Abstract
Background
Frailty aggregates a composite of geriatric and elderly features that is classified into a singular syndrome; literature thus far has proven its influence over postoperative outcomes. In this study, we evaluate the effects of frailty following gastrectomy for gastric cancer.
Methods
2011–2017 National Inpatient Sample was used to isolate patients with gastric cancer undergoing gastrectomy; from this, the Johns Hopkins ACG frailty criteria were applied to segregate frailty-present and absent populations. The case–controls were matched using propensity-score matching and compared to various endpoints.
Results
Post match, there were 1171 with and without frailty who were undergoing gastrectomy for gastric cancer. Those with frailty had higher mortality (6.83 vs 3.50% p < 0.001, OR 2.02 95% CI 1.37–2.97), length of stay (16.7 vs 12.0d; p < 0.001), and costs ($191,418 vs $131,367; p < 0.001); frail patients also had higher rates of complications including wound complications (3.42 vs 0.94% p < 0.001, OR 3.73 95% CI 1.90–7.31), infection (5.98 vs 3.67% p = 0.012, OR 1.67 95% CI 1.13–2.46), and respiratory failure (6.32 vs 3.84% p = 0.0084, OR 1.69 95% CI 1.15–2.47). In multivariate, those with frailty had higher mortality (p < 0.001, aOR 2.04 95% CI 1.38–3.01), length of stay (p < 0.001, aOR 1.40 95% CI 1.37–1.43), and costs (p < 0.001, aOR 1.46 95% CI 1.46–1.46).
Conclusion
This study finding demonstrates the presence of frailty is an independent risk factor of adverse outcomes following gastrectomy; as such, it is important that these high-risk patients are stratified preoperatively and provided risk-averting procedures to alleviate their frailty-defining features.
Similar content being viewed by others
Introduction
Elderly patients can develop clinical frailty due to the composite presence of geriatric and medical conditions that multi-modally affect different domains of functions, dependence, ambulation, and medical/clinical performance [1]. Essentially, frailty combines conditions of malnutrition, physiological aberrations in metabolism, feeding difficulties, and fecal and urinary incontinence with deficiencies in the socioeconomic sphere, including low-income status, housing difficulties and social isolation [1, 2] to describe a clinical phenotype that is prone to increasingly adverse effects following surgeries and medical interventions [3]. The Johns Hopkins Adjusted Clinical Groups (ACG) definition of frailty is based on the consideration of 10 diagnostic clusters, which are listed in Supplementary Tables 1 and 4. This definition of frailty is particularly applicable in patients that require gastric surgery for gastric tumors [5, 6], as these patients are often elderly or have underlying feeding and nutritional difficulties that predispose them to frailty-development [7, 8]. However, frailty is not only restricted to elderly patients but can also be manifested in younger patients with malignancy, which induces conditions overlapping with frailty-defining features that range from nutritional deficiencies to social maladjustments. Prior NIS studies have also used Johns Hopkins ACG frailty criteria to define frailty in patients with malignancy undergoing resective procedures.
In surgical literature, it is currently well known that the underlying presence of frailty imposes a significant degree of risk in postoperative outcomes following various surgical procedures [4]. However, while the effects of frailty have been alluded to in multiple studies, its effects on post-gastrectomy remain undefined due to the sparsity of studies. Thus, in light of this, we plan to systematically evaluate the postoperative effects of frailty on gastrectomy outcomes in patients with gastric malignancy; to accomplish this, we use a national registry of hospital data and propensity-score matching to evaluate the respective risks associated with frailty on post-gastrectomy outcomes.
Methods
NIS database and variable selection
This study uses 2011–2017 data from the National Inpatient Sample (NIS), an annually updated database pertaining up to 40 ICD diagnoses and 25 ICD-10 PCS codes per patient, such as demographics, admission, and discharge characteristics [9]. It is derived from the State Inpatient Databases (SID), which compiles billing information from non-Federal US hospitals excluding centers for rehabilitation or long-term acute care. As part of the Healthcare Cost and Utilization Project (HCUP), NIS is funded by the Agency for Healthcare Research and Quality (AHRQ). NIS underwent several changes in 2011–2017. Previously, NIS derived all its data from 1000 hospitals; since 2014, it began gathering data from a fraction of discharges from all hospitals [9, 10]. It was further updated in 2015 to follow ICD-10. This study adheres to the updated NIS guidelines [11].
