Abstract
Objective
The aim of the present study was to investigate the effects of a lifestyle intervention on cardiometabolic risk factors in patients with systemic lupus erythematosus with a high cardiovascular risk profile.
Methods
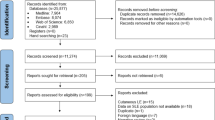
This trial was conducted in Sao Paulo, Brazil between August 2020 and March 2023. The patients were randomly assigned to lifestyle intervention or control. The intervention was a 6-month multifaced program focused on behavioral changes through personalized recommendations for increasing physical activity (structured and non-structured) and improving eating aspects. Cardiometabolic risk score (primary outcome), anthropometry and visceral fat, aerobic capacity, blood pressure, inflammatory and oxidative stress markers, and blood flow and endothelial function were assessed before and after the intervention.
Results
A total of 80 patients were randomized. Twelve and 6 patients dropped out due to personal reasons in the intervention and control groups, respectively. Average adherence rate for the intervention was 56.9%. Intention-to-treat analysis showed no significant difference between groups in the cardiometabolic risk score (intervention group – Pre: 1.7 ± 3.6; Post: -1.6 ± 4.0; control group – Pre: -1.9 ± 3.6; Post: -2.0 ± 3.8; estimated mean difference between groups at post: -0.4; 95% confidence intervals: -2.7; 1.9; p = 0.96). This finding was confirmed by exploratory, per-protocol analysis. No significant differences were observed between adherents vs. non-adherent participants. Secondary outcomes did not change between groups.
Conclusion
This 6-month, individualized, lifestyle intervention did not improve cardiovascular risk factors in SLE patients with a high cardiovascular risk profile.
Trial Registration: clinicaltrials.gov (NCT04431167).
Key Points • This study was the first to investigate the efficacy of a multifaceted lifestyle intervention in SLE patients with a high cardiovascular risk profile. • Our lifestyle intervention did not change cardiometabolic risk score or any other cardiovascular outcomes in the population. • Whether a lifestyle intervention ameliorates other health-related outcomes and wellbeing requires further assessments. |

Similar content being viewed by others
Data availability
Data may be shared upon request.
References
Borba EF, Latorre LC, Brenol JCT et al (2008) Consenso de lúpus eritematoso sistêmico. Rev Bras Reumatol 48:196–207. https://doi.org/10.1590/S0482-50042008000400002
O’neill S, Cervera R (2010) Systemic lupus erythematosus. Best Pract Res Clin Rheumatol 24:841–855. https://doi.org/10.1016/j.berh.2010.10.006
Golder V, Hoi A (2017) Systemic lupus erythematosus: an update. Med J Aust 206:215–220. https://doi.org/10.5694/mja16.01229
Ocampo-Piraquive V, Nieto-Aristizábal I, Cañas CA, Tobón GJ (2018) Mortality in systemic lupus erythematosus: causes, predictors and interventions. Expert Rev Clin Immunol 14:1043–1053. https://doi.org/10.1080/1744666X.2018.1538789
Kim CH, Al-Kindi SG, Jandali B et al (2017) Incidence and risk of heart failure in systemic lupus erythematosus. Heart 103:227–233. https://doi.org/10.1136/heartjnl-2016-309561
Giannelou M, Mavragani CP (2017) Cardiovascular disease in systemic lupus erythematosus: A comprehensive update. J Autoimmun 82:1–12. https://doi.org/10.1016/j.jaut.2017.05.008
Miyake CNH, Gualano B, Dantas WS et al (2018) Increased Insulin Resistance and Glucagon Levels in Mild/Inactive Systemic Lupus Erythematosus Patients Despite Normal Glucose Tolerance. Arthritis Care Res (Hoboken) 70:114–124. https://doi.org/10.1002/acr.23237
Tydén H, Lood C, Gullstrand B et al (2017) Endothelial dysfunction is associated with activation of the type I interferon system and platelets in patients with systemic lupus erythematosus. RMD Open 3:e000508. https://doi.org/10.1136/rmdopen-2017-000508
Rodríguez Huerta MD, Trujillo-Martín MM, Rúa-Figueroa Í et al (2016) Healthy lifestyle habits for patients with systemic lupus erythematosus: A systemic review. Semin Arthritis Rheum 45:463–470. https://doi.org/10.1016/j.semarthrit.2015.09.003
Patterson R, McNamara E, Tainio M et al (2018) Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol 33:811–829. https://doi.org/10.1007/s10654-018-0380-1
de Medeiros MCS, Medeiros JCA, de Medeiros HJ et al (2019) Dietary intervention and health in patients with systemic lupus erythematosus: A systematic review of the evidence. Crit Rev Food Sci Nutr 59:2666–2673. https://doi.org/10.1080/10408398.2018.1463966
