Abstract
Introduction
Concussion is defined as a mild traumatic brain injury that can occur in all sport activities. Cervical vestibular-evoked myogenic potentials (cVEMPs) are accepted to demonstrate the vestibulocollic reflex.
Main
To evaluate subclinical cervical abnormalities in the vestibulospinal pathway in subjects with concussion history with and without related symptoms via evoked vestibular potential.
Methods
Monaurally air conduction cVEMP (500 Hz tone bursts) at intensity of 100 dBnHL and 200 sweeps. All responses were replicated.
Results
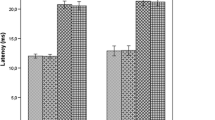
One hundred fifty-four participants were initially tested; however, three (03) participants did not produce usable data (no response) and were eliminated for the dataset cutoff values analysis, being considered just as abnormal response. One hundred fifty-one responses consisted of 45 non-athlete individuals without any history of a concussion or concussion symptoms (normative group), 45 athletes without any history of a concussion or concussion symptoms (control group), 33 athletes with a history of at least one concussion but no concussion symptoms related (history group), and 28 athletes with a history of at least one concussion and concussion symptoms (symptoms group). The history and symptoms groups had statistically higher latency scores than the control and the normative groups. The Index Ratio data and Threshold data did not produce a significant effect for four groups. But, a pattern of abnormal cVEMP was found when comparing those without a history of concussion (0% abnormal response) versus the history group (24%) and symptoms group (32.3%).
Conclusion
The study provides data which supports the positive impact of cVEMP when evaluating athletes and identifying concussion processes.

Similar content being viewed by others
References
Kerr ZY, Chandran A, Nedimyer AK, Arakkal A, Pierpoint LA, Zuckerman SL. Concussion incidence and trends in 20 high school sports. Pediatrics. 2019;144(5). doi: https://doi.org/10.1542/peds.2019-2180.
Conder A, Conder R, Friesen C (2020 Feb 21) Neurorehabilitation of persistent sport-related post-concussion syndrome. NeuroRehabilitation. 46:167–180. https://doi.org/10.3233/NRE-192966
Howell DR, O’Brien MJ, Fraser J, Meehan WP 3rd (2020) Continuing play, symptom severity, and symptom duration after concussion in youth athletes. Clin J Sport Med 30(Suppl 1):S42–S46. https://doi.org/10.1097/JSM.0000000000000570
Savikangas T, Tirkkonen A, Alen M, Rantanen T, Fielding RA, Rantalainen T, Sipilä S (2020) Associations of physical activity in detailed intensity ranges with body composition and physical function. a cross-sectional study among sedentary older adults. Eur Rev Aging Phys Act 17:4. https://doi.org/10.1186/s11556-020-0237-y
Covassin T, Moran R, Wilhelm K (2013) Concussion symptoms and neurocognitive performance of high school and college athletes who incur multiple concussions. Am J Sports Med 41(12):2885–2889
Alkathiry AA, Kontos AP, Furman JM, Whitney SL, Anson ER, Sparto PJ (2019) Vestibulo-ocular reflex function in adolescents with sport-related concussion: preliminary results. Sports Health 11(6):479–485. https://doi.org/10.1177/1941738119865262
Marcus HJ, Paine H, Sargeant M, Wolstenholme S, Collins K, Marroney N, Arshad Q, Tsang K, Jones B, Smith R, Wilson MH, Rust HM, Seemungal BM (2019) Vestibular dysfunction in acute traumatic brain injury. J Neurol 266(10):2430–2433. https://doi.org/10.1007/s00415-019-09403-z
Dwyer B, Katz DI (2018) Postconcussion syndrome. Handb Clin Neurol 158:163–178. https://doi.org/10.1016/B978-0-444-63954-7.00017-3 Review
