Abstract
Background
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) presents significant treatment challenges due to its chronic nature, varied clinical presentations, and rarity. Subcutaneous immunoglobulin (SCIG) has emerged as a maintenance therapy, offering potential advantages in administration and patient experience over the previously recognized intravenous immunoglobulin (IVIG). Methods: We included all clinical studies involving CIDP patients treated with SCIG from eleven databases up to March 2024.
Results
50 clinical studies were included in the systematic review, with 22 involved in the meta-analysis. These studies offer clinical data on around 1400 CIDP patients. Almost all studies considered SCIG a maintenance therapy, with the majority of results suggesting it as a viable substitute that may offer comparable or enhanced advantages. Studies covered aspects such as efficacy, safety, quality of life, practicality, economic evaluation, and patient preference. Meta-analysis showed SCIG significantly improved muscle strength and sensory function, had fewer and milder side effects, reduced relapse rates, and received a strong preference.
Conclusions
Findings suggest that SCIG for CIDP maintenance not only provides a more feasible alternative, with economic evaluations showing considerable cost reductions over time, and patient preference for SCIG being pronounced, but may also deliver comparable or superior health outcomes. Ongoing research lines on formulations, techniques, and direct comparative studies are critical to further illuminate, enhance, and expand SCIG's role in treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) remains a compound challenge in neurology, due to its nature, spectrum, and rarity. It is caused by a long term immune-mediated demyelinating pathology of peripheral nerves, occurring as rarely as 1 per 100 thousand and presenting with multiple types and disease courses, with the typical and most prevalent form of CIDP involving deficiency in both motor and sensory limb functions and showing symmetry in both right and left, upper and lower, distal and proximal limb regions [1].
However, this condition can indeed be treatable, with treatment aiming to achieve and maintain significant improvement in overall function, symptoms, and quality of life, or even an end goal for some of being stable and off treatment in the long term [2].
CIDP was defined in the 1970s, its reported management with immunoglobulins began with Intravenous Immunoglobulin (IVIG) in the 1980s, Subcutaneous Immunoglobulin (SCIG) in the late 2000s and 2010s, while their official approvals came in the late 2000s for IVIG and late 2010s for SCIG [3,4,5].
As earlier treatments for CIDP were limited and less effective, the adoption of IVIG and subsequently SCIG significantly improved patient outcomes, representing a significant advancement in the management of this autoimmune disorder [6, 7].
The official approvals of SCIGs for CIDP maintenance from the late 2010s forward have expanded treatment options for CIDP patients; however, there is a need to further investigate their comparative benefits and tolerability both objectively and from the patient perspective [7,8,9].
This study intended to assess the efficacy, safety, and convenience of SCIG for CIDP maintenance treatment, using most reported data from most of the available and suited studies retrieved from diverse Databases funneled, condensed, and synthesized through the extensive and organized presentation and analyses, including but not limited to the analysis of overall function, muscle strength, sensory function, serum IgG levels, quality of life, relapse rate, adverse events, patient treatment preferences, and economic implications and considering most reported outcome-measures for the aforementioned outcomes, hence the use of the adjective "comprehensive" in the title.
Methods
We observed the guidelines suggested by the PRISMA statement in conducting this systematic review and meta-analysis. The protocol was registered with PROSPERO, International Prospective Register of Systematic Reviews (ID: CRD42024521670).
Eligibility criteria for included studies
For studies included in the systematic review, we considered the following criteria:
-
1) Study design: All clinical study designs: interventional RCTs and other clinical trials, observational prospective, retrospective or cross-sectional studies, case reports, and case series. Additionally, cost studies were included.
-
2) Participants: Patients with Chronic Inflammatory Demyelinating Polyneuropathy (CIDP), regardless of age, gender, severity of disease, type, or comorbidities
-
3) Interventions: subcutaneous immunoglobulins (SCIG) in any dosage, administration method, or regimen, either alone or in combination with other treatments.
-
4) Comparator: IVIG, different dose, administration method, or regimen of SCIG, placebo, no treatment, standard care, or other pharmacological interventions.
-
5) Outcomes: The main outcomes will pertain to the effectiveness and safety of SCIG in CIDP, using various relevant indicators, functional scores, and adverse events, additionally, cost-effectiveness, practicality, and patient-reported outcomes associated with SCIG for the treatment of CIDP.
Excluded were
1) non-human research studies (laboratory animals, isolated cells, in-vitro), 2) Studies with IVIG alone, or any other interventions not accompanied with or compared to SCIG, 3) Secondary research studies (reviews, systematic reviews, meta-analysis), 4) Non-empirical studies (opinion pieces and hypotheses), and 5) non-peer-reviewed (Book chapters, editorials, and conference abstracts)
The aforementioned rules were of course applied to include the articles in the Systematic review first, but then regarding the meta-analysis case reports, case series, cost studies, and any study that did not assess at least one of the desired outcomes were not involved in the meta-analysis.
Information sources and search strategy
The following databases were searched for publications that were available till 1 March 2024, then the search was updated on 30 March: PubMed/Medline, Web of Science, ScienceDirect, SCOPUS, CLINICALTRIALSGOV, CENTRAL/COCHRANE, ICTRP, Google Scholar, LILACS, Europe PMC, and SpringerLink.
Data sources were searched using the following query: ("chronic inflammatory demyelinating polyneuropathy" OR "CIDP" OR "chronic inflammatory demyelinating polyradiculoneuropathy") AND ("subcutaneous immunoglobulin" OR "SCIG" OR "HyQvia" OR "Hizentra" OR "IgPro20" OR "subcutaneous immunoglobulins"). (More details in the supplementary material).
Study selection
After removing duplicates, two reviewers screened titles and abstracts in a blinded fashion, and studies that met the exclusion criteria were removed. Afterward, full-text screening was performed blindly by two reviewers to assess their eligibility for SR and MA. Any controversies were resolved through discussion or consultation with a third researcher if consensus was not reached.
Data extraction
Two researchers independently extracted the data using a standardized online extraction form for all included studies in the systematic review, except case and cost studies which required 2 other suitable specialized data extraction forms.
According to the standardized data extraction form, the extracted data initially included the following:
1) study ID: author, year, 2) study design, 3) participants: Number, Age in years, Males: n (%), Disease Duration & Age at first diagnosis of CIDP, Baseline disease measures, Inclusion and Exclusion Criteria,4) Intervention: (SCIG), brand name, regimen, etc., Type of treatment (induction, maintenance, or both), 5) Comparator: Detailed as intervention if applicable. If the comparison is to baseline, we mentioned that. 6) Outcomes: Primary Outcome(s), Primary outcome measures, Secondary Outcome(s), Secondary outcome measures, 7) Follow-up, 8) Adverse Events 9) Comorbidities 10) Concise summary of main aims/objectives/study question, 11) Concise summary of main findings and conclusions, 12) settings: funding, settings/Places where interventions took place, country, conflict of interest.