Variables of interest for this study were chosen using a search engine that browses for keywords in a database integrating the official CMS ICD-9 to ICD-10 conversion tables as well as diagnosis-related group (DRG) sets for each ICD system [12,13,14,15,16,17,18,19]. Cross-linking between the ICD codes allowed for variables to be selected with minimum heterogeneity.
Study cohort and study variables
The study cohort includes patients who underwent either total or partial gastrectomy (surgical removal of the stomach) for the treatment of gastric cancer; those younger than 18 years old and those who received multiple procedures were not excluded in the analysis. Frailty was used as the exposure variable to divide the cohort into frailty-present and frailty-absent cohorts. Like previous National Inpatient Studies, this study employs the Johns Hopkins ACG definition of frailty [20,21,22], a diagnostic index composed of criteria, such as dementia, housing needs and homelessness, difficulties with ambulation, weight loss and feeding difficulties, vision impairment, frequent falls, urinary and fecal incontinence, malnutrition, and pressure ulcerations. The primary endpoints investigated in this study are mortality, length of stay, hospitalization costs, and disposition at discharge. Secondary endpoints include postoperative bleeding, postoperative infection (i.e., surgical-site infections, infections of the postsurgical seroma, postsurgical abscesses, peritonitis/abdominal wall infections, internal abscesses, sepsis, and other deep and superficial surgery-related infections), postoperative wound complications (i.e., disruptions in the surgical wound and disruptions due to trauma, wound dehiscence, and fistulous malformations), and postoperative respiratory failure. Further analysis of subgroups divided by age (younger than 65 years vs 65 years and older) and by gastrectomy type (partial vs total) was conducted and recorded in the supplementary tables. All variables used along with their corresponding ICD-9 and 10 codes are documented in the supplementary tables.
Study design and statistical analysis
Propensity-score matching between cohorts was conducted using the following covariates: age, gender (female), race, diabetes, hyperlipidemia, hypertension, chronic obstructive pulmonary disease, coronary artery disease, chronic kidney disease, congestive heart failure, coagulopathy, alcohol use disorder, cigarette use, obesity, nature of procedure (emergent vs non-emergent in relation to time of admission), spread to lymph nodes, spread to non-gastrointestinal organs, spread to gastrointestinal organs, and chemotherapy history. These comorbidities were designated covariates based on their projected impact on mortality and clinical outcomes. Post matching, the frailty-present and frailty-absent cohorts underwent univariate and multivariate analyses. In univariate analysis, parametric/non-parametric tests in addition to Chi-squared or Fisher’s Exact tests were employed to compare mean values for demographics, medical comorbidities, socioeconomic status, hospital information, and other endpoints. The multivariate analysis generated primary endpoints (mortality, length of stay, hospitalization costs, and disposition at discharge) as dependent variables through either logistic or Poisson’s regression analysis while controlling for variables excluded from the matching process. All multivariate findings were evaluated for multicollinearity, fit, and accuracy using several analyses: Akaike information criterion (AIC) assessment, Bayesian information criterion (BIC) assessment, and variance inflation factor (VIF) analysis [23,24,25]. For every endpoint, adjusted and non-adjusted odd ratios were generated with confidence intervals, and statistical significance was assigned to p values less than 0.05.
The multivariate imputation by chained equation (MICE) method was used to fill in any missing NIS data. The MICE method is commonly employed by large database studies over singular imputation methods for its relative accuracy in imputing missing values, owed to its process of running multiple sequential imputations according to feedback [26,27,28].
All calculations involved in analysis were generated by Rstudio version 1.2.5042 with R code version 3.6.3. With all data originating from the HCUP-NIS database, this study was not required to undergo National Review Board or institutional review board approval.
Results
Patient selection
Figure 1 outlines the patient selection procedure of the study. Of 5,286 patients comprising the initial pre-match cohort, 1171 patients with and 1171 patients without frailty were included in the post-match cohort.
Comparison of demographics and comorbidities
Table 1 demonstrates pre-match and post-match information on the demographics and comorbidities of gastrectomy patients with and without frailty. There were no differences in age, gender, race, or in the incidence of medical, gastric, and cancer-related comorbidities between the two cohorts following the matching process.
