Abstract
Objective
To evaluate the value of interleukin-6 (IL-6) in predicting long-term disease prognosis for Takayasu arteritis (TA).
Methods
Sixty-seven TA patients, who had IL-6 levels detected at the first visit and had a regular follow-up of at least 2 years, were enrolled. Data recorded up to March 31, 2019, including clinical presentations, laboratory indices, treatments, and radiological images were collected and used for analysis. The value of IL-6 in predicting disease relapse and imaging progression was analyzed.
Results
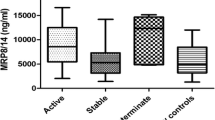
IL-6 levels were positively related with disease activity index, including Kerr scores, C-reactive protein (CRP) levels. Patients were divided into three groups according to baseline serum IL-6 levels: low group (< 5.4 pg/mL, n = 29), medium group (5.4–11.5 pg/mL, n = 20), and high group (> 11.5 ng/mL, n = 18). Patients in the medium and high group had higher disease activity than those in the low group (p < 0.01). Baseline IL-6 levels were correlated with luminal stenosis (p < 0.05), although no significant correlations with long-term imaging progression were observed. Patients with more than 2 episodes of disease relapses were most commonly seen in the medium group (p < 0.05). Multivariate Cox proportional hazard regression analysis indicated that medium and high IL-6 levels were positive predictors for disease relapse (HR 4.3, 95%CI 1.3–18.7 p = 0.07 for medium group; HR 2.1, 95% CI 0.7–48.9, p = 0.19 for high group) with disease status and treatment adjusted.
Conclusions
IL-6 may be a valuable predictor of TA disease relapse during long-term follow-up. Treatments targeted at IL-6 pathways might reduce disease relapse and have better prognostic effects for TA.
Key Points • Positive relationships between IL-6 levels and disease activity index, including Kerr scores, C-reactive protein (CRP) levels, etc. were indicated. • Medium and high baseline IL-6 levels were valuable for predicting disease relapse during the 2-year follow-up. • Baseline IL-6 levels were positively correlated with luminal stenosis on imaging. |


Similar content being viewed by others
References
Yang L, Zhang H, Jiang X, Zou Y, Qin F, Song L, Guan T, Wu H, Xu L, Liu Y, Zhou X, Bian J, Hui R, Zheng D (2014) Clinical manifestations and long-term outcome for patients with Takayasu arteritis in China. J Rheumatol 41:2439–2446
Yilmaz N, Can M, Oner FA, Kalfa M, Emmungil H, Karadag O, Yildiz F, Kimyon G, Yilmazer B, Gerdan V, Bilge SY, Ilhan B, Cobankara V, Kasifoglu T, Cefle A, Kisacik B, Onat AM, Akar S, Onen F, Erken E, Kiraz S, Aksu K, Keser G, Mumcu G, Direskeneli H (2013) Impaired quality of life, disability and mental health in Takayasu’s arteritis. Rheumatology (Oxford) 52:1898–1904
Watanabe Y, Miyata T, Tanemoto K (2015) Current clinical features of new patients with Takayasu arteritis observed from a cross-country research in Japan: age and sex specificity. Circulation 132:1701–1709
Kerr FS, Hallahan CW, Gordano J et al (1994) Takayasu arteritis. Ann Intern Med 120:919–929
Misra R, Danda D, Rajappa SM, Ghosh A, Gupta R, Mahendranath KM, Jeyaseelan L, Lawrence A, Bacon PA, Indian Rheumatology Vasculitis (IRAVAS) group (2013) Development and initial validation of the Indian Takayasu clinical activity score (ITAS2010). Rheumatology (Oxford) 52:1795–1801
