Abstract
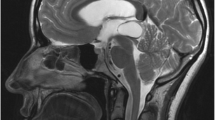
In this short review, the authors performed a database search and summarize current knowledge of the management of patients with pineal cysts (PCs) and investigate the role of surgical treatment. The scientific literature on the surgical treatment of PCs is sparse and encompasses only case series with little over 200 operated patients combined. All included papers reported favorable results after pineal cyst surgery with improvement of symptoms in most patients. Microsurgical resection of PCs, preferably using the supracerebellar-infratentorial approach, could be considered as a viable treatment option in symptomatic patients. Even patients with non-specific symptoms are reported to improve after surgery. However, evidence offered by this literature review is very limited and therefore our conclusions must be tempered by the restricted set of data. For ethical reasons, a randomized controlled trial is not an acceptable approach, and therefore patient registry could be a useful tool to identify a subset of symptomatic patients that might benefit from pineal cyst resection.


Similar content being viewed by others
References
Aliaga L, Hekman KE, Yassari R, Straus D, Luther G, Chen J, Sampat A, Frim D (2012) A novel scoring system for assessing Chiari malformation type I treatment outcomes. Neurosurgery 70(3):656–665
Barboriak DP, Lee L, Provenzale JM (2001) Serial MR imaging of pineal cysts: implications for natural history and follow-up. AJR Am J Roentgenol 176(3):737–743
Berhouma M, Ni H, Delabar V, Tahhan N, Memou Salem S, Mottolese C, Vallee B (2015) Update on the management of pineal cysts: case series and a review of the literature. Neurochirurgie 61(2–3):201–207
Eide PK, Pripp AH, Ringstad GA (2016) Magnetic resonance imaging biomarkers indicate a central venous hypertension syndrome in patients with symptomatic pineal cysts. J Neurol Sci 363:207–216
Eide PK, Ringstad G (2016) Increased pulsatile intracranial pressure in patients with symptomatic pineal cysts and magnetic resonance imaging biomarkers indicative of central venous hypertension. J Neurol Sci 367:247–255
Eide PK, Ringstad G (2017) Results of surgery in symptomatic non-hydrocephalic pineal cysts: role of magnetic resonance imaging biomarkers indicative of central venous hypertension. Acta Neurochir 159(2):349–361
Fain JS, Tomlinson FH, Scheithauer BW, Parisi JE, Fletcher GP, Kelly PJ, Miller GM (1994) Symptomatic glial cysts of the pineal gland. J Neurosurg 80(3):454–460
Fetell MR, Bruce JN, Burke AM, Cross DT, Torres RA, Powers JM, Stein BM (1991) Non-neoplastic pineal cysts. Neurology 41(7):1034–1040
Hajnsek S, Paladino J, Gadze ZP, Nanković S, Mrak G, Lupret V (2013) Clinical and neurophysiological changes in patients with pineal region expansions. Coll Antropol 37(1):35–40
Kalani M, Wilson D, Koechlin N, Abuhusain H, Dlouhy B, Gunawardena M, Nozue-Okada K, Teo C (2015) Pineal cyst resection in the absence of ventriculomegaly or Parinaud’s syndrome: clincial outcomes and implications for patient selection. J Neurosurg 123(2):352–356
Kreth FW, Schätz CR, Pagenstecher A, Faist M, Volk B, Ostertag CB (1996) Stereotactic management of lesions of the pineal region. Neurosurgery 39(2):280–289 91
Kulkarni AV (2015) Editorial: pineal cyst resection. J Neurosurg 123(2):350–351
Májovský M, Netuka D, Beneš V (2016) Clinical management of pineal cysts: a worldwide online survey. Acta Neurochir 158(4):663–669
Májovský M, Netuka D, Beneš V (2017) Conservative and surgical treatment of patients with pineal cysts: a prospective case series of 110 patients. World Neurosurg. doi:10.1016/j.wneu.2017.05.155
Májovský M, Řezáčová L, Sumová A, Pospíšilová L, Netuka D, Bradáč O, Beneš V (2017) Melatonin and cortisol secretion profile in patients with pineal cyst before and after pineal cyst resection. J Clin Neurosci 39:155–163
Márquez J, Rivero M (2011) Pineal cysts. J Neurosurg Pediatr 8(4):422–422
Mena H, Armonda RA, Ribas JL, Ondra SL, Rushing EJ (1997) Nonneoplastic pineal cysts: a clinicopathologic study of twenty-one cases. Ann Diagn Pathol 1(1):11–18
Pussep L (1914) Die operative Entfernung einer Zyste der Glandula pinealis. Neurol Zentralbl 33:560–563
Qi S, Fan J, Zhang X, Zhang H, Qiu B, Fang L (2014) Radical resection of nongerminomatous pineal region tumors via the occipital transtentorial approach based on arachnoidal consideration: experience on a series of 143 patients. Acta Neurochir 156(12):2253–2262
Seifert CL, Woeller A, Valet M, Zimmer C, Berthele A, Tölle T, Sprenger T (2008) Headaches and pineal cyst: a case-control study. Headache 48(3):448–452
Starke RM, Cappuzzo JM, Erickson NJ, Sherman JH (2016) Pineal cysts and other pineal region malignancies: determining factors predictive of hydrocephalus and malignancy. J Neurosurg 1–6
Tirakotai W, Schulte DM, Bauer BL, Bertalanffy H, Hellwig D (2004) Neuroendoscopic surgery of intracranial cysts in adults. Childs Nerv Syst 20(11–12):842–851
Yoshimoto K, Araki Y, Amano T, Matsumoto K, Nakamizo A, Sasaki T et al (2013) Clinical features and pathophysiological mechanism of the hemianoptic complication after the occipital transtentorial approach. Clin Neurol Neurosurg 115(8):1250–1256
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by grant no. MO 1012NK funded by the Ministry of Defense of the Czech Republic, grant no. 15-32791A funded by the Ministry of Health of the Czech Republic and grant no. Q25/LF1/2 funded by Charles University. The sponsors had no role in the design or conduct of this research.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Májovský, M., Netuka, D. & Beneš, V. Is surgery for pineal cysts safe and effective? Short review. Neurosurg Rev 41, 119–124 (2018). https://doi.org/10.1007/s10143-017-0876-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-017-0876-2