Abstract
Chronic inflammation, such as that present in rheumatoid arthritis (RA) and psoriatic arthritis (PsA), leads to aberrations in bone remodeling, which is mediated by several signaling pathways, including the Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway. In this light, pro-inflammatory cytokines are now clearly implicated in these processes as they can perturb normal bone remodeling through their action on osteoclasts and osteoblasts at both intra- and extra-articular skeletal sites. As a selective inhibitor of JAK1 and JAK3, tofacitinib has the potential to play a role in the management of rheumatic diseases such as RA and PsA. Preclinical studies have demonstrated that tofacitinib can inhibit disturbed osteoclastogenesis in RA, which suggests that targeting the JAK-STAT pathway may help limit bone erosion. Evidence from clinical trials with tofacitinib in RA and PsA is encouraging, as tofacitinib treatment has been shown to decrease articular bone erosion. In this review, the authors summarize current knowledge on the relationship between the immune system and the skeleton before examining the involvement of JAK-STAT signaling in bone homeostasis as well as the available preclinical and clinical evidence on the benefits of tofacitinib on prevention of bone involvement in RA and PsA.
Key Points • Chronic inflammation in rheumatoid arthritis (RA) and psoriatic arthritis (PsA) leads to disturbances in bone remodeling • Bone remodeling is mediated by several signaling pathways, including the JAK-STAT pathway • Tofacitinib, a selective inhibitor of JAK1 and JAK3, is active in RA and PsA and may help limit systemic bone loss through inhibiting disturbed osteoclastogenesis • Clinical trials show that tofacitinib reduces articular bone erosion |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory rheumatic diseases, including rheumatoid arthritis (RA) and psoriatic arthritis (PsA), are characterized by disturbances in bone remodeling, the process by which the adult skeleton is continuously renewed in response to various stimuli [1]. In RA, erosion of articular bone and cartilage degradation leads to the deformity of peripheral joints and disability [2]. Bone erosion, which occurs rapidly, can be expected to affect 80% of RA patients within 1 year of diagnosis [3] and is correlated with the presence of prolonged, increased inflammation [4]. Patients with RA are also prone to periarticular and systemic bone loss, which further contributes to morbidity due to osteoporosis and fragility fractures [5,6,7]. Furthermore, as osteoporosis can facilitate the development of erosions, there is a close interrelationship between systemic and local bone loss [8, 9].
Bone erosions are also seen in the joints of patients with PsA, even if in a different scenario [10, 11]. In contrast with RA, PsA is characterized by the presence of new, abnormal bone deposition at the entheses, the insertion sites of tendons and ligaments into bone [10, 11]. Systemic bone involvement in PsA is less well-established than in RA [12, 13]. However, a recent population-based study in a longitudinal cohort showed a 7 to 26% higher incidence of fracture in patients with PsA and psoriasis, when compared with the general population [14]. Moreover, in those patients with both PsA and severe psoriasis, the risk for any fracture was comparable to that of patients with RA [14].
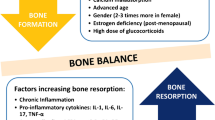
In healthy adults, bone homeostasis is maintained through a balance between the activity of osteoclasts (i.e., bone-resorbing cells) and osteoblasts (i.e., bone-forming cells) [1, 15]. The close relationship between the immune system and the skeleton is illustrated in several rheumatic diseases, where chronic inflammation perturbs this balance, leading to excessive bone resorption (RA and PsA), and to either excessive new bone formation locally (PsA) or blunted bone formation (RA) [7, 10, 16]. Growing interest in the role of this relationship in inflammatory rheumatic diseases has led to a new field of research known as “osteoimmunology” [17]. The effects of chronic inflammation on bone integrity are largely mediated by cytokines. The pro-inflammatory cytokines tumor necrosis factor (TNF)-α, interleukin (IL)-6, and IL-17 play key roles in pathologic bone resorption in RA [1, 18]. Intriguingly, TNF-α and IL-17 have been shown to inhibit or promote bone formation depending on the context [10]. In inflammatory arthropathies characterized by concurrent systemic bone loss together with entheseal inflammation leading to pathologic new bone formation, activation of the IL-17–IL-23 pathway has been reported to be a key player in its pathogenesis, as summarized in Fig. 1 [10, 19, 21].
