Abstract
Objective
To compare the effects of telerehabilitation vs home-based exercise programs for knee osteoarthritis (KOA).
Method
Patients diagnosed with moderate/mild KOA were enrolled in the study and randomized into two groups. The patients in the telerehabilitation group did their exercises via video conference simultaneously, accompanied by a physiotherapist, while the patients in the control group were given a brochure showing how to do the exercises and explaining how to do each exercise. Patients completed 30-s chair stand test (30 CST), Knee Injury and Osteoarthritis Outcome Score (KOOS), Numeric Rating Scale (NRS), International Physical Activity Questionnaire Short Form (IPAQ-SF), Hospital Anxiety and Depression Scale (HADS), TAMPA Kinesiophobia Scale (TKS), Fatigue Severity Scale (FSS) twice before and after 8-week treatment, and Quality Indicators Questionnaire for Physiotherapy Management of Hip and Knee Osteoarthritis (QUIPA) and Exercise Adherence Rating Scale (EARS) after treatment only. Moreover, the number of painkillers that patients used in the last 15 days was recorded before and after treatment, and patient satisfaction with treatment was questioned after treatment.
Results
Forty-eight patients were included in the study. The mean age of patients was 55.83 ± 6.93 years, and 43 (89.6%) patients were women. No significant differences were determined between groups in terms of baseline characteristics. After the 8-week follow-up, telerehabilitation group demonstrated better 30 CST, IPAQ-SF, KOOS, QUIPA, treatment satisfaction, and total and C subscale of EARS scores increment and greater NRS, HADS, TKS, and FSS score reduction than the control group. It was determined that there was a statistically significant difference between the telerehabilitation and control groups for all of the specified parameters; however, no statistically significant difference was found for the B subscale of EARS.
Conclusion
This study indicated that telerehabilitation is superior to self-management. Moreover, through this innovative and population specific web-based approach for KOA, a vast number of patients who have internet access could be reached. Thus, patients with KOA received effective treatment.
Key Points • Telerehabilitation is superior to self-management. • Telerehabilitation is a quality practice with the potential to reduce symptoms in patients with knee OA. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the most common degenerative joint disease with an inflammatory component that starts from the matrix of the articular cartilage, progresses with disruption of chondrocyte responses and results in tissue destruction. In OA, primary involvement is seen in the articular cartilage, and progressive damage occurs. However, although the articular cartilage is initially affected, the synovial membrane, subchondral bone, ligaments, joint capsule and periarticular muscles are also affected in the later stages. These degenerative changes in the pathophysiology of the disease make OA an important cause of disability [1,2,3,4]. It has been reported that approximately 250 million people worldwide suffer from OA. Among them, the prevalence of knee OA (KOA) is the highest, with 16–17% in the population aged 50 to 75 years [5]. Moreover, KOA is one of the five leading causes of disability in adults over 50. Therefore, it is a significant threat to patients’ quality of life (QoL) and independence [6].
Joint pain is considered the main cause of functional impairment and disability in patients with KOA [7]. However, OA patients suffer from a range of extra-articular symptoms which also leads to functional impairment and disability such as fatigue, depression, anxiety, fear of movement, physical inactivity, and decreased muscle strength [8,9,10,11,12]. As a result of all these symptoms, the QoL of patients with KOA deteriorates [13]. To address these issues and control the progression of OA, lifestyle modification is one of the effective strategies universally recommended in OA guidelines. Lifestyle modification includes physical exercises, self-management, and efficient learning of OA-related information [14].
Physical exercises play an important role in balancing cytokine dynamics in synovial fluid, inhibiting inflammatory reactions and oxidative stress [5]. Over the past 15 years, numerous studies have emerged supporting the beneficial effects of exercise in the treatment of KOA [15,16,17]. In many randomized controlled trials, the use of muscle strengthening and range-of-motion exercises has been observed to reduce pain and improve function in people with KOA, even with only moderate adherence to exercise [18,19,20]. KOA management with exercise is recognized as the cornerstone of conservative and self-treatment for this chronic disease [17]. However, applying a lifestyle modification strategy to individuals with KOA upon discharge from the healthcare setting remains a challenge [21]. The lack of professional supervision and feedback will result in reduced participation in continuing OA medical or rehabilitative services, which in turn will reduce the effectiveness of OA treatments [22]. In addition, studies have found that very few medical facilities and resources can be accessed in rural areas where the health-related QoL of the elderly is reported to be low [23].
With the development of telemedicine, it has been determined that patients living in remote areas have the chance to communicate with professional physicians simultaneously. The concept of telerehabilitation has been introduced in the field of physical medicine and rehabilitation, which combines telemedicine and rehabilitation interventions to support ongoing rehabilitation services for patients [24]. Internet-based rehabilitation is one of the effective strategies in telerehabilitation. The use of the internet to provide health-related interventions has the potential to reduce the cost of treatment and improve user satisfaction. There are many barriers to patient face-to-face care, such as distance, cost of travel, length of absence from work, and limited access to healthcare providers in rural areas [25]. In addition to these obstacles, the necessity of social isolation due to circumstances such as the recent Covid-19 pandemic restricts patients from receiving face-to-face treatment. However, these obstacles can be overcome with internet-based treatment systems.
