Abstract
This study evaluates the cognitive impairment impact on the caregiver’s burden and quality of life.
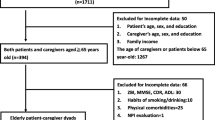
Patient–caregiver dyads admitted to dementia Diagnostic-Therapeutic Care Pathway underwent a psychological and neuropsychological assessment. Overall, 30 caregivers (age 58.97 ± 14.68) of patients with dementia and 28 caregivers (age 58.57 ± 12.22) of patients with MCI were recruited. Caregiver’s burden is positively correlated to the number (r = .37, p = .003) and severity (r = .37, p = .003) of neuropsychiatric patient’s symptoms and with the caregiver’s distress (r = .36, p = .004). It is also negatively related to good quality of life perception (r = − .52, p = < .0001), to lower cognitive impairment (r = − .26, p = .05), to higher patient’s residual functional abilities in daily living (r = − .32, p = .010) and to positive perception of the physician’s communication (r = − .28, p = .026). Moreover, the caregiver’s burden is significantly predicted by the patient’s low level of instrumental activity of daily living (β = − .74; p = .043) and by the number of neuropsychiatric symptoms (β = .74; p = .029). Thus, this study suggests that the autonomy and neuropsychiatric symptoms may determine the caregiver’s burden.


Similar content being viewed by others
References
American Psychiatric Association (APA) (2013) DSM-5. Manuale diagnostico e statistico dei disturbi mentali. Raffello Cortina Editore, Milano
Sachs-Ericsson N, Blazer DG (2015) The new DSM-5 diagnosis of mild neurocognitive disorder and its relation to research in mild cognitive impairment. Aging Ment Health 19:2–12. https://doi.org/10.1080/13607863.2014.920303
Petersen RC, Lopez O, Armstrong MJ et al (2018) Practice guideline update summary: mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 90:126–135. https://doi.org/10.1212/WNL.0000000000004826
Ganguli M, Dodge HH, Shen C, DeKosky ST (2004) Mild cognitive impairment, amnestic type: an epidemiologic study. Neurology 63:115–121. https://doi.org/10.1212/01.wnl.0000132523.27540.81
Geda YE, Roberts RO, Knopman DS et al (2008) Prevalence of neuropsychiatric symptoms in mild cognitive impairment and normal cognitive aging: population-based study. Arch Gen Psychiatry 65:1193–1198. https://doi.org/10.1001/archpsyc.65.10.1193
Prince M, Comas-Herrera A, Knapp M, Guerchet M, Karagiannidou M (2016) World Alzheimer report 2016: improving healthcare for people living with dementia: coverage, quality and costs now and in the future. Alzheimer’s Disease International (ADI), London, UK. Available at: http://eprints.lse.ac.uk/id/eprint/67858
Davis DHJ, Creavin ST, Noel-Storr A, Quinn TJ, Smailagic N, Hyde C, Brayne C, McShane R, Cullum S (2013) Neuropsychological tests for the diagnosis of Alzheimer’s disease dementia and other dementias: a generic protocol for cross-sectional and delayed-verification studies. Cochrane Dement Cogn Improv Group 28(3):CD010460
Devier DJ, Villemarette-Pittman N, Brown P et al (2010) Predictive utility of type and duration of symptoms at initial presentation in patients with mild cognitive impairment. Dement Geriatr Cogn Disord 30:238–244. https://doi.org/10.1159/000320137
Zappella E (2019) Valutare la qualità della vita nei soggetti con demenza: una rassegna delle principali scale di misurazione [Evaluating the quality of life for people with dementia: a review of the main measurement scales]. FORMAZIONE & INSEGNAMENTO. Rivista Internazionale di Scienze dell'educazione e della formazione 16(2):381–400
Birren J, Lubben Rowe JJ (1991) The concept and measurement of quality of life in the frail elderly. Academic Press, San Diego
Farina N, Page TE, Daley S et al (2017) Factors associated with the quality of life of family carers of people with dementia: a systematic review. Alzheimers Dement 13:572–581. https://doi.org/10.1016/j.jalz.2016.12.010
Etters L, Goodall D, Harrison BE (2008) Caregiver burden among dementia patient caregivers: a review of the literature. J Am Acad Nurse Pract 20:423–428. https://doi.org/10.1111/j.1745-7599.2008.00342.x
Adams KB (2006) The transition to caregiving: the experience of family members embarking on the dementia caregiving career. J Gerontol Soc Work 47:3–29. https://doi.org/10.1300/J083v47n03_02
Raggi A, Tasca D, Panerai S et al (2015) The burden of distress and related coping processes in family caregivers of patients with Alzheimer’s disease living in the community. J Neurol Sci 358:77–81. https://doi.org/10.1016/j.jns.2015.08.024
Miller DA (1981) The “sandwich” generation: adult children of the aging. Soc Work 26:419–423
