Abstract
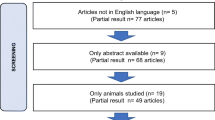
Photobiomodulation (PBM) has been emerging as a promising alternative therapy in dentistry. However, various parameters of PBM are used in different studies, and there is limited cumulative data on PBM for improving bone formation in clinical trials. The aim of this review was to evaluate the effectiveness of PBM in the process of bone remodeling in dentistry using randomized controlled trials. Initially, a total of 1,011 articles published from January 2008 to December 2021 were retrieved from five electronic databases (PubMed, Scopus, Cochrane Library, EMBASE, and CINAHL). After a two-step review, nine articles met the inclusion criteria. The parameter of PBM, group, treatment sessions, assessment times and outcomes of the included studies were reviewed. Eighty-nine percent of the studies revealed positive effects on bone formation between the laser group and the control group. Only one article reported that light-emitting diode did not significantly enhance osteogenesis. Additionally, the present study shows that Gallium aluminum arsenide of near infrared (NIR) laser with continuous mode is the most commonly used form of PBM. The biostimulatory effects are dependent on several parameters, with wavelength and dose being more important than others. Based on this review, it is suggested that the NIR range and an appropriate dose of PBM could be used to increase the efficiency of stimulating bone healing and remodeling. However, standardization of treatment protocols is needed to clarify therapeutic strategies in dentistry.




Similar content being viewed by others
Data availability
Data used to support the findings of this study are included in the article.
References
Oshiro T, Calderhead RG (1988) Low level laser therapy: a practical introduction. United Kingdom, Chichester
Karu T (1999) Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol, B 49:1–17. https://doi.org/10.1016/S1011-1344(98)00219-X
Karu TI, Kolyakov SF (2005) Exact action spectra for cellular responses relevant to phototherapy. Photomed Laser Ther 23:355–361. https://doi.org/10.1089/pho.2005.23.355
de Freitas LF, Hamblin MR (2016) Proposed mechanisms of photobiomodulation or low-level light therapy. IEEE J Sel Top Quantum Electron 22. https://doi.org/10.1109/JSTQE.2016.2561201
Henderson TA, Morries LD (2015) Near-infrared photonic energy penetration: can infrared phototherapy effectively reach the human brain? Neuropsychiatr Dis Treat 11:2191–2208. https://doi.org/10.2147/NDT.S78182
Chen CH, Hung HS, Hsu SH (2008) Low-energy laser irradiation increases endothelial cell proliferation, migration, and eNOS gene expression possibly via PI3K signal pathway. Lasers Surg Med 40:46–54. https://doi.org/10.1002/lsm.20589
Maiman TH (1960) Stimulated optical radiation in ruby. Nature 187:493–494. https://doi.org/10.1038/187493a0
Taylor R, Shklar G, Roeber F (1965) The effects of laser radiation on teeth, dental pulp, and oral mucosa of experimental animals. Oral Surg Oral Med Oral Pathol 19:786–795. https://doi.org/10.1016/0030-4220(65)90351-8
Lobene RR, Samuel Fine SM (1966) Interaction of laser radiation with oral hard tissues. J Prosthet Dent 16:589–597. https://doi.org/10.1016/0022-3913(66)90066-7
AlGhamdi KM, Kumar A, Moussa NA (2012) Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells. Lasers Med Sci 27:237–249. https://doi.org/10.1007/s10103-011-0885-2
Pires Oliveira DA, de Oliveira RF, Zangaro RA, Soares CP (2008) Evaluation of low-level laser therapy of osteoblastic cells. Photomed Laser Surg 26:401–404. https://doi.org/10.1089/pho.2007.2101
Hamblin MR (2017) Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys 4:337–361. https://doi.org/10.3934/biophy.2017.3.337
Prabhu V, Rao SB, Rao NB, Aithal KB, Kumar P, Mahato KK (2010) Development and evaluation of fiber optic probe-based helium-neon low-level laser therapy system for tissue regeneration–an in vivo experimental study. Photochem Photobiol 86:1364–1372. https://doi.org/10.1111/j.1751-1097.2010.00791.x
Reza B, Soheil N, Ehsan B, Kourosh S, Reza F (2021) Efficacy of photo bio-modulation therapy for pain relief and soft tissue wound healing after dental implant surgery: A double-blind randomized clinical trial. J Photochem Photobiol 8:100062. https://doi.org/10.1016/j.jpap.2021.100062