The optimal design of modules related to lifestyle modification in internet-based rehabilitation programs has been taken into account in patients with KOA as in other diseases. In order to investigate the feasibility and effectiveness of internet-based rehabilitation in individuals with KOA, many studies have been conducted in which internet-based applications such as “Join2Move,” “PainCOACH,” and “Help My Knees” are included in treatment programs, as well as treatment applications via message, e-mail, and video [26,27,28]. The results of some of these studies suggest that the internet can be used successfully as a tool to provide self-management and rehabilitation interventions to patients with KOA. It has been reported that pain, stiffness, and fatigue are reduced, and physical activity, function, mood, and QoL are improved in individuals who receive individualized and interactive treatment. It was also stated that patients were satisfied with the internet-based treatment approach [29]. However, the effectiveness of telerehabilitation in patients with KOA differs in studies due to reasons such as ensuring compliance with internet-based rehabilitation, education level, and willingness of the participants, whether remote control reminders such as e-mail, telephone, or text were set up during the research and so on [27]. Studies evaluating these parameters have been conducted in many countries such as China, Australia, Canada, South Korea, Denmark, Spain, America, and Germany [29].
Considering the development of technology and the conditions of the pandemic period, it is important to evaluate the acceptability, feasibility, and compliance of telerehabilitation in different populations for patients with KOA in order to determine telerehabilitation results in a universal way. In studies on telerehabilitation in patients with KOA, the level of patients’ satisfaction with the treatment was evaluated. Yet, there is no study in the literature in which the quality of the physiotherapy and rehabilitation program applied to the patient is evaluated by the patient. Besides, also, there is no study in the literature that includes a simultaneous treatment program for patients with KOA, accompanied by a physiotherapist, via video conference. This study was planned to fill these gaps in the literature. Therefore, the aim of this study was to examine the effects of simultaneous telerehabilitation with a physiotherapist in patients with KOA and to evaluate the quality of the physiotherapy and rehabilitation program received through telerehabilitation.
Materials and methods
Trial design
The present study was approved by the Research Ethics Committee of a university. It is a randomized controlled trial and carried out according to the Declaration of Helsinki [30]. All patients provided online informed consent.
Participants
Patients diagnosed with mild to moderate KOA by their physicians according to both the American College of Rheumatology (ACR) Clinical and Radiographic Classification Criteria were recruited [31]. The radiographs were procured as part of the patients’ routine care; they were not exclusive to this study. Additional inclusion criteria comprised being a volunteer to participate in the study; living independently; being able to walk without using an assistive device; owning a mobile phone, tablet, or computer with an internet connection; and being able to use the device without assistance. Exclusion criteria involved having been diagnosed with any other systemic rheumatic diseases, having been involved in a physiotherapy and rehabilitation program in any health institution in the last 6 months, having knee-related surgery, having meniscal or ligament-associated tears occurred in the past 6 months, having answered yes to at least 1 of the first 7 questions of the Physical Activity Readiness Questionnaire for Everyone [32], having a history of falling more than 2 times in the last 6 months, having a history of knee injection in the last 4 weeks or scheduled in the next 8 week, being illiterate, having cognitive problems, having blurred vision problem, and having hearing loss.
Procedure
The patients who were informed and eligible for the study were randomized into the treatment and control groups through a randomization program. For the patients in the treatment group, telerehabilitation was performed using the Zoom Meetings application, via video conference simultaneously, accompanied by a physiotherapist. The patients in the control group were given a brochure showing how to do the exercises and explaining how to do each exercise.
Participants were informed about how to download the free Zoom Meetings application where the physical performance test for both groups and treatment for the telerehabilitation group will be held. In addition, the meeting identification number and passcode required to attend the Zoom meeting were sent to the participants via message. While the patients in the control group used the Zoom Meetings application only during the evaluation on the baseline and after 8 weeks, the patients in the treatment group used it 24 times in total for telerehabilitation, excluding their evaluations. Additionally, patient education was given to each patient after the evaluation via Zoom Meetings application.
The treatment was the same for both groups and included knee extension, knee flexion, and hip flexion in sitting position; chair sit-up; isometric contraction of quadriceps and hip adductor muscles and straight leg raise in supine position; hip abduction and adduction in the side-lying position; narrow and wide angle squats and standing on one leg in the standing position. Moreover, after completing all these exercises, hamstring stretching while sitting in a chair and quadriceps stretching exercises in the side-lying position were performed. The duration and repetitions of these exercises were increased on a weekly basis. Telerehabilitation was carried out 3 days a week, for 45–60 min a day and for 8 weeks, with a physiotherapist. Patients in the control group did these exercises on their own.
Clinical outcome measures
Clinical outcomes were measured at baseline and after 8 weeks treatment. Only a physical performance test (30-s chair stand test) was assessed via Zoom Meetings application by a physiotherapist. Other outcomes including demographic features were evaluated using online questionnaires.
30 CST
This physical performance test was used to evaluate lower extremity muscle strength and dynamic balance. The individual sits on a chair with no arm support, back support, and an average height of 44 cm from the floor. The back of the chair is against the wall so that it does not slide during the test process. When the individual sits on the chair, it is recommended that the feet be further back than the knee joint so that their feet touch the ground and can sit and stand up faster. Within the framework of the instructions, it is ensured that the individual crosses his arms over his shoulders and makes two attempts. By keeping time with a stopwatch, the learner is asked to sit and stand for 30 s, and the score obtained is recorded in the evaluation form as the number of repetitions. During the test, care is taken to ensure that the individual is without shoes [33].
Physical Activity Readiness Questionnaire for Everyone
The questionnaire contains a total of 48 questions, including 7 preliminary questions and 10 additional questions (with 41 subdomains). The answers consist of yes and no options. Physicians do not see any inconvenience in making individuals who answer “no” to all of the first 7 questions become more physically active.
KOOS
Physical functioning of patients was assessed with this questionnaire. It has 5 subgroups: pain, symptoms, functional status in activities of daily living, sports and leisure activities, and knee-related quality of life. It consists of 42 questions in total [34].
Pain severity
It was evaluated with the Numeric Rating Scale (NRS). The NRS is a semi-quantitative method for subjective measurement of a sensitivity level (e.g., pain). This scale consists of a line [35]. Moving away from the left edge on this line indicates an increase in sensory intensity (e.g., 0: No pain (left edge), 10: Unbearable pain (right edge)) [36].