Alibaz-Oner F, Aydin SZ, Akar S, Aksu K, Kamali S, Yucel E, Karadag O, Ozer H, Kiraz S, Onen F, Inanc M, Keser G, Akkoc N, Direskeneli H (2015) Assessment of patients with Takayasu arteritis in routine practice with Indian Takayasu clinical activity score. J Rheumatol 42:1443–1447
Ma LY, Li CL, Ma LL et al (2019) Value of contrast-enhanced ultrasonography of the carotid artery for evaluating disease activity in Takayasu arteritis. Arthritis Res Ther 21:24
Chung JW, Kim HC, Choi YH, Kim SJ, Lee W, Park JH (2007) Patterns of aortic involvement in Takayasu arteritis and its clinical implications: evaluation with spiral computed tomography angiography. J Vasc Surg 45:906–914
Jiang L, Li D, Yan F, Dai X, Li Y, Ma L (2012) Evaluation of Takayasu arteritis activity by delayed contrast-enhanced magnetic resonance imaging. Int J Cardiol 155:262–267
Germano G, Monti S, Ponte C et al (2017) The role of ultrasound in the diagnosis and follow-up of large-vessel vasculitis: an update. Clin Exp Rheumatol 35(Suppl):194–198
Zhang X, Zhou J, Sun Y, Shi H, Ji Z, Jiang L (2018) 18F-FDG-PET/CT: an accurate method to assess the activity of Takayasu’s arteritis. Clin Rheumatol 37:1927–1935
Tamura N, Maejima Y, Tezuka D, Takamura C, Yoshikawa S, Ashikaga T, Hirao K, Isobe M (2017) Profiles of serum cytokine levels in Takayasu arteritis patients: potential utility as biomarkers for monitoring disease activity. J Cardiol 70:278–285
Sun Y, Ma L, Yan F, Liu H, Ding Y, Hou J, Jiang L (2012) MMP-9 and IL-6 are potential biomarkers for disease activity in Takayasu’s arteritis. Int J Cardiol 156:236–238
Matsuyama A, Sakai N, Ishigami M, Hiraoka H, Kashine S, Hirata A, Nakamura T, Yamashita S, Matsuzawa Y (2003) Matrix metalloproteinases as novel disease markers in Takayasu arteritis. Circulation 108:1469–1473
Ishihara T, Haraguchi G, Kamiishi T, Tezuka D, Inagaki H, Isobe M (2011) Sensitive assessment of activity of Takayasu's arteritis by pentraxin3, a new biomarker. J Am Coll Cardiol 57:1712–1713
Alibaz-Oner F, Aksu K, Yentur SP, Keser G, Saruhan-Direskeneli G, Direskeneli H (2016) Plasma pentraxin-3 levels in patients with Takayasu’s arteritis during routine follow-up. Clin Exp Rheumatol 34:s73–s76
Kong X, Sun Y, Ma L, Chen H, Wei L, Wu W, Ji Z, Ma L, Zhang Z, Zhang Z, Zhao Z, Hou J, Dai S, Yang C, Jiang L (2016) The critical role of IL-6 in the pathogenesis of Takayasu arteritis. Clin Exp Rheumatol 34:S21–S27
Gao Q, Lv N, Dang A et al (2019) Association of interleukin-6 and interleukin-10 expression, gene polymorphisms, and Takayasu arteritis in a Chinese Han population. Clin Rheumatol 38:143–148
Alibaz-Oner F, Yentur SP, Saruhan-Direskeneli G et al (2015) Serum cytokine profiles in Takayasu’s arteritis: search for biomarkers. Clin Exp Rheumatol 33:S 32–S 35
Pulsatelli L, Boiardi L, Assirelli E et al (2017) Interleukin-6 and soluble interleukin-6 receptor are elevated in larger-vessel vasculitis: a cross-sectional and longitudinal study. Clin Exp Rheumatol 103:102–110
Kong X, Ma L, Ji Z, Dong Z, Zhang Z, Hou J, Zhang S, Ma L, Jiang L (2018) Pro-fibrotic effect of IL-6 via aortic adventitial fibroblasts indicates IL-6 as a treatment target in Takayasu arteritis. Clin Exp Rheumatol 36:62–72
Chen R, Sun Y, Cui X, Ji Z, Kong X, Wu S, Huang Q, Dai X, Zhang S, Ma L, Jiang L (2019) Autophagy promotes aortic adventitial fibrosis via the IL-6/Jak1 signaling pathway in Takayasu’s arteritis. J Autoimmun 99:39–47