Gur A, Sarac AJ, Cevik R, Altindag O, Sarac S (2004) Efficacy of 904 nm gallium arsenide low level laser therapy in the management of chronic myofascial pain in the neck: a double-blind and randomize-controlled trial. Lasers Surg Med 35:229–235. https://doi.org/10.1002/lsm.20082
Langella LG, Casalechi HL, Tomazoni SS et al (2018) Photobiomodulation therapy (PBMT) on acute pain and inflammation in patients who underwent total hip arthroplasty-a randomized, triple-blind, placebo-controlled clinical trial. Lasers Med Sci 33:1933–1940. https://doi.org/10.1007/s10103-018-2558-x
Zayed SM, Hakim AAA (2020) Clinical efficacy of photobiomodulation on dental implant osseointegration: a systematic review. Saudi J Med Med Sci 8:80–86. https://doi.org/10.4103/sjmms.sjmms_410_19
Sourvanos D, Poon J, Lander B, Sarmiento H, Carroll J, Zhu TC, Fiorellini JP (2023) Improving titanium implant stability with photobiomodulation: a review and meta-analysis of irradiation parameters. Photobiomodul Photomed Laser Surg 41:93–103. https://doi.org/10.1089/photob.2022.0161
Poli PP, Jesus LK, Dayube URC et al (2022) An Evaluation of the effects of photobiomodulation therapy on the peri-Implant bone healing of implants with different surfaces: an in vivo study. Materials 15:4371. https://doi.org/10.3390/ma15134371
Magri AMP, Fernandes KR, Assis L et al (2015) Photobiomodulation and bone healing in diabetic rats: evaluation of bone response using a tibial defect experimental model. Lasers Med Sci 30:1949–1957. https://doi.org/10.1007/s10103-015-1789-3
Bai J, Li L, Kou N et al (2021) Low level laser therapy promotes bone regeneration by coupling angiogenesis and osteogenesis. Stem Cell Res Ther 12:1–18. https://doi.org/10.1186/s13287-021-02493-5
Kawasaki K, Shimizu N (2000) Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg Med 26:282–291. https://doi.org/10.1002/(sici)1096-9101(2000)26:3%3c282::aid-lsm6%3e3.0.co;2-x
Hadjidakis DJ, Androulakis II (2006) Bone remodeling. Ann N Y Acad Sci 1092:385–396. https://doi.org/10.1196/annals.1365.035
Stein A, Benayahu D, Maltz L, Oron U (2005) Low-level laser irradiation promotes proliferation and differentiation of human osteoblasts in vitro. Photomed Laser Surg 23:161–166. https://doi.org/10.1089/pho.2005.23.161
Ninomiya T, Hosoya A, Nakamura H, Sano K, Nishisaka T, Ozawa H (2007) Increase of bone volume by a nanosecond pulsed laser irradiation is caused by a decreased osteoclast number and an activated osteoblasts. Bone 40:140–148. https://doi.org/10.1016/j.bone.2006.07.026
Ribeiro LNS, de Figueiredo FAT, da Silva Mira PC et al (2022) Low-level laser therapy (LLLT) improves alveolar bone healing in rats. Lasers Med Sci 37:961–969. https://doi.org/10.1007/s10103-021-03340-y
Standal T, Borset M, Sundan A (2004) Role of osteopontin in adhesion, migration, cell survival and bone remodeling. Exp Oncol 26:179–184
Ingram RT, Clarke BL, Fisher LW, Fitzpatrick LA (1993) Distribution of noncollagenous proteins in the matrix of adult human bone: evidence of anatomic and functional heterogeneity. J Bone Miner Res 8:1019–1029. https://doi.org/10.1002/jbmr.5650080902
Hauschka PV, Lian JB, Cole DE, Gundberg CM (1989) Osteocalcin and matrix Gla protein: vitamin K-dependent proteins in bone. Physiol Rev 69:990–1047. https://doi.org/10.1152/physrev.1989.69.3.990
Khadra M, Lyngstadaas SP, Haanaes HR, Mustafa K (2005) Effect of laser therapy on attachment, proliferation and differentiation of human osteoblast-like cells cultured on titanium implant material. Biomaterials 26:3503–3509. https://doi.org/10.1016/j.biomaterials.2004.09.033
Zhou Y, Sun F, Zhang Z et al (2023) Influence of Er: YAG laser irradiation on the outcomes of alveolar ridge preservation at the infected molar sites: a randomized controlled trial. BMC Oral Health 23:1–12. https://doi.org/10.1186/s12903-023-02996-y
Monea A, Beresescu G, Boeriu S, Tibor M, Popsor S, Antonescu DM (2015) Bone healing after low-level laser application in extraction sockets grafted with allograft material and covered with a resorbable collagen dressing: A pilot histological evaluation. BMC Oral Health 15:134. https://doi.org/10.1186/s12903-015-0122-7