Physical activity level
It was assessed by the International Physical Activity Questionnaire Short Form (IPAQ-SF). It is a form consisting of 9 questions used to measure the physical activity level of the participants. The questions are about the time the participants have consumed in physical activity they have done in the last week. The IPAQ allows the calculation of metabolic equivalent (MET) by measuring frequency, duration, and physical activity intensity level over the past 7 days across all contexts and presents the amount of physical activity per week. It is calculated as weekly working hours (MET-hours/week) [37].
HADS
This scale is a self-report scale and consists of 14 items, 7 of which investigate depression and 7 anxiety symptoms. The purpose of the scale is not to make a diagnosis. It is to determine the risk group by screening for anxiety and depression in a short time in patients with physical illness. In addition, the scale can be used to evaluate the change in the emotional status of patients [38].
QUIPA
It is a patient-based outcome measurement method in which the quality of the physiotherapy treatment received by patients for hip and/or KOA is evaluated. It consists of 17 questions [39].
TKS
It is a 17-item scale developed to assess fear of movement/re-injury. The scale includes parameters of injury/re-injury and fear-avoidance in work-related activities [40].
EARS
It is a 16-item scale developed to evaluate the adherence of individuals to the exercises recommended for individuals with chronic diseases, and the reasons for their compliance or non-compliance. It consists of 3 subscales. Subscale A does not participate in scoring. Subscale B (evaluates self-reported adherence to exercises) consists of 6 questions and subscale C (evaluates the reasons for the compliance or non-compliance with the recommended exercise) consist of 10 questions, and these subscales are scored. [41].
FSS
It is a 9-item scale developed to assess fatigue. The participant is asked to answer the questions considering his fatigue in the last 1 month, including the day of the evaluation [42].
Patient satisfaction with treatment
It was evaluated with a 5-point Likert scale. For this scale, the lowest score indicates “not satisfied at all,” and the highest score indicates “very satisfied” [43].
Thirty-second chair stand test (30 CST), Knee Injury and Osteoarthritis Outcome Score (KOOS), NRS, IPAQ, HAQ, TAMPA Kinesiophobia Scale (TKS), and Fatigue Severity Scale (FSS) were evaluated twice, before and after the treatment. The Exercise Adherence Rating Scale (EARS), Quality Indicators Questionnaire for Physiotherapy Management of Hip and Knee Osteoarthritis (QUIPA tool), and the patient’s level of satisfaction with the treatment will be administered and evaluated after treatment only.
Statistical analysis
The minimum sample size to be included in the study was analyzed using the G-Power (Version 3.1.9.2, University of Dusseldorf, Dusseldorf, Germany) program. According to the results of the sample size analysis performed with 5% type 1 and 90% type 2 errors, the study was planned with a total of 40 patients, 20 of which were in the telerehabilitation group and 20 of which were in the control group. Considering the possible losses, it was decided to include at least 22 patients for both groups. SPSS 25 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.) was used to analyze the data. Qualitative data were expressed as percentages, and quantitative data were expressed as mean ± standard deviation. The conformity of the data to the normal distribution was evaluated with the Shapiro–Wilk and Levene tests. Multiple regression analysis was carried out to analyze post-intervention outcome measures as independent variables and the telerehabilitation or control group as dependent variables. Pre-intervention outcome measures were subsumed as covariates. The statistical significance level was accepted as p < 0.05 for all the analyses performed [44].
Results
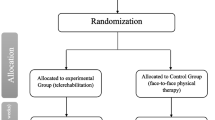
The participant flowchart of the control and intervention group, including losses to follow-up and exclusions, is demonstrated in Fig. 1. Out of a total of 64 patients interviewed for the study, 50 patients meeting the inclusion criteria were randomized, 25 to the telerehabilitation group and 25 to the control group. One participant in both groups was lost to follow-up and hence also excluded from the analyses. A total of 48 patients were analyzed. The mean age of patients was 55.83 ± 6.93 years, and 43 (89.6%) patients were women. The mean age of patients in the telerehabilitation group was 55.87 ± 7.24 years, and it was 55.79 ± 6.76 years in the control group. There were 21 (87.5%) women in the intervention, and 22 women (91.7%) in the control group. No significant differences were observed between groups with regard to gender and age before treatment. Most of the patients in both groups were primary school graduates and non-working. The mean baseline demographic and clinical characteristics are presented in Table 1. The variables were similar for patients in both groups.
Table 2 indicates the multiple regression analysis findings. The telerehabilitation group demonstrated significant improvements for the outcomes of the number of painkillers used in the last 15 days, 30 CST, knee pain on the NRS, KOOS total, and all the subscales’ scores, Hospital Anxiety and Depression Scale (HADS) total and both subscales scores, TKS score, FSS score, and IPAQ-SF score. The control group indicated significant improvements in the 30 CST, KOOS daily living activities and function subscale, HADS total, and both subscales scores and TKS score.