Sabatini F, Sato P de M, Roble OJ et al (2019) Eating pleasure in a sample of Brazilian obese women: a qualitative report of an interdisciplinary intervention based on the Health at Every Size Approach (HAES). J Acad Nutr Diet 119(9):1470–1482. https://doi.org/10.1016/j.jand.2019.01.006
Nanditha A, Snehalatha C, Raghavan A et al (2018) The post-trial analysis of the Indian SMS diabetes prevention study shows persistent beneficial effects of lifestyle intervention. Diabetes Res Clin Pract 142:213–221. https://doi.org/10.1016/j.diabres.2018.05.042
Brinkley TE, Anderson A, Soliman EZ et al (2018) Long-term effects of an intensive lifestyle intervention on electrocardiographic criteria for left ventricular hypertrophy: The look AHEAD trial. Am J Hypertens 31:541–548. https://doi.org/10.1093/ajh/hpy004
Li G, Zhang P, Wang J et al (2008) The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 371:1783–1789. https://doi.org/10.1016/S0140-6736(08)60766-7
Ali MK, Echouffo-Tcheugui J, Williamson DF (2012) How effective were lifestyle interventions in real-world settings that were modeled on the diabetes prevention program? Health Aff 31:67–75. https://doi.org/10.1377/hlthaff.2011.1009
Lindström J, Ilanne-Parikka P, Peltonen M et al (2006) Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 368:1673–1679. https://doi.org/10.1016/S0140-6736(06)69701-8
Sieczkowska SM, Smaira FI, Mazzolani BC et al (2023) A randomized controlled trial of an intervention promoting physical activity and healthy eating recommendations in systemic lupus erythematosus: the protocol study “Living Well with Lupus.” Rheumatol Int. https://doi.org/10.1007/s00296-023-05370-x
Sutton EJ, Davidson JE, Bruce IN (2013) The Systemic Lupus International Collaborating Clinics (SLICC) damage index: A systematic literature review. Semin Arthritis Rheum 43:352–361. https://doi.org/10.1016/j.semarthrit.2013.05.003
Michie S, van Stralen MM, West R (2011) The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci 6:42. https://doi.org/10.1186/1748-5908-6-42
Prochaska JO, Velicer WF (1997) The Transtheoretical Model of Health Behavior Change. Am J Heal Promot 12:38–48. https://doi.org/10.4278/0890-1171-12.1.38
Motta DG (2009) Aconselhamento nutricional. Educação Nutricional & Diabetes Tipo 2:27–33
Dempsey PC, Larsen RN, Winkler EAH et al (2018) Prolonged uninterrupted sitting elevates postprandial hyperglycaemia proportional to degree of insulin resistance. Diabetes Obes Metab 20:1526–1530. https://doi.org/10.1111/dom.13254
HOWLEY ET, BASSETT DR, WELCH HG (1995) Criteria for maximal oxygen uptake. Med Sci Sport Exerc 27:1292???1301. https://doi.org/10.1249/00005768-199509000-00009
Wasserman K (1984) The Anaerobic Threshold Measurement to Evaluate Exercise Performance 1, 2. Am Rev Respir Dis 129:S35–S40. https://doi.org/10.1164/arrd.1984.129.2P2.S35
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. https://doi.org/10.1007/BF00280883
Thijssen DHJ, Black MA, Pyke KE et al (2010) Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol. https://doi.org/10.1152/ajpheart.00471.2010
Harris RA, Nishiyama SK, Wray DW et al (2010) Ultrasound assessment of flow-mediated dilation. Hypertension 55(5):1075–1085
Thijssen DHJ, Bruno RM, van Mil ACCM et al (2019) Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J 40:2534–2547. https://doi.org/10.1093/eurheartj/ehz350
Touma Z, Gladman DD, Ibañez D et al (2011) Systemic Lupus Erythematosus Disease Activity Index 2000 Responder Index-50 Enhances the Ability of SLE Responder Index to Identify Responders in Clinical Trials. J Rheumatol 38:2395–2399. https://doi.org/10.3899/jrheum.110550
Bacchetti P, McCulloch CE, Segal MR (2008) Simple, defensible sample sizes based on cost efficiency. Biometrics 64:577–585. https://doi.org/10.1111/j.1541-0420.2008.01004_1.x
Bacchetti P (2010) Current sample size conventions: Flaws, harms, and alternatives. BMC Med 8:17. https://doi.org/10.1186/1741-7015-8-17
van Namen M, Prendergast L, Peiris C (2019) Supervised lifestyle intervention for people with metabolic syndrome improves outcomes and reduces individual risk factors of metabolic syndrome: A systematic review and meta-analysis. Metabolism 101:153988. https://doi.org/10.1016/j.metabol.2019.153988
