Abstract
Objective
To evaluate the performance of the Gout-calculator in a cohort of consecutive acute arthritis affecting large and intermediate joints (without an attack on hallux or midfoot joints).
Methods
A retrospective study. Gout-calculator data were collected in medical records of patients included in the prospective consecutive cohort of acute arthritis called SYNOLACTATE. The diagnosis of gout was defined by the presence of sodium urate crystals in synovial fluid. The diagnostic performance of the Gout-calculator was studied by performing an ROC curve with the calculation of its AUC (95% CI) as well as the calculation of Sensitivity (Se), Specificity (Sp), and positive likelihood ratio (LR+).
Results
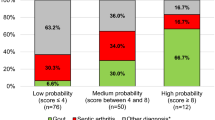
170 patients with acute arthritis were included. Variables associated with the diagnosis of gout were as follows: serum uric acid > 350 μmol/L (OR 5.52 (2.52–12.1), p < 0.001), joint redness (OR 5.08 (1.85–14.0), p = 0.001), previous patient-reported arthritis attack (OR 4.04 (1.92–8.49), p < 0.001), male (OR 3.00 (1.17–7.69), p = 0.02), hypertension or cardiovascular disease (OR 2.33 (1.07–5.06), p = 0.03). The median (IQR) of Gout-calculator was significantly higher in gouty arthritis (7.0 [5.5–8.1]) than in associated-CPP acute arthritis (4.0 [2.0–5.8]), septic arthritis (3.0 [2.0–5.1]), or others arthritis (3.5 [2.0–5.5]). The AUC was 0.833 (0.768–0.897) with for the threshold ≥ 8, a Se at 27.5% (0.161–0.428), Sp 97.7% (0.934–0.992), and LR+ 11.9 (3.5-40).
Conclusion
Despite diagnostic performances close to those published, the use of the Gout-calculator is not sufficient for the diagnosis of gout or to exclude the differential diagnosis of septic arthritis in the SYNOLACTATE cohort.
Key Points: • For a Gout-calculator threshold of ≤ 4, Sensitivity is 92.5%, Specificity 50.8% and LR− 0.15 to the gout diagnosis. • For a Gout-calculator threshold of > = 8, Sensitivity is 27.5%, Specificity 97.7% and LR+ 11.9 to the gout diagnosis. • In a population of acute arthritis affecting large joints, Gout-calculator is not sufficient to discriminate between gouty arthritis and septic arthritis. |


Similar content being viewed by others
Data availability
The cohort database is supervised by GC and OB. Data are available upon reasonable request. All data relevant to the study are included in the article.
References
Richette P, Doherty M, Pascual E, Barskova V, Becce F, Castañeda-Sanabria J, Coyfish M, Guillo S, Jansen TL, Janssens H, Lioté F, Mallen C, Nuki G, Perez-Ruiz F, Pimentao J, Punzi L, Pywell T, So A, Tausche AK, Uhlig T, Zavada J, Zhang W, Tubach F, Bardin T (2017) 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis 76(1):29–42
Dalbeth N, Merriman TR, Stamp LK (2016) Gout. Lancet 388(10055):2039–2052
Janssens HJ, Fransen J, van de Lisdonk EH, van Riel PL, van Weel C, Janssen M (2010) A diagnostic rule for acute gouty arthritis in primary care without joint fluid analysis. Arch Intern Med 170(13):1120–1126
Kienhorst LB, Janssens HJ, Fransen J, Janssen M (2015) The validation of a diagnostic rule for gout without joint fluid analysis: a prospective study. Rheumatology (Oxford) 54(4):609–614
Prior-Español Á, García-Mira Y, Mínguez S, Martínez-Morillo M, Gifre L, Mateo L (2019) Coexistence of septic and crystal-induced arthritis: a diagnostic challenge. A report of 25 cases. Reumatol Clin 15(6):e81–e85
Yu KH, Luo SF, Liou LB, Wu YJ, Tsai WP, Chen JY, Ho HH (2003) Concomitant septic and gouty arthritis--an analysis of 30 cases. Rheumatology (Oxford) 42(9):1062–1066
Berthoud O, Coiffier G, Albert JD, et al. (2020) Performance of a new rapid diagnostic test the lactate/glucose ratio of synovial fluid for the diagnosis of septic arthritis [published online ahead of print, 2020 Mar 29]. Joint Bone Spine. 2020;S1297-319X(20)30045-2. https://doi.org/10.1016/j.jbspin.2020.03.009
