Abstract
Background
Longitudinal data on the trends in systemic lupus erythematous (SLE) readmissions are limited. We aimed to study trends in 30-day readmissions of patients admitted for SLE flares and all SLE hospitalizations in the USA from 2010 to 2018.
Materials and methods
Data were obtained from the nationwide readmission database (NRD). We performed a retrospective 9-year longitudinal trend analysis using the 2010–2018 NRD databases. We searched for index hospitalizations of adult patients diagnosed with SLE using the International Classification of Diseases (ICD) codes. Elective and traumatic readmissions were excluded from the study. Multivariable logistic and linear regression analyses were used to calculate the adjusted p value trend for categorical and continuous outcomes, respectively.
Results
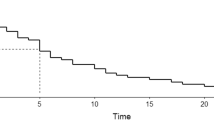
The 30-day readmissions following index admissions of all SLE patients and for SLE flares decreased from 15.6% in 2010 to 13.3% in 2018 (adjusted p trend < 0.0001), and 20.3% in 2010 to 17.6% in 2018 (adjusted p trend = 0.009) respectively. Following SLE-flare admissions, hospital length of stay (LOS) decreased from 6.7 to 6 days (adjusted p trend = 0.045), while the proportion with a Charlson comorbidity index (CCI) score ≥ 3 increased from 42.2 to 54.4% (adjusted p trend < 0.0001) during the study period. SLE and its organ involvement, sepsis, and infections were common reasons for 30-day readmissions.
Conclusion
About 1 in 5 SLE-flare admissions resulted in a 30-day readmission. The 30-day readmissions following index hospitalization for SLE flares and all SLE hospitalizations have decreased in the last decade. Although the readmission LOS was reduced, the CCI score increased over time.
Key Points • The 30-day readmissions following index hospitalization for SLE flares and all SLE hospitalizations have reduced in the last decade although the CCI score increased over time. • SLE, its organ involvement, and infections are common reasons for readmission. • Infection control strategies, optimal management of SLE and its complications, and emphasis on an ideal transition of care are essential in reducing SLE readmissions. |

Similar content being viewed by others
References
Sreedharan Pillai S, Velayudhan G (2017) Thyroid dysfunction in SLE and association of thyroid antibody levels with disease activity in SLE. J Evol Med Dental Sci 6(33):2684–2688. https://doi.org/10.14260/jemds/2017/579
Stojan G, Petri M (2018) Epidemiology of systemic lupus erythematosus: an update. Curr Opin Rheumatol 30(2):144–150. https://doi.org/10.1097/bor.0000000000000480
Teh CL, Chan GYL, Lee J (2008) Systemic lupus erythematosus in a tertiary, east Malaysian hospital: admission, readmission and death. Int J Rheum Dis 11(1):24–29. https://doi.org/10.1111/j.1756-185x.2008.00325.x
Yeh KW, Yu CH, Chan PC, Horng JT, Huang JL (2013) Burden of systemic lupus erythematosus in Taiwan: a population-based survey. Rheumatol Int 33(7):1805–1811. https://doi.org/10.1007/s00296-012-2643-6
Xie X, Song Y, Yang H, Nie A, Chen H, Li JP (2018) Effects of transitional care on self-care, readmission rates, and quality of life in adult patients with systemic lupus erythematosus: a randomized controlled trial. Arthritis Research &Amp; Therapy 20(1) https://doi.org/10.1186/s13075-018-1670-4
Panopalis P, Yazdany J, Gillis JZ, Julian L, Trupin L, Hersh AO, Criswell LAKP, Yelin E (2008) Health care costs and costs associated with changes in work productivity among persons with systemic lupus erythematosus. Arthritis & Amp; Rheumatism 59(12):1788–1795. https://doi.org/10.1002/art.24063