Grabher BJ (2018) Effects of Alzheimer disease on patients and their family. J Nucl Med Technol 46:335–340. https://doi.org/10.2967/jnmt.118.218057
Martin LR, DiMatteo MR (2013) The Oxford Handbook of Health Communication, Behavior Change, and Treatment Adherence. Oxford University Press, New York
Vrijens B, De Geest S, Hughes DA et al (2012) A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 73:691–705. https://doi.org/10.1111/j.1365-2125.2012.04167.x
Roberto KA, Blieszner R, McCann BR, McPherson MC (2011) Family triad perceptions of mild cognitive impairment. J Gerontol B Psychol Sci Soc Sci 66:756–768. https://doi.org/10.1093/geronb/gbr107
Lingler JH, Terhorst L, Schulz R et al (2016) Dyadic analysis of illness perceptions among persons with mild cognitive impairment and their family members. Gerontologist 56:886–895. https://doi.org/10.1093/geront/gnv029
Poon E (2019) A systematic review and meta-analysis of dyadic psychological interventions for BPSD, quality of life and/or caregiver burden in dementia or MCI. Clin Gerontol 1–21.https://doi.org/10.1080/07317115.2019.1694117
Petersen RC (2011) Clinical practice. Mild cognitive impairment. N Engl J Med 364:2227–2234. https://doi.org/10.1056/NEJMcp0910237
McKhann GM, Knopman DS, Chertkow H et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:263–269. https://doi.org/10.1016/j.jalz.2011.03.005
(1994) Clinical and neuropathological criteria for frontotemporal dementia. The Lund and Manchester Groups. J Neurol Neurosurg Psychiatry 57:416–418. https://doi.org/10.1136/jnnp.57.4.416
McKeith IG, Galasko D, Kosaka K et al (1996) Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology 47:1113–1124. https://doi.org/10.1212/wnl.47.5.1113
Román GC, Tatemichi TK, Erkinjuntti T et al (1993) Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology 43:250–260
Goetz CG, Emre M, Dubois B (2008) Parkinson’s disease dementia: definitions, guidelines, and research perspectives in diagnosis. Ann Neurol 64(Suppl 2):S81-92. https://doi.org/10.1002/ana.21455
Measso G, Cavarzeran F, Zappalà G et al (1993) The mini-mental state examination: normative study of an Italian random sample. Dev Neuropsychol 9:77–85. https://doi.org/10.1080/87565649109540545
Magni E, Binetti G, Bianchetti A et al (1996) Mini-Mental State Examination: a normative study in Italian elderly population. Eur J Neurol 3:198–202. https://doi.org/10.1111/j.1468-1331.1996.tb00423.x
Siciliano M, Raimo S, Tufano D et al (2016) The Addenbrooke’s Cognitive Examination Revised (ACE-R) and its sub-scores: normative values in an Italian population sample. Neurol Sci 37:385–392. https://doi.org/10.1007/s10072-015-2410-z
Stein J, Luppa M, Luck T et al (2012) The assessment of changes in cognitive functioning: age-, education-, and gender-specific reliable change indices for older adults tested on the CERAD-NP battery: results of the German Study on Ageing, Cognition, and Dementia in Primary Care Patients (AgeCoDe). Am J Geriatr psychiatry Off J Am Assoc Geriatr Psychiatry 20:84–97. https://doi.org/10.1097/JGP.0b013e318209dd08
Arevalo-Rodriguez I, Smailagic N, Roqué I Figuls M, et al (2015) Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane database Syst Rev 2015:CD010783. https://doi.org/10.1002/14651858.CD010783.pub2
EuroQol Research Foundation (2019) EQ-5D-3L User Guide. https://euroqol.org/publications/user-guides. Accessed January 2020
Spitzer RL, Kroenke K, Williams JBW, Group and the PHQPCS (1999) Validation and utility of a self-report version of PRIME-MD The PHQ Primary Care Study. JAMA 282:1737–1744. https://doi.org/10.1001/jama.282.18.1737
Spitzer RL, Kroenke K, Williams JBW, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166:1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Scala D, Menditto E, Armellino MF et al (2016) Italian translation and cultural adaptation of the communication assessment tool in an outpatient surgical clinic. BMC Health Serv Res 16:163. https://doi.org/10.1186/s12913-016-1411-9
Rossi Ferrario S, Baiardi P, Zotti AM (2004) Update on the family strain questionnaire: a tool for the general screening of caregiving-related problems. Qual life Res Int J Qual life Asp Treat care Rehabil 13:1425–1434. https://doi.org/10.1023/B:QURE.0000040795.78742.72
Katz TF (1963) A.D.L. activities of daily living. J Am Med Assoc 185:914–919
Laicardi C, Pezzuti L, Sberna S (1998) La valutazione dell’autonomia strumentale quotidiana dell’anziano (IADL): validazione di una nuova modalità di punteggio. RICERCHE DI PSICOLOGIA, 1/1998.
