, Inage K, Sainoh T, Sato J, Fujimoto K, Shiga Y, Abe K, Toyone T, Inoue G, Takahashi K (2015) Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J 56:1051–1059. https://doi.org/10.3349/ymj.2015.56.4.1051
Ozgur BM, Agarwal V, Nail E, Pimenta L (2010) Two-year clinical and radiographic success of minimally invasive lateral transpsoas approach for the treatment of degenerative lumbar conditions. Sas j 4:41–46. https://doi.org/10.1016/j.esas.2010.03.005
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 10:89. https://doi.org/10.1186/s13643-021-01626-4
Rentenberger C, Shue J, Soffin EM, Stiles BM, Craig CM, Hughes AP (2019) Intercostal artery hemorrhage with hemothorax following combined lateral and posterior lumbar interbody fusion: a case report. Spinal Cord Ser Cases 5:60. https://doi.org/10.1038/s41394-019-0205-9
Rodgers WB, Gerber EJ, Patterson J (2011) Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa 1976) 36:26–32. https://doi.org/10.1097/BRS.0b013e3181e1040a
Safaee MM, Zarkowsky D, Eichler CM, Pekmezci M, Clark AJ (2018) Management of aortic injury during minimally invasive lateral lumbar interbody fusion. Eur Spine J 27:538–543. https://doi.org/10.1007/s00586-018-5620-2
Salzmann SN, Shue J, Hughes AP (2017) Lateral lumbar interbody fusion-outcomes and complications. Curr Rev Musculoskelet Med 10:539–546. https://doi.org/10.1007/s12178-017-9444-1
Santillan A, Patsalides A, Gobin YP (2010) Endovascular embolization of iatrogenic lumbar artery pseudoaneurysm following extreme lateral interbody fusion (XLIF). Vasc Endovascular Surg 44:601–603. https://doi.org/10.1177/1538574410374655
Saraph V, Lerch C, Walochnik N, Bach CM, Krismer M, Wimmer C (2004) Comparison of conventional versus minimally invasive extraperitoneal approach for anterior lumbar interbody fusion. Eur Spine J 13:425–431. https://doi.org/10.1007/s00586-004-0722-4
Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kuniyoshi K, Aoki Y, Nakamura J, Miyagi M, Suzuki M, Kubota G, Inage K, Sainoh T, Fujimoto K, Shiga Y, Abe K, Kanamoto H, Inoue G, Takahashi K (2017) Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J 26:671–678. https://doi.org/10.1007/s00586-015-4170-0
Sellin JN, Brusko GD, Levi AD (2019) Lateral lumbar interbody fusion revisited: complication avoidance and outcomes with the mini-open approach. World Neurosurg 121:e647–e653. https://doi.org/10.1016/j.wneu.2018.09.180
Shimizu T, Fujibayashi S, Otsuki B, Murata K, Matsuda S (2020) Indirect decompression through oblique lateral interbody fusion for revision surgery after lumbar decompression. World Neurosurg 141:e389–e399. https://doi.org/10.1016/j.wneu.2020.05.151
Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P (2012) Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J 6:89–97. https://doi.org/10.4184/asj.2012.6.2.89
Sofianos DA, Briseño MR, Abrams J, Patel AA (2012) Complications of the lateral transpsoas approach for lumbar interbody arthrodesis: a case series and literature review. Clin Orthop Relat Res 470:1621–1632. https://doi.org/10.1007/s11999-011-2088-3
Spiessberger A, Arvind V, Dietz N, Grueter B, Huber F, Guggenberger R, Moriggl B, Varma V, Cho SK (2020) A comparison of complications and clinical and radiologic outcome between the mini-open prepsoas and mini-open transpsoas approaches for lumbar interbody fusion: a meta-analysis. Clin Spine Surg 33:271–279. https://doi.org/10.1097/bsd.0000000000001015
Tannoury T, Kempegowda H, Haddadi K, Tannoury C (2019) Complications associated with minimally invasive anterior to the psoas (ATP) fusion of the lumbosacral spine. Spine (Phila Pa 1976) 44:E1122-e1129. https://doi.org/10.1097/brs.0000000000003071
Taterra D, Skinningsrud B, Pękala PA, Hsieh WC, Cirocchi R, Walocha JA, Tubbs RS, Tomaszewski KA, Henry BM (2019) Artery of Adamkiewicz: a meta-analysis of anatomical characteristics. Neuroradiology 61:869–880. https://doi.org/10.1007/s00234-019-02207-y
Tessitore E, Molliqaj G, Schaller K, Gautschi OP (2017) Extreme lateral interbody fusion (XLIF): a single-center clinical and radiological follow-up study of 20 patients. J Clin Neurosci 36:76–79. https://doi.org/10.1016/j.jocn.2016.10.001
Tong YJ, Liu JH, Fan SW, Zhao FD (2019) One-stage debridement via oblique lateral interbody fusion corridor combined with posterior pedicle screw fixation in treating spontaneous lumbar infectious spondylodiscitis: a case series. Orthop Surg 11:1109–1119. https://doi.org/10.1111/os.12562