Boldrini C, de Almeida JM, Fernandes LA et al (2013) Biomechanical effect of one session of low-level laser on the bone-titanium implant interface. Lasers Med Sci 28:349–352. https://doi.org/10.1007/s10103-012-1167-3
Lopes CB, Pinheiro AL, Sathaiah S, Da Silva NS, Salgado MA (2007) Infrared laser photobiomodulation (lambda 830 nm) on bone tissue around dental implants: a Raman spectroscopy and scanning electronic microscopy study in rabbits. Photomed Laser Surg 25:96–101. https://doi.org/10.1089/pho.2006.2030
Khadra M, Ronold HJ, Lyngstadaas SP, Ellingsen JE, Haanaes HR (2004) Low-level laser therapy stimulates bone-implant interaction: an experimental study in rabbits. Clin Oral Implants Res 15:325–332. https://doi.org/10.1111/j.1600-0501.2004.00994.x
Maluf AP, Maluf RP, Brito Cda R, Franca FM, de Brito Jr RB (2010) Mechanical evaluation of the influence of low-level laser therapy in secondary stability of implants in mice shinbones. Lasers Med Sci 25:693–698. https://doi.org/10.1007/s10103-010-0778-9
Fernandes KR, Magri AMP, Kido HW et al (2017) Biosilicate/PLGA osteogenic effects modulated by laser therapy: In vitro and in vivo studies. J Photochem Photobiol B 173:258–265. https://doi.org/10.1016/j.jphotobiol.2017.06.002
Pinheiro ALB, Santos NRS, Oliveira PC et al (2013) The efficacy of the use of IR laser phototherapy associated to biphasic ceramic graft and guided bone regeneration on surgical fractures treated with miniplates: a Raman spectral study on rabbits. Lasers Med Sci 28:513–518. https://doi.org/10.1007/s10103-012-1096-1
Fangel R, Bossini PS, Renno AC et al (2011) Low-level laser therapy, at 60 J/cm2 associated with a Biosilicate® increase in bone deposition and indentation biomechanical properties of callus in osteopenic rats. J Biomed Opt 16:078001. https://doi.org/10.1117/1.3598847
Ross G, Ross A (2009) Photobiomodulation: an invaluable tool for all dental specialties. J Laser Dent 17:117–124
Goyal M, Makkar S, Pasricha S (2013) Low level laser therapy in dentistry. Int J Laser Dent 3:82–88. https://doi.org/10.5005/jp-journals-10022-1043
Kotlow L (2009) Photobiomodulating lasers and children’s dental care. J Laser Dent 17:125–130
Carroll JD, Milward MR, Cooper PR, Hadis M, Palin WM (2014) Developments in low level light therapy (LLLT) for dentistry. Dent Mater 30:465–475. https://doi.org/10.1016/j.dental.2014.02.006
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Zahra SE, Elkasi AA, Eldin MS, Vandevska-Radunovic V (2009) The effect of low level laser therapy (LLLT) on bone remodelling after median diastema closure: A one year and half follow-up study. Orthodontic Waves 68:116–122. https://doi.org/10.1016/j.odw.2009.02.001
Angeletti P, Pereira MD, Gomes HC, Hino CT, Ferreira LM (2010) Effect of low-level laser therapy (GaAlAs) on bone regeneration in midpalatal anterior suture after surgically assisted rapid maxillary expansion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:e38-46. https://doi.org/10.1016/j.tripleo.2009.10.043
Romao MM, Marques MM, Cortes AR, Horliana AC, Moreira MS, Lascala CA (2015) Micro-computed tomography and histomorphometric analysis of human alveolar bone repair induced by laser phototherapy: a pilot study. Int J Oral Maxillofac Surg 44:1521–1528. https://doi.org/10.1016/j.ijom.2015.08.989
Zaky AA, El Shenawy HM, Harhsh TA, Shalash M, Awad NM (2016) Can low level laser therapy benefit bone regeneration in localized maxillary cystic defects? - a prospective randomized control trial. Open Access Maced J Med Sci 4:720–725. https://doi.org/10.3889/oamjms.2016.140
Matys J, Swider K, Grzech-Lesniak K, Dominiak M, Romeo U (2019) Photobiomodulation by a 635nm diode laser on peri-implant bone: primary and secondary stability and bone density analysis-a randomized clinical trial. Biomed Res Int 2019:2785302. https://doi.org/10.1155/2019/2785302
Gulati P, Kumar M, Issar G, Thakral A (2020) Effect of low level laser therapy on crestal bone levels around dental implants-A pilot study. Clin Implant Dent Relat Res 22:739–746. https://doi.org/10.1111/cid.12957