Comparison of socioeconomic status and hospital characteristics
Table 2 demonstrates pre- and post-match socioeconomic and hospital data for frail and non-frail patients who underwent gastrectomy. After matching, patients with frailty were more likely to be in the lowest income quartile and less likely to be seen in hospitals in the Northeast. They were not significantly different in terms of hospital location (urban vs rural), hospital teaching status, or method of payment.
Comparison of hospital outcomes and complications
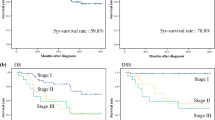
Table 3 demonstrates pre- and post-match hospital outcomes of patients undergoing gastrectomy. After matching, patients with frailty had higher mortality (6.83 vs 3.50% p < 0.001, OR 2.02 95%CI 1.37–2.97), longer length of stay (16.7 vs 12.0d; p < 0.001), and higher costs ($191,418 vs $131,367; p < 0.001) than patients without frailty. They were more likely to be discharged to non-routine care facilities or die during hospitalization. Regarding postoperative complications, frail patients had an increased incidence of postoperative wound complications (3.42 vs 0.94% p < 0.001, OR 3.73 95%CI 1.90–7.31), infection (5.98 vs 3.67% p = 0.012, OR 1.67 95%CI 1.13–2.46), and respiratory failure (6.32 vs 3.84% p = 0.0084, OR 1.69 95%CI 1.15–2.47), but no difference in bleeding complications. Multivariate analysis confirmed the univariate findings in showing frail patients to have increased mortality (p < 0.001, aOR 2.04 95%CI 1.38–3.01), length of stay (p < 0.001, aOR 1.40 95%CI 1.37–1.43), and hospitalization costs (p < 0.001, aOR 1.46 95%CI 1.46–1.46). Figure 2 demonstrates the effects of frailty on post-gastrectomy outcomes using mortality as the primary outcome variable. Furthermore, this combined model includes sub-stratified populations who underwent either partial or total gastrectomy (which is represented in the supplementary tables — see below).
Supplementary tables
Additional post-match subgroup analyses are documented in Supplementary Tables 2 and 3. Supplementary Table 2 compares clinical outcomes of younger (< 65 years) and older patients (≥ 65 years); frailty increases primary outcomes for both cohorts except for mortality in the younger cohort. Supplementary Table 3 compares clinical outcomes for partial and total gastrectomy; all primary endpoints are increased except for mortality in patients receiving total gastrectomy. The cohort-specific stratifications as per the Johns Hopkins ACG frailty criteria are shown in Supplementary Fig. 4.
Discussion
Our post-match findings show that mortality, length of hospital stay, and total cost of care are significantly increased in individuals with frailty undergoing gastrectomy compared to those without frailty. Frailty is also shown to be an independent risk factor for post-procedural complications, such as infection, respiratory failure, and wound complications, and to increase the likelihood of discharge to additional care facilities. Our findings in the supplementary tables confirm the adverse effects of frailty on both age cohorts, though on a greater scale in the elderly.
A large number of cohort studies have attempted to investigate the effects of frailty on post-gastrectomy outcomes. One shortcoming, however, is their utilization of a variety of criteria and indices in classifying frailty, which presents an ongoing challenge in interpreting the collective data [1, 29]. Our study uses the Johns Hopkins ACG system, which defines frailty based on the combined presence of the following domains: malnutrition, impaired vision, dementia, decubitus ulcers, fecal and urinary incontinence, loss of weight, digestive difficulties, poverty, inadequate housing, difficulty in walking, and falls. The findings from our study corroborate several prior studies that demonstrate the positive association between the domains of frailty and mortality, length of stay, and post-operative complications in patients receiving major resective procedures, such as gastrectomy [30,31,32]. Our study strengthens these findings by assessing the effects of frailty across a cohort derived from a national database, using propensity-score matching to optimize the accuracy of analysis. Moreover, it evaluates these effects separately in elderly and younger cohorts, which allows us to further elucidate trends that may vary based on age.