In the context of meta-analysis, a systematic approach was employed to extract detailed outcome measures from the included studies. This involved standardizing treatment types and dosages to be uniformly expressed as (maintenance: previously stable participants on IVIg or SCIg, induction: treatment-naïve participants, or both), and g/kg/m, respectively. To deal with missing data, appropriate statistical analysis was conducted when only raw data was accessible using Jamovi software. Also, for data presented only in the form of bar plots, the WebPlotDigitizer tool was utilized to extract the values. Additionally, the effect measure was reported as mean and standard deviation (SD). In cases where outcome measures were presented in a different format, we calculated the mean and SD using the Meta Converter conversion tool if applicable.
Measures of treatment effect
The following outcome measurements were used in the meta-analysis:
-
For relapse rate, the proportion of patients who had a CIDP relapse during the subcutaneous treatment period excluding those who withdrew for any reason other than relapse. CIDP relapse was defined as clinical deterioration that required IVIg rescue treatment.
-
For overall function and disability assessment, Rasch-built Overall Disability Scale R-ODS, Overall Disability Sum Score ODDSs, Inflammatory Neuropathy Cause and Treatment disability score INCATd, and INCAT sensory sum for overall sensory functions assessment.
-
For muscle strength assessment, the Medical Research Council sum score MRC and Grip strength GS (measured by Martin vigorimeter or JAMAR dynamometer)
-
For functional Mobility assessment, nine-Hole-Peg Test 9-HPT and timed meter walk.
-
For patient reported outcomes, 1) patients' health-related quality of life was evaluated by the EuroQol 5 Dimension 5 level EQ5D5L index value and life quality index scale LQI, 2) health status by visual analog scale EQ-VAS, and 3) patient preference of SCIG or IVIG treatment.
-
For safety assessment, adverse events AE frequency including: local-infusion reactions, headache, severe AE, and AE leading to withdrawal.
-
serum IgG levels.
Quality assessment or risk of bias for included studies
Two researchers independently assessed the quality of each included study in accordance with tools specific to the study designs as follows:
-
Assessing the Risk of Bias for clinical trials:The risk of bias was assessed using the Cochrane Collaboration's tool for randomized trials ROB2 and the ROBINS-I tool for non-randomized studies. Assessments will be made at the study level, focusing on domains such as the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result.
-
Characteristics and Criteria for Assessment: Key characteristics assessed will include the method of randomization, treatment allocation concealment, blinding of participants and personnel, completeness of outcome data, selective reporting, and other biases. Each domain will be judged as 'low risk,' 'high risk,' or 'some concerns.'
-
Assessing quality for other study designs: CASP Checklists (Critical Appraisal Skills Programme Checklists) were employed for cohort studies and cost studies.
Strategy for data syntheses
Data synthesis combines meta-analysis for quantifiable data, with narrative synthesis providing context and insights for all findings.
Narrative Qualitative Synthesis: for studies that were unsuitable for meta-analysis, a narrative synthesis was provided. This synthesis offers a comprehensive overview by summarizing findings through:
-
Thematic Analysis: Identifying recurring themes, concepts, and patterns by coding and clustering qualitative data.
-
Synthesis of Findings: Creating a cohesive narrative that highlights key insights, trends, and implications from the collected evidence.
-
Contextualization and Interpretation: Placing the synthesized narrative within broader conceptual frameworks to interpret the relevance of findings to both practice and future research.
Meta-Analysis and Statistical Quantitative Syntheses: for data suitable for quantitative analysis, the following was employed:
We used mainly RevMan 5.3 software and in a few instances OpenMeta-analyst. Changes in continuous variables were pooled as a standardized mean difference (SMD) or mean differences (MD), depending on the specific analysis. Both fixed effects and random effects models were adopted as appropriate. Fixed effects model, which is characterized by a wider standard error, a larger weight to smaller studies, and a wider confidence interval, was used for low variability.
Visual assessment of the forest plots was used to determine heterogeneity, and the I2 and χ2 (χ2) tests to measure it. The presence of notable heterogeneity was investigated using the χ2 test, and if heterogeneity was found, it was quantified using the I2 test. The Cochrane Handbook's guidelines for meta-analysis were followed when interpreting the I2 test (0-40% = may not be significant, 30-60% = may represent moderate heterogeneity, 50-90% = may represent substantial heterogeneity, and 75-100% = significant heterogeneity).
Analysis of subgroups
Subgroup analyses were conducted to assess the differential effects of SCIG based on dosage for MRC, walk test type, and adverse events in comparison to placebo and IVIG. Dosage subgroups were categorized as low, medium, and high. Based on our standardization for dosages to be expressed as g/kg/month, we classified them as follows:
-
Low dose group: 0.87, 0.87, 1, 1, 1, 1.1, 1.15
-
Medium dose group: 1.24, 1.3, 1.3, 1.3, 1.3, 1.44, 1.5, 1.6
-
High dose group: 1.7, 1.74, 1.74, 1.74, 1.74, 1.74, 1.74
For the Timed Meter Walk Test, the 10-Meter Walk Test (10-MWT), and 40-Meter Walk Test (40-MWT) scores were analyzed separately, and as a total. Adverse events were evaluated by comparing the occurrence rates in SCIG versus placebo and SCIG versus IVIG groups.
Results
Description of studies
Results of the search
On March 1st, 2024, 2846 studies were initially identified then reduced to 1166 by search settings through the following 11 electronic databases:
Web of Science (n = 181), Scopus (n = 85), PubMed (n = 61), Google Scholar (n = 326), SpringerLink (n = 141), CENTRAL (n = 85), Europe PMC (n = 189), LILACS (n = 1), ScienceDirect (n = 64), ClinicalTrials.gov (n = 15), and ICTRP (n = 18).
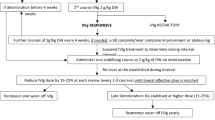
The search was updated on March 30th but yielded no extra studies for inclusion. Eventually, 50 clinical studies were included for the systematic review, and 22 of them were involved in the meta-analysis. Excluded studies were of course those that did not meet the inclusion criteria specified and detailed in the Methods section. The flow of that process is visually summarized as a flowchart. (Fig. 1).
Included studies
Included studies offer clinical data on around 1400 CIDP patients, mostly from western Europe and the US, which might represent near 10% of their entire CIDP populations. The 50 studies are 6 RCTs, 10 non-randomized clinical trials, 10 observational cohort studies, 18 case series and reports, 5 cost studies and one cross-sectional.
Tabular presentations for included studies are sufficiently provided in the supplementary material and for convenience, we included only one compact table (Table 1) for summarizing study characteristics and it contains only clinical trials.
A Compact List of brief IDs (author year) for the included studies:
Bril 2023[10], Hansen 2023 [11], Markvardsen 2023 [12], Svacina 2023 [13], Alonge 2022 [14], Ricciardi 2022 [15], Gingele 2021 [16], Kapoor 2021 [17], Murphy 2021 [18], Vu 2021 [19], Cocito 2020 [20], Gentile 2020 [21], Ryltoft 2020 [22], Cirillo 2019 [23], van Schaik 2019 [24], Cirillo 2018 [25], van Schaick 2018 [26], Christiansen 2017 [27], Cocito 2017 [28], Markvardsen 2017 [29], Markvardsen 2016 [30], Markvardsen 2016 [31], Markvardsen 2016 [32], Markvardsen 2015 [33], Cocito 2014 [34], Markvardsen 2014 [35], Markvardsen 2013 [36].
