Abstract
Background
Sexual dysfunction (SD) is a frequent non-motor symptom in Parkinson’s disease (PD) that is rarely addressed, and sexual counseling is sporadic.
Objectives
To investigate PD patients’ SD and sexual counseling motivation and to propose an interventional strategy for movement disorder specialists.
Methods
All consecutive PD patients who presented to a movement disorder unit between 2018 and 2019 completed anonymous questionnaires containing the Female Sexual Function Index, the International Index of Erectile Function, and a questionnaire on sexual needs and motivation to receive sexual counseling.
Results
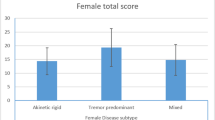
The age range of the 100 recruited patients (78 men) was 40–80 years, and the mean disease duration was 8.64 ± 6.84 years. SD appeared at all PD stages. The presence of SD pre-PD diagnosis significantly predicted SD post-diagnosis in men. Erectile dysfunction was the most common male SD (70%). Women reported frequent SD before PD diagnosis and currently. More than half of the responders (74% of the men and 40% of the women) were motivated to receive sexual counseling. Most of them (77.4%) were in a relationship.
Conclusions
The findings of this analysis revealed that most PD patients had experienced SD before being diagnosed with PD and were interested in receiving sexual counseling. We propose a six-step intervention strategy for the management of SD in PD designed for application in a movement disorder unit. We also recommend that neurologists and other healthcare providers undergo training to provide basic sexual counseling tailored to the needs of PD patients.
Similar content being viewed by others
References
Lees AJ, Hardy J, Revesz T (2009) Parkinson’s disease. Lancet 373:2055–2066
Seppi K, Weintraub D, Coelho M et al (2011) The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov disord 26:S42-80
Chaudhuri KR, Healy DG, Schapira AH (2006) Non-motor symptoms of Parkinson’s disease: diagnosis and management. Lancet Neurol 5:235–245
Giladi N, Manor Y, Hilel A et al (2014) Interdisciplinary teamwork for the treatment of people with Parkinson’s disease and their families. Curr Neurol Neurosci Rep 14:493
Vela-Desojo L, Urso D, Kurtis-Urra M et al (2020) Sexual dysfunction in early-onset Parkinson’s disease: a cross-sectional, multicenter study. J Parkinsons Dis 10:1621–1629
Basson R, Rees P, Wang R et al (2010) Sexual function in chronic illness. J Sex Med 7:374–438
Bronner G, Royter V, Korczyn AD et al (2004) Sexual dysfunction in Parkinson’s disease. J Sex Marital Ther 30:95–105
Buhmann C, Dogac S, Vettorazzi E et al (2017) The impact of Parkinson’s disease on patients’ sexuality and relationship. J Neural Transm (Vienna) 128:983–996
Dyer K, das Nair R (2013) Why don’t healthcare professionals talk about sex? A systematic review of recent qualitative studies conducted in the United Kingdom. J Sex Med 10:2658–2670
Bhattacharyya KB, Rosa-Grilo M (2017) Sexual dysfunctions in Parkinson’s disease: an underrated problem in a much discussed disorder. Int Rev Neurobiol 134:859–876
Politis M, Wu K, Molloy S et al (2010) Parkinson’s disease symptoms: the patient’s perspective. Mov Disord 25:1646–1651
Lindau ST, Schumm LP, Laumann EO et al (2007) A study of sexuality and health among older adults in the United States. N Engl J Med 357:762–774
Gott M, Hinchliff S, Galena E (2004) General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med 58:2093–2103
Postuma RB, Berg D, Stern M et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601
Rosen RC, Brown C, Heiman J et al (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
Rosen RC, Riley A, Wagner G et al (1999) The International Index of Erectile Function (IIEF): a multidimensional scale for the assessment of erectile dysfunction. Urology 49:822–830
Rosen RC, Cappelleri JC, Smith MD et al (1999) Development and evaluation of an abridged, 5-item version of the International Index of Erectile Dysfunction (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 11:319–326
Huyghe E, Sui D, Odensky E et al (2009) Needs assessment survey to justify establishing a reproductive health clinic at a comprehensive cancer center. J Sex Med 6:149–163
Gao X, Chen H, Schwarzschild MA et al (2007) Erectile function and risk of Parkinson’s disease. Am J Epidemiol 166:1446–1450
Celikel E, Ozel-Kizil ET, Akbostanci MC et al (2008) Assessment of sexual dysfunction in patients with Parkinson’s disease: a case-control study. Eur J of Neu 15:1168–1172