Mean change from baseline to 8 weeks indicated that the number of painkillers used in the last 15 days (between-group difference, − 4.62[95%CI, − 6.32 to -2.92]; p ≤ 0.001); 30 CST (between-group difference, 5.25 [95%CI, 4.18 to 6.31]; p ≤ 0.001); knee pain on the NRS (between-group difference, − 3.83 [95%CI, − 5.10 to − 2.56]; p ≤ 0.001); KOOS total (between-group difference, 27.66 [95%CI, 15.44 to 39.88]; p ≤ 0.001), symptoms (between-group difference, 24.75 [95%CI, 12.90 to 36.59]; p ≤ 0.001), pain (between-group difference, 30.95 [95%CI, 18.77 to 43.14]; p ≤ 0.001), functional status-daily living activities (between-group difference, 29.54 [95%CI, 17.07 to 42.01]; p ≤ 0.001), functional status-sports and leisure activities (between-group difference, 30.20 [95%CI, 14.08 to 46.33]; p ≤ 0.001) and knee-related QoL (between-group difference, 23.95 [95%CI, 11.28 to 36.63]; p ≤ 0.001) subscales’ scores; and HADS total (between-group difference, − 5.33 [95%CI, − 8.20 to − 2.46]; p ≤ 0.001), anxiety (between-group difference, − 2.62[95%CI, − 4.37 to 0.87]; p = 0.004), and depression (between-group difference, − 2.70[95%CI, − 4.21 to − 1.19]; p ≤ 0.001) subscales’ scores; TKS score (between-group difference, − 4.79[95%CI, − 8.21 to1.36]; p = 0.007), FSS score (between-group difference, − 1.91[95%CI, − 2.62 to − 1.20]; p ≤ 0.001), and IPAQ-SF score (between-group difference, 394.77[95%CI, 19.05 to 770.48]; p = 0.040) outcomes improved significantly in the telerehabilitation group compared to the control group (Table 2). No serious adverse events were notified in any of the groups.
The parameters evaluated only after the end of treatment are shown in Table 3. After 8 weeks of treatment, it was determined that there was a statistical difference in all subscales and total score of QUIPA in the telerehabilitation group compared to the control group. Moreover, there was a statistical difference in the C subscale and total score of EARS in the telerehabilitation group compared to the control group. However, no statistically significant difference was found between the telerehabilitation and control groups for the B subscale of EARS. When the treatment satisfaction levels of the groups were compared, it was determined that there was a statistically significant difference in the telerehabilitation group compared to the control group.
Discussion
Until today, unfortunately, the great majority of patients with KOA remains sedentary and receives no support for the augmentation of physical activity. Since a physically active way of life has been linked with decreased pain and increased physical function, accessible and effective physiotherapy programs are required [45]. Therefore, this study was designed to determine the effectiveness of telerehabilitation and the quality of physiotherapy for patients with KOA. The aim of this study was to examine the effects of telerehabilitation on physical performance, pain, functional status, emotional status, kinesiophobia, fatigue, and physical activity level in patients with KOA and to evaluate the exercise compliance, satisfaction with the treatment, and the quality of the physiotherapy they received. The results of this study demonstrated improvements in terms of the mentioned parameters for the telerehabilitation group.
It has been reported in the literature that the incidence of KOA is higher in women than in men [46]. In our study, female patients were in the majority in both the telerehabilitation and control groups. In terms of gender distribution, our findings are compatible with studies in the literature [27, 47, 48]. KOA, one of the five leading causes of disability in adults over 50, is a significant threat to patients’ QoL and independence [49]. In our study, the mean age of the patients in the telerehabilitation group and the control group was over 50 years, too. In similar studies in the literature, the mean age of the patients was over 50 years [50,51,52]. In terms of age distribution, our findings are compatible with studies in the literature. Obesity and being overweight are defined as serious risk factors for KOA. Obesity has been shown to cause excessive mechanical stress on the knee joint, which can cause changes in the structure and mechanical properties of the articular cartilage as a result of this stress, resulting in cartilage erosion [53]. Clinically, those with BMI < 18 kg/m2 are accepted as underweight, those with 18–24.9 kg/m2 are accepted as normal weight, those with 25–29.9 kg/m2 are accepted as overweight, and those with 30–39.9 kg/m2 are accepted as obese, and those with > 40 kg/m2 are accepted as morbidly obese [54]. Regarding BMI, patients in both groups can be accepted as obese. In similar studies in the literature, it was determined that the BMI of the patients was over 30, that is, the patients were obese [51, 55]. The mean BMI findings of our study are consistent with the studies in the literature and support the view regarding the effect of obesity on KOA.
Pain is one of the most common symptoms in patients with KOA [56, 57]. The NRS was used to evaluate the severity of pain in our study. Before treatment, pain intensity was similar for both groups. Although pain intensity decreased in both groups after treatment, this decrease was not statistically significant in the control group. When the amount of decrease in the pain intensity after treatment was compared between the groups, it was determined that the amount of decrease in the pain intensity of the telerehabilitation group was statistically significantly higher than the control group. It is known that regular and correct exercise is effective in reducing pain in patients with KOA [14, 58, 59]. In this study, the patients in the telerehabilitation group did their exercises regularly and correctly through simultaneous video conference accompanied by a physiotherapist, the patients were shown the correct application of each exercise they did wrong. On the other side, only an exercise brochure was given to the control group. During the treatment period, the patients in the control group were not reminded to do the exercises. In addition, it is not known whether the exercises recommended to them are performed correctly by the patients with the appropriate number of repetitions and duration. The authors deduced the reason why the decrease in the pain intensity of the patients in the telerehabilitation group was higher than the patients in the control group is that the patients in the telerehabilitation group did their exercises more regularly and correctly. Considering similar studies in the literature, it has been reported that the severity of pain decreases with exercises performed through telerehabilitation [27, 48, 50, 52, 55, 60, 61]. In our study, the finding of a reduction in pain intensity with telerehabilitation is similar to the studies in the literature.
As mentioned above, pain is one of the most common findings in patients with KOA. The number of painkillers used by the two groups in the last 15 days before the treatment was similar. Although it was decreased for both groups, the statistical difference was found only in the telerehabilitation group. Comparing the groups for this parameter, the amount of decrease in the number of painkillers used in the last 15 days of the telerehabilitation group was statistically significantly higher than the control group. When similar studies in the literature were examined, it was reported that the number of painkillers used together with telerehabilitation decreased [28, 48]. Our finding regarding the number of painkillers used by the patients in our study was found to be compatible with other studies. Since the severity of pain decreased more in the telerehabilitation group, the decrease in the number of painkillers used by the patients in this group is an expected finding.