Adrichem 2017 [37], Hadden 2015 [38], Yoon 2015 [39], Lee 2008 [5], Hiya 2022 [40], Matsubayashi 2022 [41], Santilli 2021 [42], Alsolaihim 2020 [43], Marastoni 2020 [44], Cianci 2019 [45], Katzberg 2019 [46], Vacchiano 2019 [47], Rosso 2018 [48], Assenza 2016 [49], Debs 2016 [50], Nogues 2016 [51], Rosso 2014 [52], Bayas 2013 [53].
Mallick 2023 [54], Piscitelli 2021 [55], Lepage 2020 [56], Perraudin 2020 [57], Lazzaro 2014 [58].
Quality or risk of bias assessments for included studies are provided in the supplementary material. Here, we offer a visual representation regarding RCTs by ROB2 depicted as (Fig. 2).
Narrative summary of patterns and findings across studies
Considering the opportunity presented by the very large pooled sample size, we calculated the average age at disease onset and the male percentage across studies, resulting in an average age of 52 years and males being affected twice as frequently as females, which is consistent with the consensus.
Almost all studies considered SCIG to be a maintenance therapy in their context. Our analysis, though comprising multiple direct comparisons, fundamentally offers broad indirect comparisons between SCIG and IVIG, predicated on the reported facts that most patients had been previously treated with IVIG before their inclusion in the studies. Therefore, the initial disease metrics practically mirror the outcomes of IVIG treatment.
Given that SCIG is positioned as a maintenance therapy, the primary goal was to reduce relapse rates and sustain or enhance neuromuscular functions and overall ease and quality of life, with the majority of results across the various studies suggesting that SCIG not only emerges as a viable substitute but may also yield comparable or enhanced advantages in specific clinical parameters and the notable inclination towards SCIG among patients, satisfying that aim.
The majority of SCIG was Hizentra, with its manufacturer CSL Behring serving as a funding provider for many of the studies, which could partially be attributed to the high cost of human immunoglobulins in medicine. The average dose across studies and different brands was about 1.3 g/kg/month, which is equivalent to the guideline-recommended maintenance dose for CIDP using IVIG at approximately 1.44 g/kg/month [59]. SCIG doses in the studies were generally equivalent to previous IVIG doses and fall within the recommended range for maintenance therapy. Most SCIG doses align with IVIG maintenance guidelines, indicating appropriate dosing adjustments when transitioning from IVIG to SCIG. A detailed sheet for these comparisons is provided in the supplementary material.
SCIG treatments, including fSCIG (HyQvia), Gammanorm, subcuvia and Hizentra (Igpro20), have demonstrated effectiveness in reducing relapse rates and maintaining clinical stability in CIDP patients. The findings suggest that continuous, stable dosing is crucial for maintaining remission, with some patients even able to taper off SCIG treatments without triggering relapse. This indicates potential for long-term disease management strategies that emphasize personalized dosing regimens to prevent disease progression and reduce treatment dependency.
The variation in patient responses highlights the necessity of personalized treatment plans, informed by factors like disease severity and prior treatment responses. A nuanced approach to patient monitoring is vital, as it balances regular assessments to detect potential relapse with minimizing treatment burden. Innovations in treatment administration, particularly the shift towards home-based and patient-administered treatments, underscore the movement towards enhancing treatment adherence and patient satisfaction.
A shift towards patient-centered research is evident, with an increasing focus on patient-reported outcomes alongside traditional clinical measures. This reflects a broader healthcare trend towards prioritizing patient experiences of health and treatment satisfaction.
Case studies are 4 case series, 5 reports of 2 cases each, and 9 reports of single cases.
In these studies, the general patterns identified from the larger study designs largely still hold true. Even though documenting unusual reactions and adverse events is one of the roles of case reports, regardless of how seemingly not generalizable they may be, the reported adverse effects were mostly local and transient, and more tolerable compared to those associated with IVIG.
Across multiple cases, there's a significant move from Intravenous Immunoglobulin (IVIg) to SCIg due to its convenience and reduced systemic side effects.
Several note that SCIg maintains functional stability in CIDP patients with fewer fluctuations in symptoms compared to IVIg, highlighting SCIg's role in long-term management.
Some analyses discuss the economic implications of switching to SCIg, alongside improvements in quality of life. These discussions reflect a broader consideration of treatment impact beyond immediate clinical outcomes.
With SCIg, there is an emphasis on managing local injection site reactions, suggesting a need for careful patient monitoring and support. Strategies include site rotation, managing infusion rates, and adjusting SCIg dosing based on patient feedback and symptom management, and focusing on patient training for SCIg self-administration for injection and monitoring treatment response. There's an acknowledgment of the need for better tools to monitor treatment efficacy, particularly for patients managing their therapy with self-administration at home. These could include both physical symptom trackers and digital health applications.
Apropos of self-administration, Murphy et al. (2021) conducted a retrospective analysis of 310 CIDP patients transitioning from IVIG to SCIG, dedicated to this topic [18]. It examined the efficacy of the Specialty Pharmacy Nurse Network's training program, delivered in patients' homes, aimed at achieving independent management of SCIG therapy. The majority of patients needed between three and four sessions to finish, achieving a high training completion rate of 90%. Transitioning to SCIG was not only beneficial for enhancing patient autonomy and convenience but also resulted in a reduction of systemic adverse events when compared to IVIG. However, there was a minor proportion of the cohort that discontinued treatment due to adverse events, highlighting the importance of monitoring and support during the early stages of transition.
Cost studies are all relatively recent, indicating high relevancy and the avant-garde nature of the subject matter, driven by the emerging interests.
A suite of specialized studies spanning from 2014 to 2023 offers an economic and clinical evaluation of SCIG versus IVIG treatments for CIDP across various healthcare systems. These studies collectively could enhance the understanding of the budget impact, cost-effectiveness, and patient quality of life implications associated with these treatment modalities.
Mallick 2023 (USA): This budget impact model study within the US healthcare system forecasts significant savings with SCIG over IVIG, emphasizing reduced drug and non-drug costs, modeling future impacts based on current data and assumptions about treatment costs and patient outcomes. It underscores SCIG's benefits, such as self-administration, fewer adverse events, and less patient burden.
Piscitelli 2021 (Italy): Conducted through a retrospective analysis combined with a budget impact analysis, this study is an outlier that reports higher costs for SCIG compared to IVIG. Despite these higher costs, SCIG demonstrated significant safety benefits and enhancements in patient quality of life.
Perraudin 2020 (Switzerland): It Integrates model-based cost-minimization analysis with both retrospective patient data and prospective cost estimations. It suggests SCIG as a more cost-effective alternative from a societal perspective, primarily due to lower total costs for health insurance and other payers.