The pathology of bone metabolism in rheumatoid arthritis (RA) and psoriatic arthritis (PsA). PsA proper pathways are indicated in red. ACPA anti-citrullinated protein antibody; IL interleukin; IFN interferon; mSC mesenchymal cell; OPG osteoprotegerin; RANK receptor activator of NF-κB; RANKL receptor activator of NF-κB ligand; TNF tumor necrosis factor
The Janus kinase (JAK)-signal transducer and activator of transcription (STAT) pathway is a key regulator of various mammalian cellular processes, including cytokine signal transduction, and this is also true in bone cells (Fig. 2 [20]) [22, 23]. Not surprisingly, members of the JAK family have become an attractive development target for orally administered, small-molecule inhibitors designed to treat a number of chronic inflammatory conditions [23, 24]. In this regard, tofacitinib, a selective inhibitor of JAK1 and JAK3 and, to a smaller degree, JAK2 [25], was the first targeted synthetic disease-modifying anti-rheumatic drug (DMARD) to be approved for the treatment of RA and more recently of PsA. In the Oral Rheumatoid Arthritis Trial (ORAL) and obesity prevention and lifestyle Oral Psoriatic Arthritis Trial (OPAL) programs [26,26,27,28,29,30,31,32,33,35], the large clinical development program that evaluated the efficacy and safety of tofacitinib alone or in combination with methotrexate in patient populations that included those refractory to standard therapy, tofacitinib was non-inferior to anti-TNF-α therapy (adalimumab) [28] and superior to methotrexate in treatment-naïve patients [30]. Positive effects of tofacitinib on radiographic disease progression have also been reported in clinical trials [30, 31, 33,33,35].
Schematic of signaling by type I/II cytokine receptors. While there are more than 200 secreted factors, many of which are referred to as cytokines, a smaller subset including interleukins (ILs), interferons (IFNs), colony-stimulating factors, and structurally related factors use a class of receptors designated type I and type II cytokine receptors. These receptors rely on Janus family kinases (JAKs) for intracellular signaling. Cytokine binding to the extracellular domain of receptors, activating JAKs, which in turn, phosphorylate (designated by “P”) multiple substrates including signal transducers and activators of transcription (STATs). STATs directly bind DNA and regulate gene expression. JAK inhibitors (Jakinibs) are small molecules that block cytokine signaling by directly interfering with JAK enzymatic activity [20]
In this review, we provide an overview of the effects of tofacitinib on bone damage in RA and PsA, briefly reviewing current knowledge of the relationship between the immune system and the skeleton before discussing the involvement of JAK-STAT signaling in bone homeostasis and the available preclinical and clinical evidence supporting the effects of tofacitinib on the prevention of bone involvement in RA and PsA.
Interactions between the immune system and the skeleton
The relationship between inflammation and the skeleton has been extensively investigated, and some of the signaling pathways involved in pathologic bone changes induced by chronic inflammation have been identified, especially in RA [7]. Normal bone remodeling is maintained through the highly coordinated activity of osteoclasts and osteoblasts essential in preventing a net loss or gain of bone [1, 36]. A number of factors contribute to the tight regulation of the interaction that occurs between osteoclasts and osteoblasts. Osteoblasts originate from mesenchymal cells; in contrast, osteoclasts are derived from hematopoietic stem cells [37, 38]. Osteoblasts control the synthesis and mineralization of bone while regulating osteoclast differentiation via the induction or production of various factors, including macrophage colony-stimulating factor, receptor activator of NF-κB ligand (RANKL) (a cytokine belonging to the TNF superfamily) [18], and osteoprotegerin (OPG) [1, 15, 39, 40]. RANKL is essential for osteoclastogenesis, as it interacts with the RANK receptor on osteoclast precursors, thereby promoting osteoclast differentiation, whereas OPG is a soluble decoy receptor produced by osteoblasts to prevent excessive bone resorption by binding RANKL and inhibiting osteoclast differentiation [1].
Macrophage colony-stimulating factor and RANKL are crucial for osteoclastogenesis; however, this process can also be enhanced by other cytokines. Among pro-inflammatory cytokines, the most important triggers of bone resorption in RA are TNF-α, IL-17, and IL-6 [18]. In joints affected by RA, inflamed synovial tissue (pannus) expands into cortical, subchondral, and trabecular bone causing erosion [1]. Evidence suggests that combinations of pro-inflammatory cytokines locally produced by synovial fibroblasts, macrophages, and lymphocytes from inflamed tissues induce the expression of RANKL and trigger osteoclastogenesis and bone loss [39, 41, 42]. For example, the successful treatment of RA with DMARDs was found to be associated with a reduction in the ratio between osteoclastogenic RANKL and its naturally occurring inhibitor OPG [39]. A later study showed that a combination of TNF-α and IL-6 was capable of inducing bone resorption in osteoclast-like multinuclear cells in vitro and in vivo [42].