Rosero KAV, Sampaio RMF, Deboni MCZ et al (2020) Photobiomodulation as an adjunctive therapy for alveolar socket preservation: a preliminary study in humans. Lasers Med Sci 35:1711–1720. https://doi.org/10.1007/s10103-020-02962-y
Arshad M, Ghanavati Z, Aminishakib P, Rasouli K, Shirani G (2021) Effect of light-emitting diode phototherapy on allograft bone after open sinus lift surgery: a randomized clinical trial (Concurrent Parallel). J Lasers Med Sci 12:e16. https://doi.org/10.34172/jlms.2021.16
Križaj Dumić A, Pajk F, Olivi G (2021) The effect of post-extraction socket preservation laser treatment on bone density 4 months after extraction: Randomized controlled trial. Clin Implant Dent Relat Res 23:309–316. https://doi.org/10.1111/cid.12991
Lubart R, Friedmann H, onitLavie R (2000) Photobiostimulation as a function of different wavelengths. Laser Ther 12:38–41. https://doi.org/10.5978/islsm.12.38
Kushibiki T, Hirasawa T, Okawa S, Ishihara M (2015) Low Reactive Level Laser Therapy for Mesenchymal Stromal Cells Therapies. Stem Cells Int 2015:974864. https://doi.org/10.1155/2015/974864
Barbosa D, de Souza RA, Xavier M, da Silva FF, Arisawa EA, Villaverde AG (2013) Effects of low-level laser therapy (LLLT) on bone repair in rats: optical densitometry analysis. Lasers Med Sci 28:651–656. https://doi.org/10.1007/s10103-012-1125-0
Su CT, Chen CM, Chen CC, Wu JH (2020) Dose analysis of photobiomodulation therapy in stomatology. Evid Based Complement Alternat Med 2020:8145616. https://doi.org/10.1155/2020/8145616
Su CT, Chiu FC, Ma SH, Wu JH (2022) Optimization of photobiomodulation dose in biological tissue by adjusting the focal point of lens. Photonics 9:350. https://doi.org/10.3390/photonics9050350
Barbosa D, Villaverde AG, LoschiavoArisawa EA, de Souza RA (2014) Laser therapy in bone repair in rats: analysis of bone optical density. Acta Ortop Bras 22:71–74. https://doi.org/10.1590/1413-78522014220200438
Batista JD, Sargenti-Neto S, Dechichi P, Rocha FS, Pagnoncelli RM (2015) Low-level laser therapy on bone repair: is there any effect outside the irradiated field? Lasers Med Sci 30:1569–1574. https://doi.org/10.1007/s10103-015-1752-3
Heiskanen V, Hamblin MR (2018) Photobiomodulation: lasers vs. light emitting diodes? Photochem Photobiol Sci 17:1003–1017. https://doi.org/10.1039/c8pp00176f
Karu TI, Andreichuk T, Ryabykh T (1993) Changes in oxidative metabolism of murine spleen following diode laser (660–950nm) irradiation: effect of cellular composition and radiation parameters. Lasers Surg Med 13:453–462. https://doi.org/10.1002/lsm.1900130410
Park JB, Ahn SJ, Kang YG, Kim EC, Heo JS, Kang KL (2015) Effects of increased low-level diode laser irradiation time on extraction socket healing in rats. Lasers Med Sci 30:719–726. https://doi.org/10.1007/s10103-013-1402-6
da Silva RV, Camilli JA (2006) Repair of bone defects treated with autogenous bone graft and low-power laser. J Craniofac Surg 17:297–301. https://doi.org/10.1097/00001665-200603000-00017
da Fonseca GAMD, Cavalcanti MFXB, de Souza Maior JD et al (2022) Laser-photobiomodulation on titanium implant bone healing in rat model: comparison between 660-and 808-nm wavelength. Lasers Med Sci 37:2179–2184. https://doi.org/10.1007/s10103-021-03481-0
Cobb CM (2006) Lasers in periodontics: a review of the literature. J Periodontol 77:545–564. https://doi.org/10.1902/jop.2006.050417
Farkas JP, Hoopman JE, Kenkel JM (2013) Five parameters you must understand to master control of your laser/light-based devices. Aesthetic Surg J 33:1059–1064. https://doi.org/10.1177/1090820X13501174
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
J.R. Mi Le (Jie-Ren Mi Le) and C.T. Su (Chuan-Tsung Su) contributed to data preparation and collection, studies review, data analysis, and data interpretation. C.-T.S and J. H. Wu. contributed to idea formulation, reporting results, and the writing of the manuscript. Fu-Shan Jaw (F.S. Jaw) and C.T. Su contributed to review and editing. All authors have seen and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Le, JR.M., Wu, JH., Jaw, FS. et al. The effect of bone remodeling with photobiomodulation in dentistry: a review study. Lasers Med Sci 38, 265 (2023). https://doi.org/10.1007/s10103-023-03933-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03933-9