Lepage 2020 (France): From the French Social Security perspective, this budget impact model predicts a 10% decrease in total annual costs per patient when switching from IVIG to SCIG over five years. It promotes SCIG as a cost-saving option that could substantially reduce hospital visits and overall treatment expenses.
Lazzaro 2014 (Italy): Conducting a cost-minimization analysis, it supports the economic benefits of SCIG over IVIG from a societal perspective, highlighting minimal annual savings favoring SCIG.
Across these diverse healthcare contexts, SCIG emerges as a generally more cost-effective treatment compared to IVIG, mainly due to its potential for reducing overall healthcare costs, including drug and non-drug related expenses. However, the Piscitelli 2021 study presents an important counterpoint by highlighting a scenario where SCIG was more expensive, which emphasizes the variability in cost-effectiveness depending on specific national healthcare system prices and patient management practices.
The studies underline similar clinical outcomes between SCIG and IVIG, suggesting that treatment decisions may be influenced more by economic considerations and patient preferences, particularly regarding quality of life. SCIG’s advantages in terms of self-administration and reduced adverse events are consistently recognized as factors that could lead to improved patient satisfaction and adherence, showing a general trend towards the cost-effectiveness and patient-centered benefits of SCIG balancing clinical efficacy with economic and quality of life considerations, especially when considering long-term treatment.
Meta-analysis
Meta-analysis showed SCIG significantly improved muscle strength and sensory function, had fewer and milder side effects, reduced relapse rates, and received a strong preference. These results are illustrated in Figures 3, 4, 5, 6, 7, 8, 9, and 10.
Muscle Strength (Medical Research Council Scale, MRC): Analysis incorporating data from 18 studies with a combined participant pool of 542 individuals demonstrated a significant improvement in muscle strength post-SCIG treatment. The pooled standardized mean difference (SMD) in MRC scores was 0.68 points (95% CI: 0.28 to 1.08), with statistically significant enhancement (p = 0.0008). Heterogeneity among studies was high (I2 = 88%)
MRC Subgroup Analysis by Dose: Subgroups were divided by dose as low, medium, and high. The low dose subgroup shows no significant effect (SMD -0.05, 95% CI [-0.22, 0.14]). The medium dose subgroup shows a small but not statistically significant effect (SMD 0.18, 95% CI [-0.04, 0.40]). The high dose subgroup shows a significant effect (SMD 2.39, 95% CI [0.79, 3.98]) and high heterogeneity (I2 = 95%)
INCAT Sensory Score: Our analysis of 5 studies, including 67 participants, revealed a significant improvement in sensory function as measured by the INCAT Sensory Score. The pooled mean difference (MD) showed a reduction of 1.73 points (95% CI: -2.29 to -1.17), which was statistically significant (p < 0.00001). This improvement indicates enhanced sensory function following SCIG therapy, there was high heterogeneity (I2 = 92%) among the included studies
Side Effects Analysis: SCIG vs. IVIG: Overall Side Effects: From 4 studies (202 patients), side effects were less likely with SCIG, showing a significant pooled OR of 0.22 (95% CI: 0.12 to 0.40, p < 0.0001). Heterogeneity was insignificant (I2 = 17%) Headache: Analysis from 2 studies (202 patients) found significant difference in headache occurrence in SCIG group, OR = 0.14 (95% CI: 0.07 to 0.30, p < 0.0001) Infusion Site Reactions: Not significantly more common with SCIG in 2 studies (104 patients), with an OR of 1.75 (p = 0.50). No heterogeneity (I2 = 0%) Severe Side Effects: No significant differences were found in severe side effects (OR = 0.23, p = 0.19) across 2 studies (104 patients)
Further Meta-Analysis
The figures representing the meta-analyses of Quality of Life Measures, EQ-VAS, Timed Meter Walk Test, 9-HPT, Side Effects Analysis SCIG vs. Placebo, ODSS, IRODS, INCAT, Grip Strength, and IgG levels are provided in the supplementary materials.
Discussion
This comprehensive Systematic Review and Meta-Analysis aimed to evaluate the efficacy, safety, and convenience of subcutaneous immunoglobulin (SCIG) in the maintenance treatment of Chronic Inflammatory Demyelinating Polyneuropathy (CIDP), covering a broad range of dimensions and outcomes, including relapse rate, overall function and disability, muscle strength, sensory function, serum IgG levels, quality of life, adverse events, patient treatment preferences, and economic implications.
To our knowledge, this can be considered the first systematic review or meta-analysis dedicated specifically to this particular topic, at least within accessible or peer-reviewed sources. The closest related meta-analysis is an older one by Racosta et al., comparing SCIG with intravenous immunoglobulin (IVIG) for chronic autoimmune neuropathies [60]; however, it is both less specific to our focus and less comprehensive, and it predates the main bulk of the current literature. Nonetheless, some of their findings align with ours in direction.
For this project, we compiled 50 clinical studies from 11 databases, 50 for the narrative syntheses, and 22 for the statistical syntheses.
Summary of key findings and their integration with existing literature
Since SCIG is considered a maintenance therapy after stabilizing on IVIG [61], the primary objective is to avoid a recurrence and maintain or uphold neuromuscular function and overall quality of life [10]. Interestingly, our meta-analysis met the desired goal of SCIg treatment, showing that the relapse rate was relatively acceptable, and all the assessed efficacy outcomes were either maintained or improved.
In comparison to the conventional IVIG treatment, a previous 52-week open-label study found that IVIG administered as maintenance therapy had a relapse rate of 10.5% [62], similar to the results of high-dose SCIG treatment in the 48-week open-label PATH extension trial RR 10.8% [24]. Our results of 14.6% RR relate to these findings, indicating that both IVIG and SCIG might have comparable efficacy in terms of relapse rates.
In brief, the most important efficacy assessment outcome measures in CIDP include the INCATd scale and the R-ODS scale for disability, in addition to grip strength and the MRC sum score for muscle strength [63,64,65]. Analysis of these scores did not show any deterioration during the SCIg treatment compared to IVIG stabilized baseline, compatible with the prior Meta-analysis conclusion, noting that it assessed only the MRC sum score [60].
MRC's Initial meta-analysis results indicated a significant improvement in MRC scale scores post-SCIG treatment. Sensitivity analysis, however, revealed a non-significant effect, necessitating further examination through subgroup analysis. This analysis demonstrated a dose–response relationship, where higher SCIG doses correlated with significant improvements in MRC scores. However, a direct comparison between low and high doses in the PATH study did not reveal a discernible superiority of high-dose SCIg in MRC scores [26].
Furthermore, sensory impairment is considered one of the main hallmarks of CIDP and can be evaluated by the INCATss scale [66, 67]. Our findings demonstrated a statistically significant improvement in this scale, in favor of SCIg treatment even after sensitivity analysis, however, the studies that reported this outcome were not of high quality. For impaired functional mobility, no worsening was observed in the analysis of 9-HPT and timed meter walk test scores, indicating that patients preserved their functional mobility upon SCIG maintenance treatment.