A number of studies have suggested that pro-inflammatory cytokines also promote bone resorption by impairing the differentiation and function of osteoblasts [1, 16]. In RA, for example, pro-inflammatory cytokines have been implicated in the impairment of bone repair mechanisms mediated by osteoblasts and chondrocytes [18]. Of note, TNF-α is a potent inhibitor of osteoblast differentiation [18].
Wingless (Wnt) and the bone morphogenic protein (BMP) signaling pathways are also crucial for the regulation of osteoblast differentiation and function involved in the bone remodeling process [1]. The canonical Wnt pathway (the Wnt/ß-catenin pathway) induces osteoblast differentiation and ensures the maintenance of balanced bone resorption and formation [1]. Wnt signaling is blocked by a number of endogenous inhibitors, including members of the Dickkopf (DKK) family [1]. Among these, DKK1 has attracted considerable interest in recent years for its ability to inhibit bone formation by blocking Wnt signaling. In more detail, preclinical studies have shown that the overexpression of DKK1 causes osteopenia in mice, while reduced DKK1 expression is associated with high bone mass [43, 44]. Furthermore, altered serum levels of DKK1, reported in patients with inflammatory rheumatic diseases, including RA and ankylosing spondylitis, suggest the involvement of DKK1 in bone loss in inflammatory arthropathies [45,45,46,47,49].
Evidence has shown that the pro-inflammatory cytokine TNF, which is highly expressed in the synovium of inflamed RA joints, induces the expression of DKK1, which leads to the suppression of the Wnt pathway and the inhibition of new bone formation [18]. Thus, in RA, pro-inflammatory cytokines present in the inflamed bone microenvironment have detrimental effects on bone health not only because they induce osteoclastogenesis, but also because they impair new bone formation by osteoblasts [1]. In a recent small longitudinal study in patients with RA, treatment with an anti-TNF-α was associated with rapidly and significantly decreasing levels of serum DKK1, along with decreased bone resorption and increased bone formation [50].
Finally, it should be noted that, in RA, a strong predictor of bone erosion, besides inflammatory disease, is the presence of anti-citrullinated protein antibodies (ACPAs) [41]. The presence of ACPAs precedes the clinical onset of RA, and bone damage was demonstrated to develop before the clinical manifestations of RA in patients with ACPAs [51]. Moreover, an increased ACPA titer has been linked to a negative effect on systemic BMD, especially at femoral sites [52]. These observations highlight the fact that the loss of immune tolerance can have detrimental effects on bone and suggest that a close relationship exists between the adaptive immune system and the skeleton [41].
The absence of new bone formation in RA in response to pathologic resorption is one of the key differences between RA and PsA [10]. As pointed out above, in PsA, bone erosion coexists with excessive new bone formation [10]. While the factors responsible for bone loss in PsA are fairly well understood and overlapping with those involved in RA [53], at least in part, pathologic bone formation in PsA, which arises from aberrant osteoblast differentiation and function, is less well characterized [19]. Multiple signaling pathways (including the Wnt pathway) and pro-inflammatory cytokines (notably TNF-α and IL-17) have been shown to be involved [10]. In particular, a recent study addressing serum levels of Wnt pathway regulators in PsA found significantly lower levels of DKK1 in PsA patients compared with RA patients and healthy controls [54]. The highest levels of DKK1 were seen in RA patients, which might explain the distinct bone phenotype of RA (erosive) and PsA (erosive-proliferative) [54]. Recently, we observed a rapid increase in WNT signaling antagonists in patients with PsA treated with secukinumab, an anti-IL-17 antibody [55]. Differing from TNFα, IL-17 also promotes osteogenesis, particularly at inflamed sites, such as entheses, undergoing mechanical stress. In RA, where TNFα is the major pro-inflammatory cytokine, although overexpression of IL-17 also occurs, bone resorption largely predominates over bone formation. In contrast, the prevailing inflammatory cytokine in PsA is IL-17, which also promotes osteogenesis. Furthermore, in PsA and ankylosing spondylitis, where the involvement of entheses poor in osteoclasts is prevalent, excess formation of bone may even prevail over excess resorption of bone [21]. Data from clinical trials supports the difference in the pathophysiology of bone involvement in chronic arthritis: the use of anti-TNFα agents to control inflammation in PsA has not produced comparable effects on excess bone formation.
