Abstract
Background
Recently, it has been reported that anorectal malformation with rectourethral fistula in male neonates can be managed by primary neonatal reconstruction without colostomy. To prevent urethral injury during anorectoplasty, the fistula’s location is important. To date, the use of voiding cystourethrograms to determine the presence and location of fistulas in neonates with anorectal malformations has not been studied.
Objective
To compare the accuracy of ultrasound (US) and voiding cystourethrogram for determining the presence and location of fistulas in neonates with anorectal malformation.
Materials and methods
We included 21 male neonates with anorectal malformation with rectourethral fistula (n=16), rectovesical fistula (n=1) or no fistula (n=4) who underwent US and voiding cystourethrogram preoperatively on the day of surgery. Fistula imaging was classified into three grades (0–2), and grades 1–2 were considered fistula positive. We compared the imaging-based location of the fistula with surgical findings.
Results
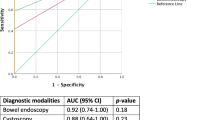
US performed significantly better than voiding cystourethrogram for determining the presence of fistulas (area under the receiver operating characteristic curve, 0.90 vs. 0.71, respectively; P=0.044) (diagnostic accuracy 85.7%, 95% confidence interval [95% CI] 63.7–97.0% and 52.4%, 95% CI 29.8–74.3%, respectively). In cases with fistulas detected by either modality, the accuracy of locating the fistula by US was 50.0% (95% CI 24.7–75.3%) and by voiding cystourethrogram was 100% (95% CI: 59.0–100%).
Conclusion
US accurately detected, but did not accurately locate, fistulas in neonates with anorectal malformation. When planning primary neonatal reconstruction of anorectal malformation without colostomy, voiding cystourethrogram could provide additional information about fistula location.





Similar content being viewed by others
References
Pena A (1993) Management of anorectal malformations during the newborn period. World J Surg 17:385–392
Santulli TV, Kiesewetter WB, Bill AH Jr et al (1970) Anorectal anomalies: a suggested international classification. J Pediatr Surg 5:281–287
Holschneider A, Hutson J, Pena A et al (2005) Preliminary report on the international conference for the development of standards for the treatment of anorectal malformations. J Pediatr Surg 40:1521–1526
van der Steeg HJ, Schmiedeke E, Bagolan P et al (2015) European consensus meeting of ARM-net members concerning diagnosis and early management of newborns with anorectal malformations. Tech Coloproctol 19:181–185
Adeniran JO, Abdur-Rahman L (2005) One-stage correction of intermediate imperforate anus in males. Pediatr Surg Int 21:88–90
Albanese CT, Jennings RW, Lopoo JB et al (1999) One-stage correction of high imperforate anus in the male neonate. J Pediatr Surg 34:834–836
Amanollahi O, Ketabchian S (2016) One-stage vs. three-stage repair in anorectal malformation with rectovestibular fistula. Afr J Paediatr Surg 13:20–25
Liu G, Yuan J, Geng J et al (2004) The treatment of high and intermediate anorectal malformations: one stage or three procedures? J Pediatr Surg 39:1466–1471
Menon P, Rao KLN, Sinha AK et al (2017) Anorectal malformations in males: pros and cons of neonatal versus staged reconstruction for high and intermediate varieties. J Indian Assoc Pediatr Surg 22:83–86
Abdalla WMA, De La Torre L (2017) The high pressure distal colostogram in anorectal malformations: technique and pitfalls. J Pediatr Surg 52:1207–1209
Kraus SJ, Levitt MA, Pena A et al (2018) Augmented-pressure distal colostogram: the most important diagnostic tool for planning definitive surgical repair of anorectal malformations in boys. Pediatr Radiol 48:258–269
Tainaka T, Uchida H, Tanaka Y et al (2018) Long-term outcomes and complications after laparoscopic-assisted anorectoplasty vs. posterior sagittal anorectoplasty for high- and intermediate-type anorectal malformation. Pediatr Surg Int 34:1111–1115
Xiao H, Huang R, Chen L et al (2018b) The midterm outcomes of 1-stage versus 3-stage laparoscopic-assisted anorectoplasty in anorectal malformations with rectoprostatic fistula and rectobulbar fistula: a retrospective cohort study. Medicine (Baltimore) 97:e11843
Xiao H, Chen L, Ren XH et al (2018a) One-stage laparoscopic-assisted anorectoplasty for neonates with anorectal malformation and recto-prostatic or recto-bulbar fistula according to the Krickenbeck classification. J Laparoendosc Adv Surg Tech A Part A 28:1029–1034
Alam S, Lawal TA, Pena A et al (2011) Acquired posterior urethral diverticulum following surgery for anorectal malformations. J Pediatr Surg 46:1231–1235
Japanese multicenter study group on male high imperforate anus (2013) Multicenter retrospective comparative study of laparoscopically assisted and conventional anorectoplasty for male infants with rectoprostatic urethral fistula. J Pediatr Surg 48:2383–2388
Hong AR, Acuna MF, Pena A et al (2002) Urologic injuries associated with repair of anorectal malformations in male patients. J Pediatr Surg 37:339–344
De Vos C, Arnold M, Sidler D, Moore SW (2011) A comparison of laparoscopic-assisted (LAARP) and posterior sagittal (PSARP) anorectoplasty in the outcome of intermediate and high anorectal malformations. S Afr J Surg 49:39–43