The present analysis reveals that SCIG is associated with a 22% decreased risk of adverse events compared to IVIG. This observation is relatable to previous research, including Racosta's meta-analysis that noted a 28% reduction in the risk of moderate and systemic adverse events with SCIG versus IVIG [60]. Additionally, studies by Farmakidis et al. and Allen et al. support our findings, suggesting that SCIG leads to fewer adverse events relative to IVIg. This advantage is attributed to the slower absorption into the bloodstream with SCIG, which avoids the high peak levels of Immunoglobulin G (IgG) seen after IVIG administrations [8, 68].
Findings also showed that quality of life and health status remained stable after treatment with SCIG, which is consistent with IVIG treatments. This supports earlier research by Rajabally et al., which found that SCIg either improved or matched the outcomes of IVIg in treating CIDP [69]. It is worth noting that quality of life (QoL) is likely affected by the efficacy of immunoglobulin therapy [70], and since our analysis showed similar efficacy of SCIg and IVIg, stable QoL measures could be justified, especially when using general QoL scales like EQ-5D. Interestingly, two included studies that used a more IgG treatment oriented scale like LQI that considers many items related to patients' convenience, comfort, and independence according to the IgG route of administration [71], showed better QoL measures after SCIg. A previous pooled analysis of QoL in patients with Primary Immunodeficiency treated with Hizentra, an SCIG, may have reflected this by showing significant improvements in all LQI domain scores [72].
Patients' treatment preferences, when analyzed, unanimously demonstrated a preference for SCIG across all studies. This includes, among others, probably the two largest studies in the field: PATH [26] and ADVANCE-CIDP1[10]. Studies that numerically reported a preference for SCIG over IVIG, depicted in Fig. 10, all have a mean age older than 55 years, with an overall weighted mean age of 57.
Treatment Preference: Analyzing data from 6 studies with 304 participants, there was a significant preference for SCIG over alternative treatments. The pooled Risk ratio (RR) was 0.52, with a 95% CI of 0.37 to 0.67, indicating a statistically significant preference (p < 0.0001). Heterogeneity was high (I2 = 81%)
Unsurprisingly, this finding is in agreement with a previous systematic review on the burden of illness in CIDP by Querol et al., [73], as well as a literature review by Goyal et al.,[7]. Querol et al., highlights that 53–88% of patients favor SCIG over IVIG for its ease, flexibility, stability, and fewer side effects, also noting its time efficiency. Goyal et al., confirms a similar preference for SCIG among CIDP patients, attributing it to home administration convenience, lower volumes, fewer AEs, and fewer fluctuations.
An intriguing historical report notes that the initial application of immunoglobulin therapy for immune disorders commenced with subcutaneous administration in 1952, so it might after all come to what Wasserman elegantly phrased in a title of his, “from subcutaneous to intravenous infusions and back again” [74, 75].
The economic evaluations integrated into our analysis reveal that SCIG generally presents as a more cost-effective option, particularly when considering long-term treatment. These evaluations, conducted across various healthcare systems, indicate potential cost savings associated with SCIG, primarily attributed to reductions in hospitalization, administration costs, and the management of adverse events. These findings align with the broader trend towards home-based and patient-centered care models, suggesting that the adoption of SCIG should be considered within the specific context of each healthcare system.
Strengths, limitations, and future research recommendations
This work offers a thorough and organized presentation and analysis of most available data, providing strong evidence supporting the use of SCIG for CIDP. Given CIDP's rarity, incorporating data from all available study designs is a notable strength, maximizing the use of limited information for a better understanding and management of this condition. However, the analysis encountered some limitations, especially in accessing specific raw data, despite reaching out to researchers. This brings to mind the broader issue of data transparency in scientific research and the call for future work to push for more open data sharing for richer analyses. Additionally, given the heterogeneity in certain outcomes and the partial reliance on predominantly indirect SCIG versus IVIG comparisons, a cautious interpretation of the findings is recommended.
Some kind of paradox emerged in Bril 2023, for example, when a seemingly synonymous or related group of constructs displayed some degree of divergence. Namely, in one study, the compound scale Treatment Satisfaction Questionnaire for Medication (TSQM) scores suggested some decrease in treatment satisfaction, yet the same patients from the same study reported simply an increased satisfaction and also separately a clear preference for SCIG treatment, while concurrently showing no significant change in health-related quality of life scales. This situation, observed in Bril 2023 and van Schaick 2018, highlights the complexity of interpreting patient-reported outcome measures (PROMs). Despite seemingly contradictory results, these instances reveal the nuanced nature of patient preferences and experiences in chronic disease management.
The analysis of economic outcomes, limited to countries with somewhat similar economic systems, further emphasizes the need for careful consideration when generalizing these results to different contexts.
Future research should focus on longitudinal studies comparing SCIG and IVIG as CIDP maintenance treatments to identify predictors of successful treatment transitions. Whenever possible, they should also refine inclusion criteria, grouping and outcome measures within individual studies to precisely differentiate between typical and atypical CIDP subtypes and other related conditions like MMN, enhancing inferential capacity and accessibility. Expanding economic impact studies of these therapies across diverse economies is also essential.
It is also advisable for some future research lines and guidelines to consider giving more weight to specialized physiotherapy for CIDP maintenance. Although not yet well-documented in the literature and not our focus here, practical experience suggests it could be of pivotal importance in sustaining remission and perhaps could be considered as an add-on to SCIG for an increased, additive, or even synergistic benefit.
Furthermore, exploring the Facilitated SCIG (FSCIG), which holds the potential to combine the main advantages of SCIG and IVIG, presents a promising research direction that could significantly impact CIDP treatment strategies. The increasing capability of SCIG to administer larger doses of immunoglobulins could indicate its potential for use in CIDP induction therapy in the future [76].
Conclusion
The findings suggest that SCIG for CIDP maintenance not only provides a more feasible alternative, with economic evaluations showing considerable cost reductions over time and patient preference for SCIG being pronounced, but may also deliver comparable or superior health outcomes.
A patient-focused strategy in handling CIDP, guided by robust evidence and economic considerations, aiming for optimal patient outcomes and satisfaction, shall highlight the importance of SCIG for those suited to it.
Ongoing research lines on formulations, techniques, and direct comparative studies are critical to further illuminate, enhance, and expand SCIG's role in treatment, ensuring medical practices are equipped with optimal tools, informed by comprehensive evidence, are cost-effective, and probably most importantly, aligned with patient preferences and convenience.
Data availability
Provided in the supplementary material.