Physical function is affected due to the symptoms that occur in patients with KOA. In our study, physical function was evaluated with the 30 CST. Mean scores of this test were similar for both groups before treatment. After treatment, the mean score increased statistically significantly for both groups. However, the increase in the control group did not reach clinical significance. When the amount of increase in the 30 CST score after the treatment was compared between the groups, it was determined that the amount of increase in the score of the telerehabilitation group was statistically significantly higher than the control group. It is known that regular and correct exercises are effective in reducing symptoms in patients with KOA [62]. In addition, progressive strengthening exercises increase muscle strength [63]. The 30 CST is a physical performance test that also evaluates lower extremity muscle strength [64]. Therefore, an increase in the mean score for this test in patients in both groups in our study is an expected result. In this study, the patients in the telerehabilitation group did their exercises regularly and correctly through simultaneous video conference accompanied by a physiotherapist, the patients were shown the correct application of each exercise they did wrong, and the patients were warned by keeping a certain time for each exercise by a stopwatch. On the other hand, only a brochure was given to the control group. During the treatment period, the patients in the control group were not reminded to do the exercises. In addition, it is not known whether the exercises given to them are performed correctly by the patients with the appropriate number of repetitions and duration. Therefore, these results might be emerged due to the fact that the patients in the telerehabilitation group did their exercises more regularly and correctly. In similar studies in the literature, the result of the change in physical function through telerehabilitation differs. The finding related to physical function in our study is similar to the findings in the study of Gohir et al. and Nero et al. [48, 55] but differs from the finding in the study of Allen et al. [65]. Allen et al. [65] reported that the reason for this finding was due to the lower motivation of the participants in their own study compared to the participants in other studies.
The symptoms developing in patients with KOA affect the functional status of the patients. In our study, functional status was evaluated with KOOS. Before treatment, the total score of the questionnaire and scores for all sub-parameters were similar for both groups. When compared with before treatment, there was a statistically significant difference for both the total score and all sub-parameters of the questionnaire for the telerehabilitation group after the treatment, while a statistically significant difference was found only in the functions in daily living activities sub-parameter in the control group. When the functional status was compared between the post-treatment groups, it was found that the telerehabilitation group had statistically significantly better scores than the control group. It is an expected result that the functional status of the patients in the telerehabilitation group improved as a result of a significant decrease in the severity of pain and an increase in their physical functions. In addition, as mentioned before, the authors think this is due to the fact that the patients in the telerehabilitation group do their exercises more regularly and correctly. In similar studies in the literature, the evaluation of functional status and the effect of telerehabilitation on functional status vary. Functional status was evaluated with KOOS in some studies and with WOMAC in other studies. KOOS includes all of the questions of WOMAC and addresses functional status more comprehensively than WOMAC. When the studies in the literature were examined, the findings obtained for the functional status in our study were similar to the results of the study conducted by Brooks et al. [28], Allen et al. [65], Gohir et al. [55], and Aily et al. [61].
In chronic diseases, as a result of the presence of symptoms such as pain and the limitation of the physical functions of the patients and their activities in daily living activities, emotional status changes can be seen in the patients. In our study, emotional status was evaluated with the HADS. Before treatment, anxiety and depression subparameters and total scores of the questionnaire were similar for both groups. It was determined that there was a statistically significant difference for both the sub-parameters and the total score of the questionnaire for both groups after the treatment when compared with the pre-treatment. In the present study, when the emotional status was compared between the post-treatment groups, it was found that the emotional status was statistically significantly better in the telerehabilitation group compared to the control group. It is an expected result that the emotional status of the patients in the telerehabilitation group improved as a result of the decrease in pain intensity and improvement in physical function and functional status. Additionally, the first evaluation of all patients participating in the study was made during the pandemic process. However, for some patients, the evaluations were made after the end of the treatment which coincides with the end of the restrictions. Recalling the psychological effects of the pandemic on patients, it is thought that the end of the restrictions has also positively affected the emotional status of the patients in the control group. In the study of Bossen et al. [27], emotional status was evaluated with the HADS. As a result of the evaluation made at the 3rd month after the treatment, no statistically significant difference was found between the treatment and control groups in terms of emotional status. As a result of the evaluation made at the 12th month, a statistically significant difference was found in the anxiety level of the treatment group compared to the control group. When similar studies in the literature were scanned, it was determined that emotional status was evaluated only in the study by Bossen et al. [27]. The result of our study is not exactly similar to the results of the study performed by Bossen et al. [27]. The authors think this is because of the fact that there was a pandemic during the process of this study, and the emotional status of the patients was affected due to the restrictions imposed by the government.
Kinesiophobia has been investigated in various patient populations to date and has been found to be associated with increased pain, psychosocial problems, and physical disability [66]. Kinesiophobia is also a condition encountered in patients with KOA. In our study, kinesiophobia was evaluated with the TKS. Before treatment, kinesiophobia scores were similar for both groups. According to the TKS, those who score 13–22 “kinesiophobia is not at the clinical level (subclinical),” those who score 23–32 “mild,” those who score 33–42 “moderate,” and those who score 43–52 “severe” [67]. According to this classification, the patients in both the control group and telerehabilitation group in our study initially had severe kinesiophobia. It was determined that there was a statistically significant difference in terms of kinesiophobia score for both groups after treatment when compared with before treatment. When kinesiophobia was compared between the post-treatment groups, it was found that kinesiophobia was statistically significantly better in the telerehabilitation group than in the control group. It is an expected result that kinesiophobia decreases more as a result of the decrease in pain intensity of the patients and the improvement in their physical function, functional status, and emotional status in the telerehabilitation group compared to the patients in the control group. There is no study in the literature evaluating the effect of telerehabilitation on kinesiophobia in patients with KOA. This study makes a contribution to the literature in terms of evaluating the effect of telerehabilitation on kinesiophobia in patients with KOA.