Vaishnav AS, Othman YA, Virk SS, Gang CH, Qureshi SA (2019) Current state of minimally invasive spine surgery. J Spine Surg 5:S2-s10. https://doi.org/10.21037/jss.2019.05.02
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335:806–808. https://doi.org/10.1136/bmj.39335.541782.AD
Waddell B, Briski D, Qadir R, Godoy G, Houston AH, Rudman E, Zavatsky J (2014) Lateral lumbar interbody fusion for the correction of spondylolisthesis and adult degenerative scoliosis in high-risk patients: early radiographic results and complications. Ochsner J 14:23–31
Walker CT, Farber SH, Cole TS, Xu DS, Godzik J, Whiting AC, Hartman C, Porter RW, Turner JD, Uribe J (2019) Complications for minimally invasive lateral interbody arthrodesis: a systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J Neurosurg Spine:1–15. https://doi.org/10.3171/2018.9.Spine18800
Wang MY, Vasudevan R, Mindea SA (2014) Minimally invasive lateral interbody fusion for the treatment of rostral adjacent-segment lumbar degenerative stenosis without supplemental pedicle screw fixation. J Neurosurg Spine 21:861–866. https://doi.org/10.3171/2014.8.Spine13841
Woods K, Fonseca A, Miller LE (2017) Two-year outcomes from a single surgeon’s learning curve experience of oblique lateral interbody fusion without intraoperative neuromonitoring. Cureus 9:e1980. https://doi.org/10.7759/cureus.1980
Woods KR, Billys JB, Hynes RA (2017) Technical description of oblique lateral interbody fusion at L1–L5 (OLIF25) and at L5–S1 (OLIF51) and evaluation of complication and fusion rates. Spine J 17:545–553. https://doi.org/10.1016/j.spinee.2016.10.026
Xi Z, Chou D, Mummaneni PV, Burch S (2020) The navigated oblique lumbar interbody fusion: accuracy rate, effect on surgical time, and complications. Neurospine 17:260–267. https://doi.org/10.14245/ns.1938358.179
Zeng ZY, Xu ZW, He DW, Zhao X, Ma WH, Ni WF, Song YX, Zhang JQ, Yu W, Fang XQ, Zhou ZJ, Xu NJ, Huang WJ, Hu ZC, Wu AL, Ji JF, Han JF, Fan SW, Zhao FD, Jin H, Pei F, Fan SY, Sui DX (2018) Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg 10:98–106. https://doi.org/10.1111/os.12380
Zhang YH, White I, Potts E, Mobasser JP, Chou D (2017) Comparison perioperative factors during minimally invasive pre-psoas lateral interbody fusion of the lumbar spine using either navigation or conventional fluoroscopy. Global Spine J 7:657–663. https://doi.org/10.1177/2192568217716149
Zhengkuan X, Qixin C, Gang C, Fangcai L (2019) The technical note and approach related complications of modified lateral lumbar interbody fusion. J Clin Neurosci 66:182–186. https://doi.org/10.1016/j.jocn.2019.04.019
Acknowledgements
We thank Ryley Herren for preparing the anatomical illustration and Debra J. Zimmer for editorial support.
Author information
Authors and Affiliations
Contributions
Conception and design: Pollina, Aguirre, Soliman.
Acquisition of data: Aguirre, Azmy
Interpretation of data: all authors
Drafting the manuscript: Aguirre, Soliman
Critically revising the manuscript: all Authors
Reviewed submitted version of manuscript: all Authors
Statistical analysis: Aguirre
Study supervision: Pollina
Corresponding author
Ethics declarations
Ethics approval
University at Buffalo Institutional Review Board STUDY00005744.
Consent to participate
Consent was obtained from patients or a legally authorized representative before procedures were performed.
Consent for publication
At the time of hospital admission, informed consent for patient information to be published was provided by each patient or a legally authorized representative.
Conflict of interest
Dr. Khan received a research grant from the Scoliosis Research Society to study scoliosis in Chiari patients. Dr. Mullin receives research funding from AOSpine North America (AOSNA) and the Research Committee Award #87639; and from Medtronic External Research Program Health Professionals, ERP ID#2020–12271. Dr. Pollina is involved with surgical training for Medtronic, and he serves as a consultant for and receives royalties from ATEC Spine. All other authors have no personal, financial, or institutional interest in the materials or devices described in this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aguirre, A.O., Soliman, M.A.R., Azmy, S. et al. Incidence of major and minor vascular injuries during lateral access lumbar interbody fusion procedures: a retrospective comparative study and systematic literature review. Neurosurg Rev 45, 1275–1289 (2022). https://doi.org/10.1007/s10143-021-01699-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01699-8