References:
Lehmann HC, Burke D, Kuwabara S (2019) Chronic inflammatory demyelinating polyneuropathy: update on diagnosis, immunopathogenesis and treatment. J Neurol Neurosurg Psychiatry 90(9):981–987. https://doi.org/10.1136/jnnp-2019-320314
Gorson KC (2012) An update on the management of chronic inflammatory demyelinating polyneuropathy. Ther Adv Neurol Disord 5(6):359–373. https://doi.org/10.1177/1756285612457215
Dyck PJ et al (1975) Chronic inflammatory polyradiculoneuropathy. Mayo Clin Proc 50(11):621–637
Albala M et al (1987) Improvement of neurologic function in chronic inflammatory demyelinating polyradiculoneuropathy following intravenous gamma-globulin infusion. Arch Neurol 44(3):248–249
Lee DH et al (2008) Subcutaneous immunoglobulin infusion: a new therapeutic option in chronic inflammatory demyelinating polyneuropathy. Muscle Nerve 37(3):406–409. https://doi.org/10.1002/mus.20909
Hughes RA et al (2009) Clinical applications of intravenous immunoglobulins in neurology. Clin Exp Immunol 158(Suppl 1):34–42. https://doi.org/10.1111/j.1365-2249.2009.04025.x
Goyal NA et al (2021) Subcutaneous immunoglobulin treatment for chronic inflammatory demyelinating polyneuropathy. Muscle Nerve 64(3):243–254. https://doi.org/10.1002/mus.27356
Allen JA et al (2020) Immunoglobulin administration for the treatment of CIDP: IVIG or SCIG? J Neurol Sci 408:116497. https://doi.org/10.1016/j.jns.2019.116497
Dimachkie MM (2022) Optimizing chronic inflammatory demyelinating polyneuropathy care with subcutaneous immunoglobulin: The Polyneuropathy and Treatment with Hizentra Open-Label Extension (PATH OLE) study and beyond. RRNMF Neuromusc J 3(2):13–26. https://doi.org/10.17161/rrnmf.v3i2.16304
Bril V et al (2023) Hyaluronidase-facilitated subcutaneous immunoglobulin 10% as maintenance therapy for chronic inflammatory demyelinating polyradiculoneuropathy: The ADVANCE-CIDP 1 randomized controlled trial. J Peripher Nerv Syst 28(3):436–449. https://doi.org/10.1111/jns.12573
Hansen PN et al (2023) Changes in axonal and clinical function during intravenous and subcutaneous immunoglobulin therapy in chronic inflammatory demyelinating polyneuropathy. J Peripher Nerv Syst 28(3):425–435. https://doi.org/10.1111/jns.12563
Markvardsen LK et al (2023) Standardized Tapering off Subcutaneous Immunoglobulin in Chronic Inflammatory Demyelinating Polyneuropathy. J Neuromuscul Dis 10(5):787–796. https://doi.org/10.3233/JND-221615
Svacina MKR et al (2024) Immunomodulatory effects of intravenous and subcutaneous immunoglobulin in chronic inflammatory demyelinating polyneuropathy: An observational study. Eur J Neurol 31(1):e16079. https://doi.org/10.1111/ene.16079
Alonge P et al (2022) Clinical and Neurophysiological Follow-Up of Chronic Inflammatory Demyelinating Polyneuropathy Patients Treated with Subcutaneous Immunoglobulins: A Real-Life Single Center Study. Brain Sci 13(1):10. https://doi.org/10.3390/brainsci13010010
Ricciardi D et al (2022) Neurophysiological Hallmarks of Axonal Degeneration in CIDP Patients: A Pilot Analysis. Brain Sci 12(11):1510. https://doi.org/10.3390/brainsci12111510
Gingele S et al (2021) Switch from intravenous to subcutaneous immunoglobulin IgPro20 in CIDP patients: a prospective observational study under real-world conditions. Ther Adv Neurol Disord 14:17562864211009100. https://doi.org/10.1177/17562864211009100
Kapoor M et al (2021) Subcutaneous immunoglobulin dose titration to clinical response in inflammatory neuropathy. J Neurol 268(4):1485–1490. https://doi.org/10.1007/s00415-020-10318-3
Murphy E et al (2021) Infusion Parameters and Demographics of Patients With Chronic Inflammatory Demyelinating Polyneuropathy During Subcutaneous Immunoglobulin Self-Administration Training. J Infus Nurs 44:289–297. https://doi.org/10.1097/NAN.0000000000000441
Vu T et al (2021) Impact of subcutaneous immunoglobulin on quality of life in patients with chronic inflammatory demyelinating polyneuropathy previously treated with intravenous immunoglobulin. Muscle Nerve 64(3):351–357. https://doi.org/10.1002/mus.27345
Cocito D et al (2020) Manual push technique, an alternative route of subcutaneous immunoglobulin administration in chronic inflammatory demyelinating polyradiculoneuropathy: A proof-of-concept study. Clin Neurol Neurosurg 198:106240. https://doi.org/10.1016/j.clineuro.2020.106240
Gentile L et al (2020) Long-term treatment with subcutaneous immunoglobulin in patients with chronic inflammatory demyelinating polyradiculoneuropathy: a follow-up period up to 7 years. Sci Rep 10(1):7910. https://doi.org/10.1038/s41598-020-64699-6
Ryltoft AK et al (2020) Quality of life in chronic inflammatory demyelinating polyneuropathy patients treated with subcutaneous immunoglobulin. Acta Neurol Scand 142(6):637–640. https://doi.org/10.1111/ane.13322
Cirillo G et al (2019) Clinical-neurophysiological correlations in chronic inflammatory demyelinating polyradiculoneuropathy patients treated with subcutaneous immunoglobulin. Muscle Nerve 60(6):662–667. https://doi.org/10.1002/mus.26669
van Schaik IN et al (2019) Long-term safety and efficacy of subcutaneous immunoglobulin IgPro20 in CIDP: PATH extension study. Neurol Neuroimmunol Neuroinflamm 6(5):e590. https://doi.org/10.1212/NXI.0000000000000590
Cirillo G, Todisco V, Tedeschi G (2018) Long-term neurophysiological and clinical response in patients with chronic inflammatory demyelinating polyradiculoneuropathy treated with subcutaneous immunoglobulin. Clin Neurophysiol 129(5):967–973. https://doi.org/10.1016/j.clinph.2018.01.070
van Schaik IN et al (2018) Subcutaneous immunoglobulin for maintenance treatment in chronic inflammatory demyelinating polyneuropathy (PATH): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol 17(1):35–46. https://doi.org/10.1016/S1474-4422(17)30378-2
Christiansen I, Markvardsen LH, Jakobsen J (2018) Comparisons in fluctuation of muscle strength and function in patients with immune-mediated neuropathy treated with intravenous versus subcutaneous immunoglobulin. Muscle Nerve 57(4):610–614. https://doi.org/10.1002/mus.25967
Cocito D et al (2017) Subcutaneous “bolus” immunoglobulin dose in CIDP: A proof-of concept study. J Neurol Sci 380:54–57. https://doi.org/10.1016/j.jns.2017.07.003