Almost half of the individuals with OA experience fatigue and are more likely to suffer from fatigue compared to healthy individuals. In studies in the literature, it has been reported that many parameters such as aging, increased pain, psychosocial problems, decreased physical activity, and muscle strength may be related to fatigue in patients with OA. In our study, fatigue was evaluated using the FSS. Fatigue scores were similar for both groups before treatment. There was a statistically significant difference in the severity of fatigue in the telerehabilitation group when compared with the pre-treatment after treatment, but not in the control group. When the severity of fatigue was compared between the post-treatment groups, it was found that the fatigue was statistically significantly better in the telerehabilitation group compared to the control group. The authors think this is due to the fact that the intensity of pain decreased more, physical functions and functional status increased more, and emotional status improved more in the individuals in the telerehabilitation group compared to the control group. In similar studies, fatigue was assessed using the NRS or VAS [27, 52]. When the results of these studies are examined, the findings of fatigue severity in our study are similar to the results of these studies.
Physical activity level might be affected by disease-related symptoms, kinesiophobia, and fatigue in patients with KOA. In our study, physical activity level was evaluated with the IPAQ-SF. Physical activity scores were similar for both groups before treatment. There was a statistically significant difference in the level of physical activity in the telerehabilitation group when compared to the pre-treatment level after the treatment, but not in the control group. When the physical activity level was compared between the post-treatment groups, it was found that the level of physical activity in the telerehabilitation group was statistically significantly better than the control group. The authors deduce that this is due to the fact that the severity of pain, kinesiophobia, and fatigue of the individuals decreased more and their physical functions and functional and emotional status improved more in the telerehabilitation group compared to the individuals in the control group. In similar studies, physical activity level was evaluated with different methods such as accelerometer [47], SQUASH Questionnaire [60], and Physical Activity Score [27, 65]. When the results of these studies are examined, our results are similar to the long-term (12 months) results of the studies conducted by Bossen [27] and Allen et al. [65]. However, in another study by Bossen et al. [60] in which patients were evaluated at the 6th and 12th weeks, and in the study of Kloek et al. [47], in which the patients were followed up for long term (12 months), no statistically significant difference was found in the physical activity result compared to the pre-treatment. The authors think the difference between the physical activity results in this study and the mentioned studies in the literature is due to the fact that the patients were educated before the treatment and the importance of physical activity was mentioned during the patient education. In addition, while the telerehabilitation group was treated simultaneously with video conference, the physiotherapist answered the questions of the patients on this subject and may have been effective in the emergence of these results.
The quality of the physiotherapy received by the patients was evaluated with the QUIPA tool after the treatment. In the present study, it was determined that there was a statistically significant difference between the two groups for all sub-parameters and the total score of the QUIPA. According to these results, it was determined that the telerehabilitation group found the quality of the physiotherapy they received statistically significantly higher than the control group. Before the treatment, both groups were given the patient education which explains KOA, its symptoms, the progress of the disease, the effects of the disease on the patients, the units that patients should apply when they are affected, suggestions to the patients in order not to increase the severity of the disease, and the tools they could use to increase the functions in daily life. All the explained information in patient education met the answers to all the questions of the QUIPA tool. The patients in the telerehabilitation group were able to ask questions regarding the information they learned in the patient education to the physiotherapist during the simultaneous video conference. Thus, their knowledge was current and more advanced. This can be the explanation of why the QUIPA results of the patients in the telerehabilitation group were higher than the QUIPA results of the patients in the control group in the post-treatment evaluation. Umapathy et al. [51] evaluated the change in the appropriateness of care received by the participants in their study using the Osteoarthritis Quality Indicator Questionnaire [68]. According to this questionnaire, those who received telerehabilitation from a website for 12 months reported significant improvements in self-management and weight reduction compared to those who did not receive it. The questionnaire used in the study of Umapathy et al. [51] does not only evaluate the treatment quality in terms of physiotherapy but also has questions about pharmacological treatment modalities [68]. In the literature, there is no study evaluating only the quality of physiotherapy with telerehabilitation in patients with KOA. This study is the first to evaluate the quality of physiotherapy received with telerehabilitation in patients with KOA and makes a contribution to the literature in this respect.
Patients’ compliance with exercise was evaluated with the EARS after treatment. In this study, it was determined that there was a statistically significant difference between the two groups for the subscale C and the total score of the questionnaire, but no significant difference was found between the two groups for the subscale B. Subscale B reports compliance with exercise by the patient. Since the patients in both the treatment and control groups stated that they did their exercises, it is an expected finding that there is no difference when the two groups are compared in terms of part B. Considering the total score, it was found that the telerehabilitation group’s adherence to exercise was statistically significantly higher than the control group. It is not a surprising result that the exercise compliance of the patients followed by the physiotherapist is high. In similar studies in the literature, exercise adherence was evaluated with NRS [69] besides EARS [61]. The findings of both of these studies regarding exercise adherence were similar to the findings of our study in terms of this parameter.
In the present study, the satisfaction levels of the patients with the treatment were evaluated by the answers given by the patients to the 5-point Likert Scale to the question “What is your satisfaction level with the treatment?” While 100% of the patients in the telerehabilitation group stated that they were very satisfied or satisfied with the treatment, 58.3% of the patients in the control group stated that they were very satisfied or satisfied. As a result of this study, it was determined that the level of satisfaction with the treatment of the telerehabilitation group was statistically significantly higher than the control group. In similar studies in the literature, the level of satisfaction with the treatment of patients was questioned by a questionnaire [28] or using NRS [69]. The results of this study regarding patients’ level of satisfaction with the treatment was similar to the results of the study of Brooks et al. [28]; however, it was not compatible with the study of Bennell et al. [69]. For this parameter, the authors think the reason for the similarity with the study by Brooks et al. [28] is that the treatment duration for both studies was 8 weeks. However, the treatment duration was 3 weeks, namely, shorter, in the study of Bennell et al. [69].