Pollet S, Coiffier G, Albert JD, Chales G, Guggenbuhl P, Perdriger A (2015) Concordance between fresh joint fluid analysis by the rheumatologist and joint fluid analysis at the laboratory: prospective single-center study of 180 samples. Joint Bone Spine 82(3):161–165
Newberry SJ, FitzGerald JD, Motala A et al (2017) Diagnosis of gout: a systematic review in support of an american college of physicians clinical practice guideline. Ann Intern Med 166(1):27–36
Lee SK, Jung JY, Jee WH, Lee JJ, Park SH (2019) Combining non-contrast and dual-energy CT improves diagnosis of early gout. Eur Radiol 29(3):1267–1275
Zhang Q, Gao F, Sun W, Ma J, Cheng L, Li Z (2018) The diagnostic performance of musculoskeletal ultrasound in gout: a systematic review and meta-analysis. PLoS One. 13(7):e0199672
Pattamapaspong N, Vuthiwong W, Kanthawang T, Louthrenoo W (2017) Value of ultrasonography in the diagnosis of gout in patients presenting with acute arthritis. Skeletal Radiol 46(6):759–767
Ogdie A, Taylor WJ, Neogi T, Fransen J, Jansen TL, Schumacher HR, Louthrenoo W, Vazquez-Mellado J, Eliseev M, McCarthy G, Stamp LK, Perez-Ruiz F, Sivera F, Ea HK, Gerritsen M, Cagnotto G, Cavagna L, Lin C, Chou YY, Tausche AK, Lima Gomes Ochtrop M, Janssen M, Chen JH, Slot O, Lazovskis J, White D, Cimmino MA, Uhlig T, Dalbeth N (2017) Performance of ultrasound in the diagnosis of gout in a multicenter study: comparison with monosodium urate monohydrate crystal analysis as the gold standard. Arthritis Rheumatol 69(2):429–438
Pascart T, Grandjean A, Norberciak L, Ducoulombier V, Motte M, Luraschi H, Vandecandelaere M, Godart C, Houvenagel E, Namane N, Budzik JF (2017) Ultrasonography and dual-energy computed tomography provide different quantification of urate burden in gout: results from a cross-sectional study. Arthritis Res Ther 19(1):171
Wang Y, Deng X, Xu Y, Ji L, Zhang Z (2018) Detection of uric acid crystal deposition by ultrasonography and dual-energy computed tomography: a cross-sectional study in patients with clinically diagnosed gout. Medicine (Baltimore) 97(42):e12834
Bongartz T, Glazebrook KN, Kavros SJ, Murthy NS, Merry SP, Franz WB 3rd et al (2015) Dual-energy CT for the diagnosis of gout: an accuracy and diagnostic yield study. Ann Rheum Dis 74(6):1072–1077
Yu Z, Mao T, Xu Y, Li T, Wang Y, Gao F, Sun W (2018) Diagnostic accuracy of dual-energy CT in gout: a systematic review and meta-analysis. Skeletal Radiol 47(12):1587–1593
Acknowledgments
All authors would like to thank the patients who participated in this study.
Author information
Authors and Affiliations
Contributions
GC, OB, AJD, FR, and SC included patients, conducted inclusion visits, performed joint puncture, analyzed results and statistics, and wrote the manuscript; GJA performed microbiologic analysis on synovial fluid, analyzed results and statistics, and wrote the manuscript; BC performed biochemist analysis on synovial fluid, analyzed results and statistics, and wrote the manuscript; PG supervised the progress of the study, analyzed results and statistics, and wrote the manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Ethical approval information
All patients were informed of the objectives and procedures of the study and gave their consent. The study was approved by the ethics committee of Rennes university hospital (Avis no. 16.96, September 2016).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Robin, F., Berthoud, O., Albert, J.D. et al. External validation of Gout-calculator performance on a cohort of acute arthritis (SYNOLACTATE) sparing distal joints such as hallux and midfoot. A cross-sectional study of 170 patients. Clin Rheumatol 40, 1983–1988 (2021). https://doi.org/10.1007/s10067-020-05382-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05382-z