Yue JK, Phelps RRL, Chandra A, Winkler EA, Manley GT, Berger MS (2020) Sideline concussion assessment: the current state of the art. Neurosurgery. https://doi.org/10.1093/neuros/nyaa022
Theadom A, Mahon S, Hume P, Starkey N, Barker-Collo S, Jones K, Majdan M, Feigin VL (2020) Incidence of sports-related traumatic brain injury of all severities: a systematic review. Neuroepidemiology. 14:1–8. https://doi.org/10.1159/000505424
Gardner AJ, Quarrie KL, Iverson GL (2019) The epidemiology of sport-related concussion: what the rehabilitation clinician needs to know. J Orthop Sports Phys Ther 49(11):768–778. https://doi.org/10.2519/jospt.2019.9105
Lanka P, Rangaprakash D, Gotoor SSR, Dretsch MN, Katz JS, Denney TS Jr, Deshpande G (2020) MALINI (Machine learning in neuroimaging): A MATLAB toolbox for aiding clinical diagnostics using resting-state fMRI data. Data Brief 29:105213. https://doi.org/10.1016/j.dib.2020.105213
Ofoghi Z, Dewey D, Barlow KM (2020) A systematic review of structural and functional imaging correlates of headache or pain after mild traumatic brain injury. J Neurotrauma 37:907–923. https://doi.org/10.1089/neu.2019.6750
Ebert SE, Jensen P, Ozenne B, Armand S, Svarer C, Stenbaek DS, Moeller K, Dyssegaard A, Thomsen G, Steinmetz J, Forchhammer BH, Knudsen GM, Pinborg LH (2019) Molecular imaging of neuroinflammation in patients after mild traumatic brain injury: a longitudinal I-CLINDE single photon emission computed tomography study. Eur J Neurol 26(12):1426–1432. https://doi.org/10.1111/ene.13971
Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, Kutcher JS, Pana A, Putukian M, Roberts WO (2013) American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med 47(1):15–26. https://doi.org/10.1136/bjsports-2012-091941 Review
Hubertus V, Marklund N, Vajkoczy P (2019) Management of concussion in soccer. Acta Neurochir 161(3):425–433. https://doi.org/10.1007/s00701-019-03807-6
Inness EL, Sweeny M, Habib Perez O, Danells C, Chandra T, Foster E, Saverino C, Comper P, Bayley M, Mochizuki G (2019) Self-reported balance disturbance and performance-based balance impairment after concussion in the general population. J Head Trauma Rehabil 34(3):E37–E46. https://doi.org/10.1097/HTR.0000000000000431
Ledwidge PS, Patterson JN, Molfese DL, Honaker JA (2019) Clinical utility of oculomotor and electrophysiological measures in identifying concussion history. Clin J Sport Med 29(4):292–297. https://doi.org/10.1097/JSM.0000000000000512
Stokes W, Choynowki J, St Pierre M, Anaya MA, Statton MA, Celnik PA, Cantarero G (2020) Altered corticomotor latencies but normal motor neuroplasticity in concussed athletes. J Neurophysiol 123:1600–1605. https://doi.org/10.1152/jn.00774.2019
Washnik NJ, Anjum J, Lundgren K, Phillips S (2019) A review of the role of auditory evoked potentials in mild traumatic brain injury assessment. Trends Hear 23:2331216519840094. https://doi.org/10.1177/2331216519840094
Felipe L, Kingma H, Lambertucci JR, Carneiro-Proietti AB, Gonçalves DU (2013) Testing the vestibular evoked myogenic potential (VEMP) to identify subclinical neurological alterations in different phases of human T-lymphotropic virus type 1 infection. Spine J 13(4):397–401. https://doi.org/10.1016/j.spinee.2012.11.015
Nogueira A, Tovar-Gálvez M, González-Hernández J (2019) Do it, don't feel it, and be invincible: a prolog of exercise addiction in endurance sports. Front Psychol 10:2692. https://doi.org/10.3389/fpsyg.2019.02692