This is the first study to evaluate the efficacy of physiotherapy and rehabilitation through simultaneous video conference in the presence of a physiotherapist. Moreover, this is the first study to evaluate the change in the level of kinesiophobia due to KOA after the telerehabilitation intervention and the quality of the physiotherapy received by the patients through telerehabilitation. The authors consider the lack of double blind study design to be a limitation of this study.
All in all, as a result of this study it can be concluded that telerehabilitation is superior to self-management. No harm was reported in individuals in either group. Findings from this study indicate that telerehabilitation is a quality practice with the potential to reduce symptoms in patients. For this reason, the authors believe that the findings of this study will not only contribute to the literature but also shed light on people working in this field. Evaluation of the effect of simultaneous telerehabilitation performed with a physiotherapist in terms of cost and effectiveness on the health system is recommended in future studies.
References
Arden NK, Leyland K (2013) Osteoarthritis year 2013 in review: clinical. Osteoarthr Cartil 21(10):1409–1413
Cross M et al (2014) The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73(7):1323–1330
Bernetti A et al (2021) New viscoelastic hydrogel hymovis MO. RE. Single intra-articular injection for the treatment of knee osteoarthritis in sportsmen: safety and efficacy study results. Front Pharmacol 12:673988
Bernetti A et al (2020) Evaluation of the efficacy of intra-articular injective treatment with reticular hyaluronic acid (Mo. Re. Technology) in amateur athletes with over-use gonarthrosis. Med Sport 73(1):127–39
Xie SH et al (2020) The feasibility and effectiveness of internet-based rehabilitation for patients with knee osteoarthritis: a study protocol of randomized controlled trial in the community setting. Medicine 99(44):e22961
Dunlop DD et al (2003) The costs of arthritis. Arthritis Care Res: Off J Am Coll Rheumatol 49(1):101–113
Glyn-Jones S et al (2015) Osteoarthritis. Lancet 386(9991):376–387
Wolfe F (1999) Determinants of WOMAC function, pain and stiffness scores: evidence for the role of low back pain, symptom counts, fatigue and depression in osteoarthritis, rheumatoid arthritis and fibromyalgia. Rheumatology (Oxford) 38(4):355–361
Stubbs B et al (2016) Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing 45(2):228–235
Alaca N (2019) The relationships between pain beliefs and kinesiophobia and clinical parameters in Turkish patients with chronic knee osteoarthritis: a cross-sectional study. J Pak Med Assoc 69(6):823–827
Bartholdy C et al (2020) Changes in physical inactivity during supervised educational and exercise therapy in patients with knee osteoarthritis: a prospective cohort study. Knee 27(6):1848–1856
Suzuki Y et al (2019) Patients with early-stage knee osteoarthritis and knee pain have decreased hip abductor muscle strength while descending stairs. Clin Rheumatol 38(8):2249–2254
Bernad-Pineda MJ, Heras-Sotos dL, Garcés-Puentes M (2014) Quality of life in patients with knee and hip osteoarthritis. Rev Esp Cir Ortop Traumatol (English Edition) 58(5):283–289
Hochberg MC et al (2012) American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 64(4):465–474
Pisters MF et al (2007) Long-term effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review. Arthritis Care Res 57(7):1245–1253
Roddy E et al (2005) Evidence-based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee—the MOVE consensus. Rheumatology 44(1):67–73
Bennell KL, Hinman RS (2011) A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport 14(1):4–9
Fransen M et al (2015) Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med 49(24):1554–1557
Thomas K et al (2002) Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ 325(7367):752
Van Baar M et al (2001) Effectiveness of exercise in patients with osteoarthritis of hip or knee: nine months’ follow up. Ann Rheum Dis 60(12):1123–1130
Hunter DJ (2010) Quality of osteoarthritis care for community-dwelling older adults. Clin Geriatr Med 26(3):401–417
Mudge S, Stretton C, Kayes N (2014) Are physiotherapists comfortable with person-centred practice? An autoethnographic insight. Disabil Rehabil 36(6):457–463
Bodenheimer T, Pham HH (2010) Primary care: current problems and proposed solutions. Health Aff 29(5):799–805
Theodoros D, Russell T, Latifi R (2008) Telerehabilitation: current perspectives. Stud Health Technol Inform 131(1):191–210
Russell TG et al (2011) Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. JBJS 93(2):113–120
Rini C et al (2015) Automated, internet-based pain coping skills training to manage osteoarthritis pain: a randomized controlled trial. Pain 156(5):837
Bossen D et al (2013) Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: randomized controlled trial. J Med Internet Res 15(11):e2662
Brooks MA et al (2014) Web-based therapeutic exercise resource center as a treatment for knee osteoarthritis: a prospective cohort pilot study. BMC Musculoskelet Disord 15(1):1–11
Wang X et al (2019) Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord 20(1):1–17
Association WM (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310(20):2191–2194
Altman R et al (1986) Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum: Off J Am Coll Rheumatol 29(8):1039–1049
Ertekin YH (2018) Turkish adaptation of the Physical Activity Readiness Questionare for Everyone (PAR-Q+). Fam Pract Palliat Care 3(1):52–64
Richmond SA et al (2013) Are joint injury, sport activity, physical activity, obesity, or occupational activities predictors for osteoarthritis? A systematic review. J Orthop Sports Phys Ther 43(8):515–519