Cummings JL, Frank JC, Cherry D et al (2002) Guidelines for managing Alzheimer’s disease: part I. Assessment. Am Fam Physician 65:2263–2272
Kaufer DI, Cummings JL, Ketchel P et al (2000) Validation of the NPI-Q, a brief clinical form of the neuropsychiatric inventory. J Neuropsychiatry Clin Neurosci 12:233–239. https://doi.org/10.1176/jnp.12.2.233
Gómez-Gómez ME, Zapico SC (2019) Frailty, cognitive decline, neurodegenerative diseases and nutrition interventions. Int J Mol Sci 20:2842. https://doi.org/10.3390/ijms20112842
Wassel JI (2006) Financial planning and the “senior sandwich” generation. J Financ Serv Prof 60(2):22–26
Fingerman KL, VanderDrift LE, Dotterer AM et al (2011) Support to aging parents and grown children in Black and White families. Gerontologist 51:441–452. https://doi.org/10.1093/geront/gnq114
Infurna FJ, Gerstorf D, Lachman ME (2020) Midlife in the 2020s: opportunities and challenges. Am Psychol 75:470–485
Terum TM, Andersen JR, Rongve A et al (2017) The relationship of specific items on the neuropsychiatric inventory to caregiver burden in dementia: a systematic review. Int J Geriatr Psychiatry 32:703–717. https://doi.org/10.1002/gps.4704
Viazzo PP (2003) What’s so special about the Mediterranean? Thirty years of research on household and family in Italy. Contin Chang 18:111–137. https://doi.org/10.1017/S0268416003004442
Annerstedt L, Elmståhl S, Ingvad B, Samuelsson SM (2000) Family caregiving in dementia–an analysis of the caregiver’s burden and the “breaking-point” when home care becomes inadequate. Scand J Public Health 28:23–31. https://doi.org/10.1177/140349480002800106
Carretero S, Garcés J, Ródenas F, Sanjosé V (2009) The informal caregiver’s burden of dependent people: theory and empirical review. Arch Gerontol Geriatr 49:74–79. https://doi.org/10.1016/j.archger.2008.05.004
Tilburgs B, Vernooij-Dassen M, Koopmans R et al (2018) The importance of trust-based relations and a holistic approach in advance care planning with people with dementia in primary care: a qualitative study. BMC Geriatr 18:184. https://doi.org/10.1186/s12877-018-0872-6
Maffoni M, Traversoni S, Costa E et al (2020) Medication adherence in the older adults with chronic multimorbidity: a systematic review of qualitative studies on patient’s experience. Eur Geriatr Med 11:369–381. https://doi.org/10.1007/s41999-020-00313-2
Martinez-Martin P, Rodriguez-Blazquez C, Forjaz MJ et al (2015) Neuropsychiatric symptoms and caregiver’s burden in Parkinson’s disease. Parkinsonism Relat Disord 21:629–634. https://doi.org/10.1016/j.parkreldis.2015.03.024
Signe A, Elmståhl S (2008) Psychosocial intervention for family caregivers of people with dementia reduces caregiver’s burden: development and effect after 6 and 12 months. Scand J Caring Sci 22:98–109. https://doi.org/10.1111/j.1471-6712.2007.00498.x
Funding
This work was partially supported by the “Ricerca Corrente” funding scheme of the Ministry of Health, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the institutional review board and the central ethics committee of the ICS Maugeri SpA SB (approval number: CEC N.2315, 11/06/2019).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Torlaschi, V., Maffoni, M., Maltauro, G. et al. The patient–caregiver dyad: the impact of cognitive and functional impairment. Neurol Sci 43, 2481–2490 (2022). https://doi.org/10.1007/s10072-021-05712-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05712-2