Deriu F, Ginatempo F, Manca A (2019) Enhancing research quality of studies on VEMPs in central neurological disorders: a scoping review. J Neurophysiol 122(3):1186–1206. https://doi.org/10.1152/jn.00197.2019
Rosengren SM, Colebatch JG, Young AS, Govender S, Welgampola MS (2019) Vestibular evoked myogenic potentials in practice: methods, pitfalls and clinical applications. Clin Neurophysiol Pract 4:47–68. https://doi.org/10.1016/j.cnp.2019.01.005
Felipe L, Gonçalves DU, Tavares MC, Sousa-Pereira SR, Antunes CM, Lambertucci JR (2009) Vestibular-evoked myogenic potential (VEMP) in the evaluation of schistosomal myeloradiculopathy. Am J Trop Med Hyg 81(4):551–554. https://doi.org/10.4269/ajtmh.2009.09-0191
Felipe L, Carvalho SA, Cunha LC, Santos MA, Peixoto MA, Gonçalves DU (2009) Vestibular evoked myogenic potential findings on multiple sclerosis. Rev Neurol 48(6):284–286
Gouttebarge V, Kerkhoffs GMMJ (2020) Sports career-related concussion and mental health symptoms in former elite athletes. Neurochirurgie. https://doi.org/10.1016/j.neuchi.2020.01.001
Caccese JB, Bodt BA, Iverson GL, Kaminski TW, Bryk K, Oldham J, Broglio SP, McCrea M, McAllister T, Buckley TA, CARE Consortium Investigators (2020) Estimated age of first exposure to contact sports and neurocognitive, psychological, and physical outcomes in healthy NCAA collegiate athletes: a cohort study. Sports Med. https://doi.org/10.1007/s40279-020-01261-4
Alsalaheen B, Johns K, Bean R, Almeida A, Eckner J, Lorincz M (2019) Women and men use different strategies to stabilize the head in response to impulsive loads: implications for concussion injury risk. J Orthop Sports Phys Ther 49(11):779–786. https://doi.org/10.2519/jospt.2019.8760
Benna P, Bergamasco B, Bianco C, Gilli M, Ferrero P, Pinessi L (1982) Brainstem auditory evoked potentials in postconcussion syndrome. Ital J Neurol Sci 3:281–287. https://doi.org/10.1007/BF02043575
Kirkwood MW, Crossland MM, Howell DR, Wilson JC, Peterson RL (2020) A longitudinal investigation of symptom recovery following concussion in youth soccer. J Pediatr. https://doi.org/10.1016/j.jpeds.2020.01.068
Tamura K, Furutani T, Oshiro R, Oba Y, Ling A, Murata N (2020) Concussion recovery timeline of high school athletes using a stepwise return-to-play protocol: age and sex effects. J Athl Train 55(1):6–10. https://doi.org/10.4085/1062-6050-452-18
Jadischke R, Viano DC, McCarthy J, King AI (2018) Concussion with primary impact to the chest and the potential role of neck tension. BMJ Open Sport Exerc Med 4(1):e000362. https://doi.org/10.1136/bmjsem-2018-000362
Asan Z (2018 Jun) Spinal cord injury without radiological abnormality in adults: clinical and radiological discordance. World Neurosurg 114:e1147–e1151. https://doi.org/10.1016/j.wneu.2018.03.162
Kennedy E, Quinn D, Tumilty S, Chapple CM (2017 Jun) Clinical characteristics and outcomes of treatment of the cervical spine in patients with persistent post-concussion symptoms: a retrospective analysis. Musculoskelet Sci Pract 29:91–98. https://doi.org/10.1016/j.msksp.2017.03.002
Author information
Authors and Affiliations
Contributions
Each author must be identified with at least one of the following:
LF and JS designed research;
LF and JS performed research;
LF and JS analyzed data;
LF and JS wrote the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Felipe, L., Shelton, J.A. The clinical utility of the cervical vestibular-evoked myogenic potential (cVEMP) in university-level athletes with concussion. Neurol Sci 42, 2803–2809 (2021). https://doi.org/10.1007/s10072-020-04849-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04849-w