Limbachia J, Ajmeri M, Keating BJ et al (2022) Effects of lifestyle interventions on cardiovascular risk factors in South Asians: a systematic review and meta-analysis. BMJ Open 12:e059666. https://doi.org/10.1136/bmjopen-2021-059666
Aamot I-L, Forbord SH, Gustad K et al (2014) Home-based versus hospital-based high-intensity interval training in cardiac rehabilitation: a randomized study. Eur J Prev Cardiol 21:1070–1078. https://doi.org/10.1177/2047487313488299
McDermott MM, Spring B, Tian L et al (2021) Effect of Low-Intensity vs High-Intensity Home-Based Walking Exercise on Walk Distance in Patients With Peripheral Artery Disease. JAMA 325:1266. https://doi.org/10.1001/jama.2021.2536
Ohno Y, Shibazaki S, Araki R et al (2016) Lifestyle Modifications Versus Antihypertensive Medications in Reducing Cardiovascular Events in an Aging Society: A Success Rate-oriented Simulation. Intern Med 55:2185–2195. https://doi.org/10.2169/internalmedicine.55.6247
Konopka AR, Laurin JL, Schoenberg HM et al (2019) Metformin inhibits mitochondrial adaptations to aerobic exercise training in older adults. Aging Cell. https://doi.org/10.1111/acel.12880
Lalani S, Kokkinos P, Gandhi S, Nylen E (2016) Metformin attenuates cardiorespiratory fitness in diabetics. Diabetes 65:189
Menconi M, Fareed M, O’Neal P et al (2007) Role of glucocorticoids in the molecular regulation of muscle wasting. Crit Care Med 35(9):S602–S608
Mikus CR, Boyle LJ, Borengasser SJ et al (2013) Simvastatin impairs exercise training adaptations. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2013.02.074
Mascitelli L, Pezzetta F (2009) Physical activity in statin-treated patients. Int J Cardiol. https://doi.org/10.1016/j.ijcard.2007.12.048
Diabetes Prevention Program Research Group (2009) 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. https://doi.org/10.1016/S0140-6736(09)61457-4
Johansen MY, Macdonald CS, Hansen KB et al (2017) Effect of an intensive lifestyle intervention on glycemic control in patients with type 2 diabetes: A randomized clinical trial. JAMA - J Am Med Assoc 318:637–646. https://doi.org/10.1001/jama.2017.10169
Wood DA, Kotseva K, Connolly S et al (2008) Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: A paired, cluster-randomised controlle. Lancet. https://doi.org/10.1016/S0140-6736(08)60868-5
Zhang X, Devlin HM, Smith B et al (2017) Effect of lifestyle interventions on cardiovascular risk factors among adults without impaired glucose tolerance or diabetes: A systematic review and metaanalysis. PLoS ONE 12:1–27. https://doi.org/10.1371/journal.pone.0176436
Acknowledgements and Funding
S.M.S, B.C.M., F.I.S., and B.G. were supported by São Paulo Research Foundation – FAPESP (grants #2019/15231-4, # 2019/14820-6, # 2019/14819-8 and #2017/13552-2),MR was supported by Support fund to education, research and extension at the State University of Campinas – FAEPEX accord 519.292 (98082-22) and SGP was supported by National Council for Scientific and Technological Development—CNPq (#303116/2022-6).
Author information
Authors and Affiliations
Contributions
SMS, BCM, FIS, and BG participated in the conception and design of the study. SMS, BCM, FIS, and MR were involved in patients’ recruitment and data collection. SP, ALSP, FRL, SU, and VRO were involved in patients’ screening and clinical assessments. SMS, BCM, FIS, MR, FBB, HR, and BG were in charge of the statistical analyses, data interpretation, and manuscript writing. SMS, BCM, FIS, and BG drafted the manuscript with critical revision from MR, SP, ALSP, FRL, SU, VRO, FBB, and HR. All authors saw and approved the final version of the manuscript for publication.
Corresponding author
Ethics declarations
All research protocols were approved by the local Ethical Committee (Commission for Analysis of Research Projects, CAPPesq; approval: 19554719.5.0000.0068), and informed consent was obtained from all participants. Confidentiality and privacy of the participants were rigorously maintained throughout the study, and the findings are reported with integrity and transparency.
Competing interest
All the authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sieczkowska, S.M., Mazzolani, B.C., Smaira, F.I. et al. Effects of a lifestyle intervention on cardiovascular risk factors in systemic lupus erythematosus patients: The study “Living well with lupus”. Clin Rheumatol 43, 1003–1013 (2024). https://doi.org/10.1007/s10067-024-06870-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-024-06870-2