Islam MN, Hasina K, Reza MS et al (2015) Urinary tract anomalies in patients with anorectal malformation. Mymensingh Med J 24:352–355
Sanchez S, Ricca R, Joyner B, Waldhausen JH (2014) Vesicoureteral reflux and febrile urinary tract infections in anorectal malformations: a retrospective review. J Pediatr Surg 49:91–94
Hosokawa T, Yamada Y, Tanami Y et al (2017c) Sonography for an imperforate anus: approach, timing of the examination, and evaluation of the type of imperforate anus and associated anomalies. J Ultrasound Med 36:1747–1758
Alexander M, Holschneider JMH (2006) Anorectal malformation in children. Springer-Verlag, Berlin Heidelberg, pp 189–200
Hosokawa T, Yamada Y, Tanami Y et al (2017d) Diagnostic accuracy of sonography for detection of a fistula on the birth day in neonates with an imperforate anus: comparison of diagnostic performance between suprapubic and perineal approaches. J Ultrasound Med 36:1989–1995
Hosokawa T, Yamada Y, Sato Y et al (2017b) Changes in the distance between the distal rectal pouch and perineum from the birth day to the next day in neonates with an imperforate anus. J Ultrasound Med 36:601–606
Hosokawa T, Yamada Y, Hsokawa M et al (2018c) Ultrasound imaging of the anorectal malformation during the neonatal period: a comprehensive review. Jpn J Radiol 36:581–591
Hosokawa T, Takahashi H, Tanami Y et al (2018b) Comparison between the pouch-perineum distance in neonates with a low-type anorectal malformation with and without an opened fistula: pitfall of measuring the pouch-perineum distance on sonography. J Ultrasound Med. https://doi.org/10.1002/jum.14636
Hosokawa T, Hosokawa M, Tanami Y et al (2018a) Distance between the distal rectal pouch and perineum in neonates of low-birth weight with imperforate anus. Ultrasound Q 34:18–22
Hosokawa T, Hosokawa M, Tanami Y et al (2017a) Comparison of diagnostic accuracy for the low-type imperforate anus between prone cross-table radiography and sonography. J Ultrasound Med 36:1679–1686
Han TI, Kim IO, Kim WS et al (2003) Imperforate anus: US determination of the type with infracoccygeal approach. Radiology 228:226–229
Donaldson JS, Black CT, Reynolds M et al (1989) Ultrasound of the distal pouch in infants with imperforate anus. J Pediatr Surg 24:465–468
Teele RL, Share JC (1997) Transperineal sonography in children. AJR Am J Roentgenol 168:1263–1267
Fernbach SK, Feinstein KA, Schmidt MB et al (2000) Pediatric voiding cystourethrography: a pictorial guide. Radiographics 20:155–171
Ditchfield MR, Grattan-Smith JD, de Campo JF, Hutson JM (1995) Voiding cystourethrography in boys: does the presence of the catheter obscure the diagnosis of posterior urethral valves? AJR Am J Roentgenol 164:1233–1235
Duran C, Valera A, Alguersuari A et al (2009) Voiding urosonography: the study of the urethra is no longer a limitation of the technique. Pediatr Radiol 39:124–131
Sussman RD, Hill FC, Koch GE et al (2017) Novel pericatheter retrograde urethrogram technique is a viable method for postoperative urethroplasty imaging. Int Urol Nephrol 49:2157–2165
Duran C, Beltran VP, Gonzalez A et al (2017) Contrast-enhanced voiding urosonography for vesicoureteral reflux diagnosis in children. Radiographics 37:1854–1869
Giordano M, Marzolla R, Puteo F et al (2007) Voiding urosonography as first step in the diagnosis of vesicoureteral reflux in children: a clinical experience. Pediatr Radiol 37:674–677
Kljucevsek D, Battelino N, Tomazic M, Kersnik Levart T (2012) A comparison of echo-enhanced voiding urosonography with X-ray voiding cystourethrography in the first year of life. Acta Paediatr 101:e235–e239
Sekhon V, Kudchadkar SJ, Raj A, Ansari MS (2017) Radiographic gapometry score: a simple predictor for surgical approach in pediatric traumatic posterior urethral strictures. J Pediatr Urol 13:624
Papadopoulou F, Efremidis SC, Oiconomou A et al (2002) Cyclic voiding cystourethrography: is vesicoureteral reflux missed with standard voiding cystourethrography? Eur Radiol 12:666–670
Rollins MD, Downey EC, Meyers RL, Scaife ER (2009) Division of the fistula in laparoscopic-assisted repair of anorectal malformations-are clips or ties necessary? J Pediatr Surg 44:298–301
Bansal A, Kumar M, Goel S, Aeron R (2016) Urethro-venous intravasation: a rare complication of retrograde urethrogram. BMJ Case Rep. https://doi.org/10.1136/bcr-2016-215206
Malhotra NR, Green JR, Rigsby CK et al (2017) Urinary tract infection after retrograde urethrogram in children: a multicenter study. J Pediatr Urol 13:623.e1–623.e5
Kim IO, Han TI, Kim WS, Yeon KM (2000) Transperineal ultrasonography in imperforate anus: identification of the internal fistula. J Ultrasound Med 19:211–216
Choi YH, Kim IO, Cheon JE et al (2009) Imperforate anus: determination of type using transperineal ultrasonography. Korean J Radiol 10:355–360
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hosokawa, T., Yamada, Y., Tanami, Y. et al. Comparison of diagnostic accuracy for fistulae at ultrasound and voiding cystourethrogram in neonates with anorectal malformation. Pediatr Radiol 49, 609–616 (2019). https://doi.org/10.1007/s00247-018-04339-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-04339-4