Roos EM et al (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2):88–96
Downie W et al (1978) Studies with pain rating scales. Ann Rheum Dis 37(4):378–381
Güzeldemir M (1995) Ağrı değerlendirme yöntemleri. Sendrom 7(6):11–21
Craig CL et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395
Aydemir O (1997) Hastane anksiyete ve depresyon olcegi Turkce formunun gecerlilik ve guvenilirligi. Turk Psikiyatri Derg 8:187–280
Teo PL et al (2020) Patient-reported quality indicators to evaluate physiotherapy care for hip and/or knee osteoarthritis-development and evaluation of the QUIPA tool. BMC Musculoskelet Disord 21(1):1–11
Yilmaz ÖT et al (2011) Tampa Kinezyofobi Ölçeği’nin Türkçe versiyonu ve test-tekrar test güvenirliği. Fiz Rehabil 22(1):44–49
Newman-Beinart NA et al (2017) The development and initial psychometric evaluation of a measure assessing adherence to prescribed exercise: the Exercise Adherence Rating Scale (EARS). Physiotherapy 103(2):180–185
Armutlu K et al (2007) The validity and reliability of the Fatigue Severity Scale in Turkish multiple sclerosis patients. Int J Rehabil Res 30(1):81–85
Joshi A et al (2015) Likert scale: explored and explained. Br J Appl Sci Technol 7(4):396
Kul S (2014) Uygun istatistiksel test seçim kilavuzu/guideline for suitable statistical test selection. Plevra Bülteni 8(2):26
Dunlop DD et al (2011) Physical activity levels and functional performance in the osteoarthritis initiative: a graded relationship. Arthritis Rheum 63(1):127–136
Loeser RF, Collins JA, Diekman BO (2016) Ageing and the pathogenesis of osteoarthritis. Nat Rev Rheumatol 12(7):412–420
Kloek CJ et al (2018) Cost-effectiveness of a blended physiotherapy intervention compared to usual physiotherapy in patients with hip and/or knee osteoarthritis: a cluster randomized controlled trial. BMC Public Health 18(1):1–12
Nero H, Dahlberg J, Dahlberg LE (2017) A 6-week web-based osteoarthritis treatment program: observational quasi-experimental study. J Med Internet Res 19(12):e9255
Wright EA et al (2010) Impact of knee osteoarthritis on health care resource utilization in a US population-based national sample. Med Care 48(9):785
Dahlberg LE et al (2016) A web-based platform for patients with osteoarthritis of the hip and knee: a pilot study. JMIR Res Protoc 5(2):e5665
Umapathy H et al (2015) The web-based osteoarthritis management resource my joint pain improves quality of care: a quasi-experimental study. J Med Internet Res 17(7):e4376
Lorig KR et al (2008) The internet-based arthritis self-management program: a one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Care Res: Off J Am Coll Rheumatol 59(7):1009–1017
Lee R, Kean WF (2012) Obesity and knee osteoarthritis. Inflammopharmacology 20(2):53–58
Sowers M et al (2009) Knee osteoarthritis in obese women with cardiometabolic clustering. Arthritis Care Res 61(10):1328–1336
Gohir SA et al (2021) Effectiveness of internet-based exercises aimed at treating knee osteoarthritis: the iBEAT-OA randomized clinical trial. JAMA Netw Open 4(2):e210012–e210012
O’Neill TW, Felson DT (2018) Mechanisms of osteoarthritis (OA) pain. Curr Osteoporos Rep 16(5):611–616
Creamer P, Lethbridge-Cejku M, Hochberg MC (1998) Where does it hurt? Pain localization in osteoarthritis of the knee. Osteoarthr Cartil 6(5):318–323
Bennell KL, Dobson F, Hinman RS (2014) Exercise in osteoarthritis: moving from prescription to adherence. Best Pract Res Clin Rheumatol 28(1):93–117
Legha A et al (2020) Do comorbidities predict pain and function in knee osteoarthritis following an exercise intervention, and do they moderate the effect of exercise? Analyses of data from three randomized controlled trials. Musculoskelet Care 18(1):3–11
Bossen D et al (2013) The usability and preliminary effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis. BMC Med Inform Decis Mak 13(1):1–8
Aily JB et al (2020) Telerehabilitation for knee osteoarthritis in Brazil: a feasibility study. Int J Telerehabilitation 12(2):137
Fransen M et al (2015) Exercise for osteoarthritis of the knee. Br J Sports Med 49(24):1554–1557
Baker KR et al (2001) The efficacy of home based progressive strength training in older adults with knee osteoarthritis: a randomized controlled trial. J Rheumatol 28(7):1655–1665
Bohannon RW (1995) Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills 80(1):163–166
Allen K et al (2018) Physical therapy vs internet-based exercise training for patients with knee osteoarthritis: results of a randomized controlled trial. Osteoarthr Cartil 26(3):383–396
Sánchez-Herán Á et al (2016) Postural stability in osteoarthritis of the knee and hip: analysis of association with pain catastrophizing and fear-avoidance beliefs. PM&R 8(7):618–628
Neblett R et al (2016) Establishing clinically meaningful severity levels for the Tampa Scale for Kinesiophobia (TSK-13). Eur J Pain 20(5):701–710
Blackburn S et al (2016) Patient-reported quality indicators for osteoarthritis: a patient and public generated self-report measure for primary care. Res Involv Engagem 2(1):1–20
Bennell KL et al (2019) Does a web-based exercise programming system improve home exercise adherence for people with musculoskeletal conditions?: a randomized controlled trial. Am J Phys Med Rehabil 98(10):850–858
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tore, N.G., Oskay, D. & Haznedaroglu, S. The quality of physiotherapy and rehabilitation program and the effect of telerehabilitation on patients with knee osteoarthritis. Clin Rheumatol 42, 903–915 (2023). https://doi.org/10.1007/s10067-022-06417-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06417-3