Considering the role of the IL-23/IL-17 axis in PsA, another cytokine that acts on osteoblasts downstream is IL-22. IL-22 is associated with bone formation and is present at elevated levels in the synovial fluid of patients with PsA, compared with those with osteoarthritis. In this setting, when IL-23 is overexpressed, IL-22 is upregulated, inducing osteoblast-related genes in the enthesis leading to new entheseal bone formation and osteoblast expansion. Recently, in vitro studies have shown enhancement of osteogenic differentiation in human mesenchymal stem cells following IL-22 exposure [56].
Involvement of the JAK-STAT pathway in bone metabolism
The JAK-STAT pathway is one of the numerous cytokine signaling pathways found in bone cells. Over the past few years, several studies have investigated the role of JAK-STAT signaling in osteoclastogenesis in animal models of RA, using specific inhibitors of the components of this pathway [57,57,59]. Of the seven known mammalian STAT proteins, STAT3 appears to be the most important transcription factor that mediates intracellular signaling in bone cells [22]. STAT3 mutations in humans have been found to increase both osteoclast number and bone resorption, leading to reduced bone mass and an increased incidence of bone fractures [22, 60, 61]. STA-21, a potent inhibitor of STAT3, was found to suppress arthritis in a mouse model of RA via regulatory effects on Th17 and Treg cells and to inhibit osteoclast formation [59]. The effects of STAT3 blockade were also investigated in a recent study with the STAT3 inhibitor Stattic [57]. By interfering with RANKL-induced STAT3 and NF-κB signaling, the inhibitor reduced osteoclastogenesis and bone loss both in vitro and in vivo. Another study investigated the effect of a JAK-2 inhibitor (AG490) on osteoclast differentiation in a murine osteoclast precursor cell line, wherein JAK-2 inhibition was associated with reduced RANKL-induced osteoclastogenesis [58]. A recent study in a mouse model of bone loss investigating WHI-131, a potent and specific small-molecule inhibitor of JAK3, showed that JAK3 inhibition might play a central role in bone remodeling via simultaneous inhibition of osteoclast differentiation and function and promotion of osteoblast differentiation [38].
In PsA, on the other hand, the innate immune pathway, which is predominantly mediated by neutrophils and mast cells, may be more relevant than the adaptive immune response mediated by Th17. In particular, the γδ T cells, a minor subset of T cells, have been shown to secrete IL-17, and are of importance in mucosal and epithelial tissue, where their role is to help to bridge innate and adaptive immunity. The majority of the production of IL-17 by γδ T cells follows stimulation by IL-23, but also occurs via IL-23-independent pathways [62]. Recently, IL-17A produced by γδ T cells was shown to increase the proliferation and osteoblastic differentiation of mesenchymal progenitor cells and to promote bone formation in IL-17A−/− mice [63]. Recent findings point to the JAK-STAT kinase signaling cascade being responsible for the regulation of activation and proliferation of IL-17 effector memory T cells, which suggest a potential role in the pathogenesis of PsA. Moreover, in PsA, IL-22 overexpression leads to the formation of new periosteal bone via STAT3 activation together with the increased expression of genes responsible for regulating bone formation, including members of the Wnt family [64]. In another inflammatory disease characterized by excessive bone formation, namely ankylosing spondylitis, IL-17A has been found to be involved in osteoblast differentiation through the JAK2/STAT3 pathway [65].
Besides cytokines, there are also other mediators that influence bone, among which the metabolic and endocrine molecules such as parathormone, fibroblast growth factor 23 (FGF23), growth hormone, and vitamin D. JAK-STAT pathways are also involved in some of these mechanisms. FGF23 has been found to be increased in a mouse model of postmenopausal osteoporosis, together with increased phosphorylation of JAK2, STAT1, and STAT3. In the same model, antibodies against FGF23 or AG490 compound (an inhibitor of JAK2/STAT1) were able to increase osteoformation markers such as osteocalcin [66]. Interestingly, calcification can be inhibited in situations of ectopic ossification such as spinal cord injury with the use of ruxolitinib (a JAK1/2 inhibitor) and in aortic valve with tofacitinib [67, 68].
Effects of tofacitinib on bone remodeling in RA and PsA
There are several potential ways in which tofacitinib affects bone remodeling, suggesting a favorable net outcome on bone in both RA and PsA, as summarized in Fig. 3. These include direct effects on bone signaling, effects on cytokines and immune cells, and the RANKL-OPG axis, as well as acting on non-immune pathways involving growth factors.