Markvardsen LH et al (2018) Resistance training and aerobic training improve muscle strength and aerobic capacity in chronic inflammatory demyelinating polyneuropathy. Muscle Nerve 57(1):70–76. https://doi.org/10.1002/mus.25652
Markvardsen LH et al (2017) Subcutaneous immunoglobulin as first-line therapy in treatment-naive patients with chronic inflammatory demyelinating polyneuropathy: randomized controlled trial study. Eur J Neurol 24(2):412–418. https://doi.org/10.1111/ene.13218
Markvardsen LH, Christiansen I, Jakobsen J (2016) Improvement of hemoglobin levels after a switch from intravenous to subcutaneous administration of immunoglobulin in chronic inflammatory demyelinating polyneuropathy and multifocal motor neuropathy. Transfusion 56(10):2443–2448. https://doi.org/10.1111/trf.13727
Markvardsen LH et al (2016) Diffusion tensor imaging can be used to detect lesions in peripheral nerves in patients with chronic inflammatory demyelinating polyneuropathy treated with subcutaneous immunoglobulin. Neuroradiology 58(8):745–752. https://doi.org/10.1007/s00234-016-1692-z
Markvardsen LH et al (2015) Headache and Nausea after Treatment with High-Dose Subcutaneous versus Intravenous Immunoglobulin. Basic Clin Pharmacol Toxicol 117(6):409–412. https://doi.org/10.1111/bcpt.12428
Cocito D et al (2014) Subcutaneous immunoglobulin in CIDP and MMN: a short-term nationwide study. J Neurol 261(11):2159–2164. https://doi.org/10.1007/s00415-014-7444-2
Markvardsen LH et al (2014) Subcutaneous immunoglobulin preserves muscle strength in chronic inflammatory demyelinating polyneuropathy. Eur J Neurol 21(12):1465–1470. https://doi.org/10.1111/ene.12513
Markvardsen LH et al (2013) Subcutaneous immunoglobulin in responders to intravenous therapy with chronic inflammatory demyelinating polyradiculoneuropathy. Eur J Neurol 20(5):836–842. https://doi.org/10.1111/ene.12080
Adrichem ME et al (2017) Drug-induced cutaneous lupus erythematosus after immunoglobulin treatment in chronic inflammatory demyelinating polyneuropathy: a case series. J Peripher Nerv Syst 22(3):213–218. https://doi.org/10.1111/jns.12218
Hadden RD, Marreno F (2015) Switch from intravenous to subcutaneous immunoglobulin in CIDP and MMN: improved tolerability and patient satisfaction. Ther Adv Neurol Disord 8(1):14–19. https://doi.org/10.1177/1756285614563056
Yoon MS, Gold R, Kerasnoudis A (2015) Subcutaneous immunoglobulin in treating inflammatory neuromuscular disorders. Ther Adv Neurol Disord 8(4):153–159. https://doi.org/10.1177/1756285615584739
Hiya S et al (2022) High-dose immunoglobulin-dependent chronic demyelinating inflammatory polyneuropathy successfully managed with subcutaneous immunoglobulin using pharmacokinetic analysis. eNeurologicalSci 27:100404. https://doi.org/10.1016/j.ensci.2022.100404
Matsubayashi Tomo et al (2022) Experience with the use of subcutaneous immunoglobulin preparations for chronic inflammatory demyelinating polyneuritis in children. Brain Dev 54(2):132–134. https://doi.org/10.11251/ojjscn.54.132
Santilli AR, Wieland ML (2021) Falsely Elevated Creatinine on Enzymatic Assay in a Patient Receiving Subcutaneous IgG Therapy. J Gen Intern Med 36(5):1427–1428. https://doi.org/10.1007/s11606-021-06631-w
Alsolaihim A, Baker SK (2020) Dose Adjustment of Subcutaneous IgG in Chronic Inflammatory Demyelinating Polyneuropathy. Case Rep Neurol 12(1):73–77. https://doi.org/10.1159/000505320
Marastoni D et al (2020) Sustained response to subcutaneous immunoglobulins in chronic ataxic neuropathy with anti-disialosyl IgM antibodies (CANDA): report of two cases and review of the literature. J Neurol 267:2353–2361. https://doi.org/10.1007/s00415-020-09843-y
Cianci P et al (2019) Subcutaneous Immunoglobulin in Infantile Chronic Inflammatory Demyelinating Polyneuropathy: A Case Report. J Pediatr Neurosci 14(1):38–41. https://doi.org/10.4103/jpn.JPN_132_18
Katzberg H et al (2019) Subcutaneous Immunoglobulin in Chronic Inflammatory Demyelinating Polyneuropathy–Neurologist, Nursing and Patient Perspectives. Eur Neurol Rev 14: 44. https://doi.org/10.17925/ENR.2019.14.1.44
Vacchiano V et al (2019) Subcutaneous immunoglobulin treatment and leucopenia in acquired demyelinating peripheral neuropathies. Eur J Neurol 26(9):e80–e81. https://doi.org/10.1111/ene.13933
Rosso T (2018) Cutaneous adverse effects after intravenous and subcutaneous immunoglobulin therapy for multifocal motor neuropahty and chronic inflammatory demielinating polineuropathy: 2 case reports. J Peripher Nerv Syst 23 (Suppl 1):S37. https://doi.org/10.1111/jns.12255
Assenza G et al (2016) 49. Effectiveness of subcutaneous immunoglobulins in paraneoplastic CIDP caused by signet ring cell adenocarcinoma. Clin Neurophysiol 127(12): e335. https://doi.org/10.1016/j.clinph.2016.10.061
Debs R et al (2017) A new treatment regimen with high-dose and fractioned immunoglobulin in a special subgroup of severe and dependent CIDP patients. Int J Neurosci 127(10):864–872. https://doi.org/10.1080/00207454.2016.1269328
Nogues MA et al (2016) Subcutaneous immunoglobulin. Treatment in chronic inflammatory demyelinating polyradiculo-neuropathy. Medicina (B Aires) 76(1):36–39
Rosso T (2014) Severe cutaneous adverse effect in a patient affected by CIDP treated with hizentra. J Peripher Nerv Syst 19(Suppl 1):S29–S30. https://doi.org/10.1111/jns5.12058
Bayas A, Gold R, Naumann M (2013) Long-term treatment of Lewis-Sumner syndrome with subcutaneous immunoglobulin infusions. J Neurol Sci 324(1–2):53–56. https://doi.org/10.1016/j.jns.2012.09.033
Mallick R, Carlton R, Van Stiphout J (2023) A Budget Impact Model of Maintenance Treatment of Chronic Inflammatory Demyelinating Polyneuropathy with IgPro20 (Hizentra) Relative to Intravenous Immunoglobulin in the United States. Pharmacoecon Open 7(2):243–255. https://doi.org/10.1007/s41669-023-00386-2
Piscitelli E et al (2021) Economic evaluation of subcutaneous versus intravenous immunoglobulin therapy in chronic inflammatory demyelinating polyneuropathy: a real-life study. Eur J Hosp Pharm 28(Suppl 2):e115–e119. https://doi.org/10.1136/ejhpharm-2020-002430
Lepage V, Moumane N, Matheron A (2020) PRO47 Budget IMPACT MODEL of Subcutaneous Immunoglobulins in the Treatment of Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) in France. Value Health 23:S698. https://doi.org/10.1016/j.jval.2020.08.1783