Yazdany J, Marafino BJ, Dean ML, Bardach NS, Duseja R, Ward MM, Dudley RA (2014) Thirty-day hospital readmissions in systemic lupus erythematosus: predictors and hospital- and state-level variation. Arthritis & Amp; Rheumatol 66(10):2828–2836. https://doi.org/10.1002/art.38768
Anandarajah AP, Luc M, Ritchlin CT (2016) Hospitalization of patients with systemic lupus erythematosus is a major cause of direct and indirect healthcare costs. Lupus 26(7):756–761. https://doi.org/10.1177/0961203316676641
Lai JS, Beaumont JL, Jensen SE, Kaiser K, Van Brunt DL, Kao AH, Chen SY (2016) An evaluation of health-related quality of life in patients with systemic lupus erythematosus using PROMIS and Neuro-QoL. Clin Rheumatol 36(3):555–562. https://doi.org/10.1007/s10067-016-3476-6
Nikpour M, Urowitz MB, Ibañez D, Gladman DD (2009) Frequency and determinants of flare and persistently active disease in systemic lupus erythematosus. Arthritis & Amp; Rheumatism 61(9):1152–1158. https://doi.org/10.1002/art.24741
Medical Expenditure Panel Survey (MEPS) | Agency for Healthcare Research and Quality. (n.d.). https://www.ahrq.gov/data/meps.html
Wei L, Wang J, Li Z, Zhang Y, Gao Y (2019) Design and implementation of an Omaha System-based integrated nursing management model for patients with newly-diagnosed diabetes. Prim Care Diabetes 13(2):142–149. https://doi.org/10.1016/j.pcd.2018.11.001
Le Berre M, Maimon G, Sourial N, Guériton M, Vedel I (2017) Impact of transitional care services for chronically ill older patients: a systematic evidence review. J Am Geriatr Soc 65(7):1597–1608. https://doi.org/10.1111/jgs.14828
Bowers E, Griffith M, Kolfenbach J, Pearson D, Hammes A, Weinstein E (2021) Quality improvement intervention to reduce thirty-day hospital readmission rates among patients with systemic lupus erythematosus. Arthritis Care & Amp Res 74(1):126–130. https://doi.org/10.1002/acr.24435
Clemente D, Leon L, Foster H, Carmona L, Minden K (2017) Transitional care for rheumatic conditions in Europe: current clinical practice and available resources. Pediatric Rheumatology 15(1) https://doi.org/10.1186/s12969-017-0179-8
Yu DSF, Lee DTF, Stewart S, Thompson DR, Choi KC, Yu CM (2015) Effect of nurse-implemented transitional care for Chinese individuals with chronic heart failure in Hong Kong: a randomized controlled trial. J Am Geriatr Soc 63(8):1583–1593. https://doi.org/10.1111/jgs.13533
Maidhof W, Hilas O (2012) Lupus: an overview of the disease and management options. P T. 37(4):240–9
Anastasiou C, Trupin L, Glidden DV, Li J, Gianfrancesco M, Shiboski S, Schmajuk G, Yazdany J (2021) Mortality among hospitalized individuals with systemic lupus erythematosus in the US between 2006 and 2016. Arthritis Care & Amp Res 73(10):1444–1450. https://doi.org/10.1002/acr.24356
Parra Sánchez AR, Voskuyl AE, van Vollenhoven RF (2022) Treat-to-target in systemic lupus erythematosus: advancing towards its implementation. Nat Rev Rheumatol 18(3):146–157. https://doi.org/10.1038/s41584-021-00739-3
Kalra AD, Fisher RS, Axelrod P (2010) Decreased length of stay and cumulative hospitalized days despite increased patient admissions and readmissions in an area of urban poverty. J Gen Intern Med 25(9):930–935. https://doi.org/10.1007/s11606-010-1370-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Idolor, O., Edigin, E., Eseaton, P.O. et al. Systemic lupus erythematous readmissions have reduced: a 9-year longitudinal study of the nationwide readmission database. Clin Rheumatol 42, 377–383 (2023). https://doi.org/10.1007/s10067-022-06476-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06476-6