Brown RG, Jahanshahi N, Quinn N et al (1990) Sexual function in patients with Parkinson’s disease and their partners. J Neurol Neurosurg Psychiatry 53:480–486
Bronner G, Cohen OS, Yahalom G et al (2014) Correlates of quality of sexual life in male and female patients with Parkinson disease and their partners. Parkinsonism Relat Disord 20:1085–1088
McCabe MP, Taleporos G (2003) Sexual esteem, sexual satisfaction, and sexual behavior among people with physical disability. Arch Sex Behav 32:359–369
Bronner G (2012) Sexuality in patients with Parkinson’s disease: dynamic and unpredictable. Proceedings from the 15th Congress of the European Society for Sexual Medicine, Amsterdam, The Netherlands, December 6th-8th 2012. J sex Med 9(suppl 5):385
Patrick K, Heywood W, Smith AMA et al (2013) A population-based study investigating the association between sexual and relationship satisfaction and psychological distress among heterosexuals. J Sex Marital Ther 39:56–70
Moore O, Gurevich T, Korczyn AD et al (2002) Quality of sexual life in Parkinson’s disease. Parkinsonism Relat Disord 8:243–246
Basson R, Bronner G (2015) Management and rehabilitation of neurologic patients with sexual dysfunction. Handb Clin Neurol 130:415–434
Bronner G, Gurevich T (2019) Management of neurogenic sexual dysfunction. In: González-Fernández M, Panicker J (eds) Nair S. Neurorehabilitation therapeutics, Cambridge University Press, pp 224–235
Ryan KL, Arbuckle-Bernstein V, Smith G et al (2018) Let’s Talk about sex: a survey of patients’ preferences when addressing sexual health concerns in a family medicine residency program office. PRiMER 2:23
McGahuey CA, Gelenberg AJ, Laukes CA et al (2000) Arizona Sexual Experience Scale (ASEX): reliability and validity. J Sex Marital Ther 26:25–40
Jitkritsadakul O, Jagota P, Bhidayasiri R (2014) The Arizona Sexual Experiences Scale: a validity and reliability assessment of the Thai translation (ASEX-Thai) in Parkinson’s disease. J Parkinsons Dis 4:205–210
Bronner G (2009) Practical strategies for the management of sexual problems in Parkinson’s disease. Parkinsonism Relat Disord 15(Suppl 3):S96–S100
Bronner G, Korczyn AD (2018) The role of sex therapy in the management of Parkinson’s disease patients. Mov Disord Clin Pract 5:6–13
Subramanian I, Mathur S, Oosterbaan A, Flanagan R, Keener AM, Moro E (2022) Unmet needs of women living with Parkinson’s disease: gaps and controversies. Mov Disord 37:444–455
Jiann BP, Su CC, Tsai JY (2013) Is female sexual function related to the male partners’ erectile function? J Sex Med 10:420–429
Elran E, Bronner G, Uziel N et al (2014) The impact of vaginal penetration difficulties on the sexual functioning of women and their male partners. Eur J Contracept Reprod Health Care 19:352–358
Santa Rosa Malcher CM, da Silva Gonçalves Oliveira KR, FernandesCaldato MC et al (2021) Sexual disorders and quality of life in Parkinson’s disease. Sex Med 9:100280
Baumann-Vogel H, Valko PO, Eisele G, Baumann CR (2015) Impulse control disorders in Parkinson’s disease: don’t set your mind at rest by self-assessments. Eur J Neurol 22(4):603–609
Hayes RD, Bennett C, Dennerstein L, Gurrin L, Fairley C (2007) Modeling response rates in surveys of female sexual difficulty and dysfunction. J Sex Med 4:286–295
Acknowledgements
We thank our patients for their kind cooperation and Ms. Esther Eshkol for the superb editorial assistance.
Author information
Authors and Affiliations
Contributions
1) Research project: A. Conception, B. Organization, C. Execution.
2) Statistical analysis: A. Design, B. Execution, C. Review and critique.
3) Manuscript: A. Writing of the first draft, B. Review and critique.
BG: 1A, 1B, 1C, 2A, 2B, 2C, 3A, 3B
PNS: 1A, 1B, 1C, 3B
MY: 1A, 1B, 1C, 2C, 3B
RA: 1A, 1B, 1C, 2C
NS: 1B, 1C
TT: 1B, 1C
EA: 1B,1C
GT: 1A, 1B, 1C, 2C, 3B
Corresponding author
Ethics declarations
Ethical approval
(1) This study was approved by the ethics committee of the Tel-Aviv Sourasky Medical Center, Tel-Aviv, Israel, approval no. Helsinki TLV#220–16.
(2) All study details and concepts were clearly explained verbally to the patients before they signed an informed consent, after which they received an envelope containing the anonymous study questionnaires.
(3) We confirm that all authors have read the journal’s position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bronner, G., Peleg-Nesher, S., Manor, Y. et al. Sexual needs and sexual function of patients with Parkinson’s disease. Neurol Sci 44, 539–546 (2023). https://doi.org/10.1007/s10072-022-06467-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06467-0