Perraudin C et al (2020) Home-based subcutaneous immunoglobulin for chronic inflammatory demyelinating polyneuropathy patients: A Swiss cost-minimization analysis. PLoS ONE 15(11):e0242630. https://doi.org/10.1371/journal.pone.0242630
Lazzaro C, Lopiano L, Cocito D (2014) Subcutaneous vs intravenous administration of immunoglobulin in chronic inflammatory demyelinating polyneuropathy: an Italian cost-minimization analysis. Neurol Sci 35(7):1023–1034. https://doi.org/10.1007/s10072-014-1632-9
Van den Bergh PY et al (2010) European Federation of Neurological Societies/Peripheral Nerve Society guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society - first revision. Eur J Neurol 17(3):356–363. https://doi.org/10.1111/j.1468-1331.2009.02930.x
Racosta JM, Sposato LA, Kimpinski K (2017) Subcutaneous versus intravenous immunoglobulin for chronic autoimmune neuropathies: A meta-analysis. Muscle Nerve 55(6):802–809. https://doi.org/10.1002/mus.25409
Van den Bergh PYK et al (2021) European Academy of Neurology/Peripheral Nerve Society guideline on diagnosis and treatment of chronic inflammatory demyelinating polyradiculoneuropathy: Report of a joint Task Force-Second revision. J Peripher Nerv Syst 26(3):242–268. https://doi.org/10.1111/jns.12455
Kuwabara S et al (2017) Intravenous immunoglobulin for maintenance treatment of chronic inflammatory demyelinating polyneuropathy: a multicentre, open-label, 52-week phase III trial. J Neurol Neurosurg Psychiatry 88(10):832–838. https://doi.org/10.1136/jnnp-2017-316427
Allen JA, Merkies ISJ, Lewis RA (2020) Monitoring Clinical Course and Treatment Response in Chronic Inflammatory Demyelinating Polyneuropathy During Routine Care: A Review of Clinical and Laboratory Assessment Measures. JAMA Neurol 77(9):1159–1166. https://doi.org/10.1001/jamaneurol.2020.0781
Vanhoutte EK et al (2013) 196th ENMC international workshop: Outcome measures in inflammatory peripheral neuropathies 8–10 February 2013, Naarden, The Netherlands. Neuromuscul Disord 23(11):924–933. https://doi.org/10.1016/j.nmd.2013.06.006
van Veen R et al (2022) Assessing deterioration using impairment and functional outcome measures in chronic inflammatory demyelinating polyneuropathy: A post-hoc analysis of the immunoglobulin overtreatment in CIDP trial. J Peripher Nerv Syst 27(2):144–158. https://doi.org/10.1111/jns.12497
Hu J et al (2022) Efficacy of rituximab treatment in chronic inflammatory demyelinating polyradiculoneuropathy: a systematic review and meta-analysis. J Neurol 269(3):1250–1263. https://doi.org/10.1007/s00415-021-10646-y
Merkies IS et al (2000) Psychometric evaluation of a new sensory scale in immune-mediated polyneuropathies. Inflammatory Neuropathy Cause and Treatment (INCAT) Group. Neurology 54(4):943–949. https://doi.org/10.1212/WNL.54.4.943
Farmakidis C et al (2020) Immunosuppressive and immunomodulatory therapies for neuromuscular diseases. Part II: New and novel agents. Muscle Nerve 61(1):17–25. https://doi.org/10.1002/mus.26711
Rajabally YA, Cavanna AE (2015) Health-related quality of life in chronic inflammatory neuropathies: a systematic review. J Neurol Sci 348(1–2):18–23. https://doi.org/10.1016/j.jns.2014.11.005
Markvardsen LH, Harbo T (2017) Subcutaneous immunoglobulin treatment in CIDP and MMN. Efficacy, treatment satisfaction and costs. J Neurol Sci 378:19–25. https://doi.org/10.1016/j.jns.2017.04.039
Daly PB et al (1991) Home-based immunoglobulin infusion therapy: quality of life and patient health perceptions. Ann Allergy 67(5):504–510
Mallick R et al (2018) Treatment Satisfaction with Subcutaneous Immunoglobulin Replacement Therapy in Patients with Primary Immunodeficiency: a Pooled Analysis of Six Hizentra(R) Studies. J Clin Immunol 38(8):886–897. https://doi.org/10.1007/s10875-018-0562-3
Querol L et al (2021) Systematic literature review of burden of illness in chronic inflammatory demyelinating polyneuropathy (CIDP). J Neurol 268(10):3706–3716. https://doi.org/10.1007/s00415-020-09998-8
Bruton OC (1952) Agammaglobulinemia. Pediatrics 9(6):722–728
Wasserman RL (2012) Progress in gammaglobulin therapy for immunodeficiency: from subcutaneous to intravenous infusions and back again. J Clin Immunol 32(6):1153–1164. https://doi.org/10.1007/s10875-012-9740-x
Locke KW, Maneval DC, LaBarre MJ (2019) ENHANZE((R)) drug delivery technology: a novel approach to subcutaneous administration using recombinant human hyaluronidase PH20. Drug Deliv 26(1):98–106. https://doi.org/10.1080/10717544.2018.1551442
Acknowledgements
The following are acknowledged for contributions:
Mufreh Amin (0009-0001-8882-5116), Mahmoud Samir (0009-0008-9338-6366), Roaa Haddad (0009-0001-3850-1295), Nada Gamal (0009-0000-0212-2982), Ahmed Nada (0000-0003-0649-6310), Ahmed
Beddor (0009-0008-4212-2424), Asmaa Alnjjar (0000-0002-1254-4289), Aya Sharkawy (0000-0001-6183-6563), Rovan Ahmed
Rouby (0009-0001-0326-9297), Zahraa Bhaya (0009-0004-1700-5462), Zeinab Natsheh (0009-0001-0763-9371), Mohammed
Yasser (0009-0000-3696-1215), Ruaa Qafesha (0000-0002-8745-0260), Ahmed Negida (0000-0001-5363-6369)
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
AR: Conceptualization, organization, contributions at all stages, and drafting the majority of the manuscript.
SM: Significant contributions at all stages and participation in manuscript preparation.
NB: Significant contributions at all stages and participation in manuscript preparation.
HS, AS, MRR, GA, SS, AK: Conducted study selection, data extraction, and quality assessment for several studies.
IS: Made a major contribution to the statistical synthesis.
MRS: Performed methodological and linguistic revisions of the manuscript, designed a specialized data extraction. form for cost studies, conducted initial data extraction for cost studies, and presented their results.
Corresponding author
Ethics declarations
Competing interests
All authors and contributors have no competing interests to declare that are relevant to the subject matter discussed within this article.
Ethics approval or consent
Not Applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramzi, A., Maya, S., Balousha, N. et al. Subcutaneous immunoglobulins (SCIG) for chronic inflammatory demyelinating polyneuropathy (CIDP): A comprehensive systematic review of clinical studies and meta-analysis. Neurol Sci (2024). https://doi.org/10.1007/s10072-024-07640-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10072-024-07640-3