Arend WP, Michel BA, Bloch DA et al (1990) The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 33:1129–1134
Hata A, Noda M, Moriwaki R et al (1996) Angiographic findings of Takayasu arteritis: new classification. Int J Cardiol 54:155–163
Yao X, Huang J, Zhong H, Shen N, Faggioni R, Fung M, Yao Y (2014) Targeting interleukin-6 in inflammatory autoimmune disease and cancers. Pharmacol Ther 141:125–139
Manku S, Wong W, Luo Z, Seidman MA, Alabdurubalnabi Z, Rey K, Enns W, Avina-Zubieta JA, Shojania K, Choy JC (2018) IL-6 expression is correlated with increased T-cell proliferation and survival in the arterial wall in giant cell arteritis. Cardiovasc Pathol 33:55–61
Burja B, Feichtinger J, Lakota K, Thallinger GG, Sodin-Semrl S, Kuret T, Rotar Ž, Ješe R, Žigon P, Čučnik S, Mali P, Praprotnik S, Tomšič M, Hočevar A (2019) Utility of serological biomarkers for giant cell arteritis in a large cohort treatment-naïve patients. Clin Rheumatol 38:317–329
Kong X, Zhang X, Lv P et al (2018) Treatment of Takayasu arteritis with the IL-6R antibody tocilizumab vs. cyclophosphamide. Int J Cardiol 266:222–228
Sun Y, Ma L, Kong X et al (2017) Cyclophosphamide could be a better choice than methotrexate as induction treatment for patients with more severe Takayasu’s arteritis. Rheumatol Int 37:2019–2026
van Sleen Y, Sandovici M, Abdulahad WH et al (2019) Markers of angiogenesis and macrophage products for predicting disease course and monitoring vascular inflammation in giant cell arteritis. Rheumatology (Oxford). https://doi.org/10.1093/rheumatology/kez034
Yoshifuji H (2019) Pathophysiology of large vessel vasculitis and utility of interleukin-6 inhibition therapy. Mod Rheumatol 29:287–293
Koster MJ, Warrington KJ (2017) Giant cell arteritis: pathogenic mechanisms and new potential therapeutic targets. BMC Rheumatol 1:2
Low C, Conway R (2019) Current advances in the treatment of giant cell arteritis: the role of biologics. Ther Adv Musculoskelet Dis. https://doi.org/10.1177/1759720X19827222
Adler S, Reichenbach S, Gloor A et al (2019) Risk of relapse after discontinuation of tocilizumab therapy in giant cell arteritis. Rheumatology (Oxford) 58:1939–1643
Sun Y, Kong X, Wu S, Ma L, Yan Y, Lv P, Jiang L (2019) YKL-40 as a new biomarker of disease activity in Takayasu arteritis. Int J Cardiol 293:231–237
Loricera J, Bianco R, Hernandez JL et al (2016) Tocilizumab in patients with Takayasu arteritis: a retrospective study and literature review. Clin Exp Rheumatol 34:S44–S53
Mekinian A, Resche-Rigon M, Comarmond C, Soriano A, Constans J, Alric L, Jego P, Busato F, Cabon M, Dhote R, Estibaliz L, Koné-Paut I, Landron C, Lavigne C, Lioger B, Michaud M, Ruivard M, Sacre K, Gottenberg JE, Gaches F, Goulenok T, Salvarani C, Cacoub P, Fain O, Saadoun D, French Takayasu network (2018) Efficacy of tocilizumab in Takayasu arteritis: multicenter retrospective study of 46 patients. J Autoimmun 91:55–60
Funding
This work was supported by the National Natural Science Foundation of China (NSFC 81601398, NSFC 81771730, and NSFC 81801598).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, Y., Kong, X., Cui, X. et al. The value of interleukin-6 in predicting disease relapse for Takayasu arteritis during 2-year follow-up. Clin Rheumatol 39, 3417–3425 (2020). https://doi.org/10.1007/s10067-020-05066-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05066-8