Preclinical evidence
A study in rats with adjuvant-induced arthritis (AIA), an in vivo model for addressing early events in RA, investigated the role of JAK inhibition with tofacitinib on osteoclast-mediated bone resorption; the study also investigated the effects of tofacitinib on RANKL production by human T lymphocytes and on the differentiation of human osteoclasts [69]. After 7 days of treatment with tofacitinib, edema, inflammation, and osteoclast-mediated bone resorption were all substantially reduced in AIA rats. The reported effects correlated with a reduction in the numbers of CD3+, CD68/ED-1+, and RANKL+ cells in rat paws; levels of IL-6 in both transcript and protein rapidly reduced within 4 h of tofacitinib administration, while the decrease in RANKL levels was slower (within 4–7 days). Tofacitinib had no effect on human osteoclast differentiation or function; however, a dose-dependent decrease in RANKL production was observed in human T lymphocytes. These findings indicate that tofacitinib may suppress osteoclast-mediated structural damage in the arthritic joint by decreasing the expression of RANKL.
A recent study in AIA rats assessed, for the first time, the impact of tofacitinib treatment on bone microstructure using micro-CT images [70]. This study is of particular relevance because most available evidence comes from studies assessing intra-articular bone, while data on the effects of tofacitinib on extra-articular bone are lacking. In the study, an adjuvant-induced animal model of arthritis, comprehensive structural and functional bone analysis was used to demonstrate that arthritis severely affected morphometric parameters in trabecular and cortical bone. A 22-day treatment with tofacitinib, initiated in the clinically overt phase of arthritis, was unable to reverse the changes in microarchitectural bone parameters, but was associated with increased hardness in cortical and trabecular bone. A decrease in the secretion of the osteoclast-stimulating cytokines TNF-α and IL-17 and inhibitory effects on bone resorption due to improved RANKL to OPG ratio were also observed [71].
Preliminary data from a study investigating the impact of tofacitinib on bone regeneration, including recruitment of human mesenchymal stromal cells, and chondrogenesis, osteogenesis, and osteoclastogenesis, have shown that tofacitinib may contribute to bone healing by promoting bone formation and reducing bone resorption in a model of fracture-like tissue environment [72].
Evidence from clinical studies
The 24-month phase III ORAL scan study assessed structural preservation, benefits in reducing the signs and symptoms of RA, and parameters of physical functioning following 24 months of treatment with tofacitinib at a twice-daily dose of 5 and 10 mg in patients with RA who had an inadequate response to methotrexate treatment [31]. Tofacitinib improved the signs and symptoms of RA and was associated with statistically significant improvements in physical function. The study also highlighted the potential of tofacitinib to reduce the progression of structural joint damage; both doses of tofacitinib resulted in lower rates of progression from baseline in both components of the van der Heijde modified total Sharp score (erosion score and joint space narrowing score) versus placebo at months 6 and 12. After 6 and 12 months of treatment, similar proportions of patients in both tofacitinib groups were without evidence of radiographic progression (defined as a ≤ 0.5 unit increase from baseline in the van der Heijde modified total Sharp score), with significant differences versus placebo for both tofacitinib groups. Furthermore, at month 12, the proportion of patients without progression in erosion score (≤ 0.5 increase from baseline) was significantly greater in the two tofacitinib treatment groups, compared with placebo.
The ORAL Start study compared tofacitinib monotherapy with methotrexate monotherapy in RA patients not previously treated with methotrexate [30]. Overall, 958 patients were randomized to receive one of three regimens: twice-daily tofacitinib 5 or 10 mg, or methotrexate at a starting dose of 10 mg per week, incrementally increased to 20 mg per week over 8 weeks. The co-primary endpoints at month 6 were mean change from baseline in the van der Heijde modified total Sharp score and the proportion of patients with an ACR70 response. At 6 months, mean changes from baseline van der Heijde modified total Sharp scores were significantly lower in the two tofacitinib groups than in patients receiving methotrexate. However, in all three groups, the changes were modest; 0.2 points in the tofacitinib 5 mg group, < 0.1 point in the tofacitinib 10 mg group, and 0.8 points in the methotrexate group (p < 0.001 for both comparisons). Twenty-five-point five percent of patients receiving tofacitinib 5 mg and 37.7% receiving tofacitinib 10 mg had an ACR70 response at month 6, versus 12.0% of methotrexate recipients (p < 0.001 for both comparisons). Notably, monotherapy with tofacitinib was superior to methotrexate in inhibiting structural joint damage progression and reducing the signs and symptoms of RA in patients not previously treated with methotrexate. Post-hoc analysis of the ORAL Start and ORAL Scan studies investigated the relationship between levels of disease activity with tofacitinib, long-term radiographically determined structural progression, and patient-reported parameters of physical functioning [73]. Of interest, tofacitinib was shown to inhibit joint damage regardless of disease activity, even in the presence of persistent inflammation, a finding that might support a direct effect on bone unrelated to inflammation control.