Frailty negatively affects clinical outcomes through numerous physiological mechanisms, especially in patients undergoing high-risk procedures [33]. In general, the state of nutritional deficiency in a frail patient impedes the calorically taxing processes involved in post-surgical recovery [34,35,36]. Protein and energy insufficiency impairs proper wound healing, coagulation, and immunological defenses, which elevates the risk of infection and bleeding [37, 38]. Decreased energy stores also depress neural drive and muscular strength, both of which may contribute to deterioration in diaphragmatic function and ultimately to post-procedural respiratory complications. Furthermore, the ambulatory decline and overall weakness that accompany the diagnosis of frailty subject patients to a higher risk of falls or injury, prolong their stay in the hospital and raising cost of treatment [39]. With delayed discharge, patients are prone to subsequent complications, such as decubitus ulcers and acquired infections, contributing to further disruption from recovery [40].
Frailty’s propensity to induce adverse post-procedural outcomes, as demonstrated in this study, renders it essential for patients to be screened early for indications of frailty during their preoperative assessment. Once components of frailty are identified, clinicians should aim to mitigate those responsive to treatment, such as malnutrition or poor physical performance, through measures, such as dietary supplementation and guided physical training [41, 42]. After the procedure, it is advisable to place the patient under the supervision of a multidisciplinary team that can provide integrated care in multiple areas, such as nutrition, wound care, and respiratory support [43]].
One noteworthy finding in this study was that mortality was not significantly increased in frail patients receiving total gastrectomy, unlike for partial gastrectomy, where a significant increase was seen. While the precise mechanism for this cannot be exacted, part of the reason may be due to the fact that total gastrectomy is a much more invasive and comprehensive procedure with implicitly higher mortality and complication risks, thus diminishing the effect of frailty on its overall outcomes.
Limitations
The primary limitation of this paper pertains to the nature of the database used; the NIS database does not contain post discharge information, which limits the study results to the cross-sectional evaluation performed during admission and in-hospital postoperative course. While the immediate effects of frailty are well characterized in this study, a follow-up prospective study would be helpful in delineating the long-term effects of frailty on patient recovery.
References
Fried LP, Tangen CM, WalstonNewman JAB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group. Frailty in older adults evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, Xue Q-L, Walston JD, Kasper JD. Frailty in older adults: a nationally representative profile in the United States. J Gerontol A Biol Sci Med Sci. 2015;70(11):1427–34.
Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC, Moss M. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg. 2013;206(4):544–50. https://doi.org/10.1016/j.amjsurg.2013.03.012.
Lin H-S, Watts JN, Peel NM, Hubbard RE. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016;16(1):157.
Lu J, Cao L-L, Zheng C-H, Li P, Xie J-W, Wang J-B, Lin J-X, Chen Q-Y, Lin M, Tu R-H, Huang C-M. The Preoperative frailty versus inflammation-based prognostic score: which is better as an objective predictor for gastric cancer patients 80 years and older? Ann Surg Oncol. 2017;24(3):754–62.
Tegels JJW, de Maat MFG, Hulsewé KWE, Hoofwi AGM, Stoot MB. Value of geriatric frailty and nutritional status assessment in predicting postoperative mortality in gastric cancer surgery. J Gastrointest Surg. 2014;18(3):439–45 (discussion 445-446).
Agarwal E, Miller M, Yaxley A, Isenring E. Malnutrition in the elderly: a narrative review. Maturitas. 2013;76(4):296–302.
Ryan AM, Healy LA, Power DG, Rowley SP, Reynolds JV. Short-term nutritional implications of total gastrectomy for malignancy, and the impact of parenteral nutritional support. Clin Nutr. 2007;26(6):718–27.
Healthcare Cost and Utilization Project (HCUP). 2017 Introduction to the HCUP National Inpatient Sample (NIS). U.S. Agency for Healthcare Research and Quality, Rockville, MD; 2019. https://www.hcup-us.ahrq.gov/db/nation/nis/NISIntroduction2017.pdf. Accessed 20 Sept 2020.
Houchens R, Ross D, Elixhauser A, Jiang J. Nationwide Inpatient Sample (NIS) Redesign Final Report. U.S. Agency for Healthcare Research and Quality, Rockville MD; 2014. https://www.hcup-us.ahrq.gov/reports/methods/2014-04.pdf. Accessed 21 Aug 2020.