A randomized exploratory study in 109 patients with RA investigated the progression of structural damage using, for the first time, three different MRI techniques [74]. Besides the comprehensive range of highly sensitive MRI endpoints, the study also used the validated RAMRIS (RA MRI score) technique [75], as well as novel quantitative techniques. Significant differences in RA MRI score bone marrow edema score were seen after 6 months for both tofacitinib alone and when combined with methotrexate [74]. Moreover, differences in quantitative RA MRI score synovitis were significant by month 3. Therefore, treatment with tofacitinib 10 mg, both as monotherapy or combined with methotrexate, was associated with an early reduction of inflammation and reduced progression of bone erosion.
As for the potential role of tofacitinib in preventing systemic bone loss, the available clinical data are very limited. A small study explored the early effects on bone homeostasis in 14 RA patients treated with tofacitinib, with a focus on osteoclast regulating factors [76]. The study was the first to show that tofacitinib improves inflammatory bone metabolism via the regulation of serum RANKL levels and serum RANKL/OPG ratio in RA. Based on the findings from a previous study in RA showing that tofacitinib regulates synovitis through the inhibition of IL-17 secretion by CD4+ T cells and IL-6 secretion by synovial fibroblasts, the authors hypothesized that tofacitinib controls RANKL induction through inhibition of IL-17 and IL-6 production in the inflamed synovium [77].
With regard to the effects of tofacitinib on bone in patients with PsA, data related to radiographic disease progression are just beginning to emerge. The OPAL Broaden trial assessed radiographic disease progression in PsA patients treated for 12 months with twice-daily tofacitinib 5 mg, twice-daily tofacitinib 10 mg, or adalimumab 40 mg once every 2 weeks, all added to background conventional synthetic DMARDs [78]. Radiographic non-progression was defined as an increase from baseline in van der Heijde-modified total Sharp score for PsA ≤ 0.5, ≤ 0, or ≤ 0.66. At 12 months, > 90% of patients treated with tofacitinib or adalimumab did not show any radiographic progression. Changes in radiographic scores were minimal and influenced by baseline levels of C-reactive protein (CRP). The ongoing long-term extension trial OPAL Balance will provide further information on the effects of tofacitinib on the radiographic progression of PsA [79].
Discussion
The effects of chronic inflammation on cells responsible for bone integrity are complex and mediated by several signaling pathways, including the JAK-STAT pathway. By acting on osteoclasts as well as osteoblasts at intra- as well as extra-articular skeletal sites, pro-inflammatory cytokines perturb normal bone remodeling. Data showing that tofacitinib can inhibit unbalanced osteoclastogenesis in RA suggests that targeting the JAK-STAT pathway may halt bone erosion, which is supported by encouraging results in RA and PsA, where tofacitinib has been shown to reduce articular bone erosion. Emerging insights into the effects of tofacitinib on the main pathogenetic factors, including IL-17, IL-22, bone morphogenetic proteins, and WNT inhibitors, may further differentiate bone resorption and repair mechanisms in these diseases. However, further clinical study is needed to fully characterize the role of tofacitinib in preventing systemic bone loss in RA and PsA, and in the important treatment goal of preventing pathologic bone formation at the entheses in PsA.