Elixhauser A, Heslin KC, Owens PL. Healthcare Cost And Utilization Project (HCUP) Recommendations for Reporting Trends Using ICD-9-CM and ICD-10-CM/PCS Data. U.S. Agency for Healthcare Research and Quality; 2017. https://www.hcup-us.ahrq.gov/datainnovations/HCUP_RecomForReportingTrends_070517.pdf. Accessed 6 March 2017.
Centers for Medicare and Medicaid Services. 2017 ICD-10 PCS Code Descriptions. Published online August 22, 2016. https://www.cms.gov/Medicare/Coding/ICD10/Downloads/2017-PCS-Long-Abbrev-Titles.zip. Accessed 17 Aug 2020.
Centers for Medicare and Medicaid Services (CMS). 2017 ICD-10-CM Code Descriptions. Published online August 22, 2016. https://www.cms.gov/Medicare/Coding/ICD10/Downloads/2017-ICD10-Code-Descriptions.zip. Accessed 17 Aug 2020.
Centers for Medicare and Medicaid Services (CMS). ICD-9-CM and PCS diagnosis and procedure codes descriptions version 32. Published online October 1, 2014. https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/Downloads/ICD-9-CM-v32-master-descriptions.zip. Accessed 17 Aug 2020.
Centers for Medicare and Medicaid Services (CMS). 2017 ICD-10 PCS General Equivalence Mappings (GEMs) – Procedure Codes. Published online December 1, 2016. https://www.cms.gov/Medicare/Coding/ICD10/Downloads/2017-GEM-PCS.zip. Accessed 17 Aug 2020.
Centers for Medicare and Medicaid Services (CMS). 2017 ICD-10-CM General Equivalence Mappings (GEMs) – Diagnosis Codes. Published online August 22, 2016. https://www.cms.gov/Medicare/Coding/ICD10/Downloads/2017-GEM-DC.zip. Accessed 17 Aug 2020.
Centers for Medicare and Medicaid Services (CMS). ICD-10 Definition of Medicare Code Edits V37.2. Published online August 2020. https://www.cms.gov/files/zip/definition-medicare-code-edits-v372.zip. Accessed 17 Aug 2020.
Centers for Medicare and Medicaid Services (CMS). ICD-10 MS-DRG Definitions Manual Files V37.2. Published online August 2020. https://www.cms.gov/files/zip/icd-10-ms-drg-definitions-manual-files-v372.zip. Accessed 17 Aug 2020.
Fung KW, Richesson R, Smerek M, Pereira KC, Green BB, Patkar A, Clowse M, Bauck A, Bodenreider O. Preparing for the ICD-10-CM transition: automated methods for translating ICD codes in clinical phenotype definitions. EGEMS (Wash DC). 2016;4(1):1211.
The Johns Hopkins ACG® System Excerpt from Version 11.0 Technical Reference Guide. Published online Nov 2014. https://www2.gov.bc.ca/assets/gov/health/conducting-health-research/data-access/johns-hopkins-acg-system-technical-reference-guide.pdf?bcgovtm=buffer. Accessed Nov 2014.
Asemota AO, Gallia GL. Impact of frailty on short-term outcomes in patients undergoing transsphenoidal pituitary surgery. J Neurosurg. 2019;132(2):360–70.
Xu D, Fei M, Lai Y, Shen Y, Zhou J. Impact of frailty on inpatient outcomes in thyroid cancer surgery: 10-year results from the U.S. national inpatient sample. J Otolaryngol Head Neck Surg. 2020;49(1):51.
Cherkassky V, Ma Y. Comparison of model selection for regression. Neural Comput. 2003;15(7):1691–714.
Burnham KP, Anderson DR. Multimodel Inference: understanding AIC and BIC in model selection. Sociol Methods Res. 2004;33(2):261–304.
Chakrabarti A, Ghosh JK. AIC, BIC and recent advances in model selection. In: Bandyopadhyay PS, Forster MR, editors. Philosophy of statistics, vol. 7. North-Holland: Elsevier; 2011.
Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4(2):30.
Liu Y, Han H, Shah G, Giralt S, Ola Landgren C, He J, Lesokhin AM. Significant nationwide variability in the costs and hospital mortality rates of autologous stem cell transplantation for multiple myeloma: an analysis of the nationwide inpatient sample database. Biol Blood Marrow Transplant. 2019;25(1):41–6.
Houchens R. Missing Data Methods for the NIS and the SID. HCUP Methods Series. Published online 2015. http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Accessed 9 Dec 2020.
Rockwood K, Hogan DB, MacKnight C. Conceptualisation and measurement of frailty in elderly people. Drugs Aging. 2000;17(4):295–302.
Shen Y, Hao Q, Zhou J, Dong B. The impact of frailty and sarcopenia on postoperative outcomes in older patients undergoing gastrectomy surgery: a systematic review and meta-analysis. BMC Geriatr. 2017;17(1):188.
Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried LP. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–8.
Sandini M, Pinotti E, Persico I, Picone D, Bellelli G, Gianotti L. Systematic review and meta-analysis of frailty as a predictor of morbidity and mortality after major abdominal surgery. BJS Open. 2017;1(5):128–37.
Mosquera C, Spaniolas K, Fitzgerald TL. Impact of frailty on surgical outcomes: the right patient for the right procedure. Surgery. 2016;160(2):272–80.
Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB Jr, Walston JD, Interventions on Frailty Working Group. Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: a consensus report. J Am Geriatr Soc. 2004;52(4):625–34.
Dasgupta M, Rolfson DB, Stolee P, Borrie MJ, Speechley M. Frailty is associated with postoperative complications in older adults with medical problems. Arch Gerontol Geriatr. 2009;48(1):78–83.
Chen X, Mao G, Leng SX. Frailty syndrome: an overview. Clin Interv Aging. 2014;9:433–41.
Bendayan M, Messas N, Perrault LP, Asgar AW, Lauck S, Kim DH, Arora RC, Langlois Y, Piazza N, Martucci G, Lefèvre T, Noiseux N, Lamy A, Peterson MD, Labinaz M, Popma JJ, Webb JG, Afilalo J. Frailty and bleeding in older adults undergoing TAVR or SAVR: insights from the FRAILTY-AVR study. JACC Cardiovasc Interv. 2020;13(9):1058–68.
Farhat JS, Velanovich V, Falvo AJ, Horst HM, Swartz A, Patton JH, Rubinfeld IS. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg. 2012;72(6):1526–30 (discussion 1530–1531).
Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, Tracy K, Hochberg MC, Rodondi N, Cawthon PM, Study of Osteoporotic Fractures Research Group. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007;62(7):744–51.
Eachempati SR, Hydo LJ, Barie PS. Factors influencing the development of decubitus ulcers in critically ill surgical patients. Crit Care Med. 2001;29(9):1678–82.
Ng TP, Feng L, Nyunt MSZ, Feng L, Niti M, Tan BY, Chan G, Khoo SA, Chan SM, Yap P, Yap KB. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled trial. Am J Med. 2015;128(11):1225-1236.e1. https://doi.org/10.1016/j.amjmed.2015.06.017.
Cameron ID, Fairhall N, Langron C, Lockwood K, Monaghan N, Aggar C, Sherrington C, Lord SR, Kurrle SE. A multifactorial interdisciplinary intervention reduces frailty in older people: randomized trial. BMC Med. 2013. https://doi.org/10.1186/1741-7015-11-65.
Braga M, Pecorelli N, Scatizzi M, Borghi F, Missana G, Radrizzani D, PeriOperative Italian Society. Enhanced recovery program in high-risk patients undergoing colorectal surgery: results from the PeriOperative Italian Society Registry. World J Surg. 2017;41(3):860–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript certify they share no affiliation or involvement with any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. None declared.
Ethics approval
The research conducted in this study did not require the use of human subject data. This study was conducted via the use of publicly available de-identified database that did not require approval from the local or global IRB bodies. This study nevertheless followed all the required protocols of the HCUP database handling guidelines, to ensure that the quality of work produced was in line with the data-use agreement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, D.U., Kwon, J., Han, J. et al. The clinical impact of frailty on the postoperative outcomes of patients undergoing gastrectomy for gastric cancer: a propensity-score matched database study. Gastric Cancer 25, 450–458 (2022). https://doi.org/10.1007/s10120-021-01265-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-021-01265-7