References
Baum R, Gravallese EM (2014) Impact of inflammation on the osteoblast in rheumatic diseases. Curr Osteoporos Rep 12:9–16
Smolen JS, Aletaha D, McInnes IB (2016) Rheumatoid arthritis. Lancet 388:2023–2038
van der Heijde DM (1995) Joint erosions and patients with early rheumatoid arthritis. Br J Rheumatol 34(Suppl 2):74–78
Visser H, le Cessie S, Vos K, Breedveld FC, Hazes JM (2002) How to diagnose rheumatoid arthritis early: a prediction model for persistent (erosive) arthritis. Arthritis Rheum 46:357–365
Gough AK, Lilley J, Eyre S, Holder RL, Emery P (1994) Generalised bone loss in patients with early rheumatoid arthritis. Lancet 344:23–27
Schett G, Gravallese E (2012) Bone erosion in rheumatoid arthritis: mechanisms, diagnosis and treatment. Nat Rev Rheumatol 8:656–664
Shim JH, Stavre Z, Gravallese EM (2018) Bone loss in rheumatoid arthritis: basic mechanisms and clinical implications. Calcif Tissue Int 102:533–546
Rossini M, Adami G, Viapiana O, Idolazzi L, Orsolini G, Fassio A, Giollo A, Gatti D (2017) Osteoporosis: an independent determinant of bone erosions in rheumatoid arthritis? J Bone Miner Res 32:2142–2143
Rossini M, Bagnato G, Frediani B, Iagnocco A, G LAM, Minisola G, Caminiti M, Varenna M, Adami S (2011) Relationship of focal erosions, bone mineral density, and parathyroid hormone in rheumatoid arthritis. J Rheumatol 38:997–1002
Paine A, Ritchlin C (2018) Altered bone remodeling in psoriatic disease: new insights and future directions. Calcif Tissue Int 102:559–574
Schett G (2014) Bone formation in psoriatic arthritis: a report from the GRAPPA 2013 annual meeting. J Rheumatol 41:1218–1219
Chandran S, Aldei A, Johnson SR, Cheung AM, Salonen D, Gladman DD (2016) Prevalence and risk factors of low bone mineral density in psoriatic arthritis: a systematic review. Semin Arthritis Rheum 46:174–182
Gulati AM, Michelsen B, Diamantopoulos A, Grandaunet B, Salvesen O, Kavanaugh A, Hoff M, Haugeberg G (2018) Osteoporosis in psoriatic arthritis: a cross-sectional study of an outpatient clinic population. RMD Open 4:e000631
Ogdie A, Harter L, Shin D, Baker J, Takeshita J, Choi HK, Love TJ, Gelfand JM (2017) The risk of fracture among patients with psoriatic arthritis and psoriasis: a population-based study. Ann Rheum Dis 76:882–885
McInnes IB, Schett G (2011) The pathogenesis of rheumatoid arthritis. N Engl J Med 365:2205–2219
Walsh NC, Reinwald S, Manning CA, Condon KW, Iwata K, Burr DB, Gravallese EM (2009) Osteoblast function is compromised at sites of focal bone erosion in inflammatory arthritis. J Bone Miner Res 24:1572–1585
Takayanagi H (2007) Osteoimmunology: shared mechanisms and crosstalk between the immune and bone systems. Nat Rev Immunol 7:292–304
Harre U, Schett G (2017) Cellular and molecular pathways of structural damage in rheumatoid arthritis. Semin Immunopathol 39:355–363
Gravallese EM, Schett G (2018) Effects of the IL-23-IL-17 pathway on bone in spondyloarthritis. Nat Rev Rheumatol 14:631–640
Gadina M et al. (2018) Translational and clinical advances in JAK-STAT biology: The present and future of jakinibs. J Leukoc Biol 104(3):499–514
Rossini M, Viapiana O, Adami S, Idolazzi L, Fracassi E, Gatti D (2016) Focal bone involvement in inflammatory arthritis: the role of IL17. Rheumatol Int 36:469–482
Li J (2013) JAK-STAT and bone metabolism. JAKSTAT 2:e23930
O'Shea JJ, Schwartz DM, Villarino AV, Gadina M, McInnes IB, Laurence A (2015) The JAK-STAT pathway: impact on human disease and therapeutic intervention. Annu Rev Med 66:311–328
Fragoulis GE, McInnes IB, Siebert S (2019) JAK-inhibitors. New players in the field of immune-mediated diseases, beyond rheumatoid arthritis. Rheumatology (Oxford) 58:i43–i54
Hodge JA, Kawabata TT, Krishnaswami S, Clark JD, Telliez JB, Dowty ME, Menon S, Lamba M, Zwillich S (2016) The mechanism of action of tofacitinib-an oral Janus kinase inhibitor for the treatment of rheumatoid arthritis. Clin Exp Rheumatol 34:318–328
Burmester GR, Blanco R, Charles-Schoeman C, Wollenhaupt J, Zerbini C, Benda B, Gruben D, Wallenstein G, Krishnaswami S, Zwillich SH, Koncz T, Soma K, Bradley J, Mebus C, Oral Step investigators (2013) Tofacitinib (CP-690,550) in combination with methotrexate in patients with active rheumatoid arthritis with an inadequate response to tumour necrosis factor inhibitors: a randomised phase 3 trial. Lancet 381:451–460
Fleischmann R, Kremer J, Cush J, Schulze-Koops H, Connell CA, Bradley JD, Gruben D, Wallenstein GV, Zwillich SH, Kanik KS, Investigators OS (2012) Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. N Engl J Med 367:495–507
Fleischmann R, Mysler E, Hall S, Kivitz AJ, Moots RJ, Luo Z, DeMasi R, Soma K, Zhang R, Takiya L, Tatulych S, Mojcik C, Krishnaswami S, Menon S, Smolen JS, Investigators OS (2017) Efficacy and safety of tofacitinib monotherapy, tofacitinib with methotrexate, and adalimumab with methotrexate in patients with rheumatoid arthritis (ORAL strategy): a phase 3b/4, double-blind, head-to-head, randomised controlled trial. Lancet 390:457–468
Kremer J, Li ZG, Hall S, Fleischmann R, Genovese M, Martin-Mola E, Isaacs JD, Gruben D, Wallenstein G, Krishnaswami S, Zwillich SH, Koncz T, Riese R, Bradley J (2013) Tofacitinib in combination with nonbiologic disease-modifying antirheumatic drugs in patients with active rheumatoid arthritis: a randomized trial. Ann Intern Med 159:253–261
Lee EB, Fleischmann R, Hall S, Wilkinson B, Bradley JD, Gruben D, Koncz T, Krishnaswami S, Wallenstein GV, Zang C, Zwillich SH, van Vollenhoven RF, Investigators OS (2014) Tofacitinib versus methotrexate in rheumatoid arthritis. N Engl J Med 370:2377–2386
van der Heijde D, Tanaka Y, Fleischmann R, Keystone E, Kremer J, Zerbini C, Cardiel MH, Cohen S, Nash P, Song YW, Tegzova D, Wyman BT, Gruben D, Benda B, Wallenstein G, Krishnaswami S, Zwillich SH, Bradley JD, Connell CA, Investigators OS (2013) Tofacitinib (CP-690,550) in patients with rheumatoid arthritis receiving methotrexate: twelve-month data from a twenty-four-month phase III randomized radiographic study. Arthritis Rheum 65:559–570
van Vollenhoven RF, Fleischmann R, Cohen S, Lee EB, Garcia Meijide JA, Wagner S, Forejtova S, Zwillich SH, Gruben D, Koncz T, Wallenstein GV, Krishnaswami S, Bradley JD, Wilkinson B, Investigators OS (2012) Tofacitinib or adalimumab versus placebo in rheumatoid arthritis. N Engl J Med 367:508–519
Gladman D, Rigby W, Azevedo VF, Behrens F, Blanco R, Kaszuba A, Kudlacz E, Wang C, Menon S, Hendrikx T, Kanik KS (2017) Tofacitinib for psoriatic arthritis in patients with an inadequate response to TNF inhibitors. N Engl J Med 377:1525–1536
Mease P, Hall S, FitzGerald O, van der Heijde D, Merola JF, Avila-Zapata F, Cieslak D, Graham D, Wang C, Menon S, Hendrikx T, Kanik KS (2017) Tofacitinib or adalimumab versus placebo for psoriatic arthritis. N Engl J Med 377:1537–1550
Tofacitinib summary of product characteristics. Available at: https://www.ema.europa.eu/en/documents/product-information/xeljanz-epar-product-information_en.pdf. 27 Jun 2019
Boyce BF, Xing L (2008) Functions of RANKL/RANK/OPG in bone modeling and remodeling. Arch Biochem Biophys 473:139–146
Boyle WJ, Simonet WS, Lacey DL (2003) Osteoclast differentiation and activation. Nature 423:337–342
Cheon YH, Kim JY, Baek JM, Ahn SJ, Jun HY, Erkhembaatar M, Kim MS, Lee MS, Oh J (2016) WHI-131 promotes osteoblast differentiation and prevents osteoclast formation and resorption in mice. J Bone Miner Res 31:403–415
Haynes D, Crotti T, Weedon H, Slavotinek J, Au V, Coleman M, Roberts-Thomson PJ, Ahern M, Smith MD (2008) Modulation of RANKL and osteoprotegerin expression in synovial tissue from patients with rheumatoid arthritis in response to disease-modifying antirheumatic drug treatment and correlation with radiologic outcome. Arthritis Rheum 59:911–920
Teitelbaum SL (2000) Bone resorption by osteoclasts. Science 289:1504–1508
Harre U, Georgess D, Bang H, Bozec A, Axmann R, Ossipova E, Jakobsson PJ, Baum W, Nimmerjahn F, Szarka E, Sarmay G, Krumbholz G, Neumann E, Toes R, Scherer HU, Catrina AI, Klareskog L, Jurdic P, Schett G (2012) Induction of osteoclastogenesis and bone loss by human autoantibodies against citrullinated vimentin. J Clin Invest 122:1791–1802
Yokota K, Sato K, Miyazaki T, Kitaura H, Kayama H, Miyoshi F, Araki Y, Akiyama Y, Takeda K, Mimura T (2014) Combination of tumor necrosis factor alpha and interleukin-6 induces mouse osteoclast-like cells with bone resorption activity both in vitro and in vivo. Arthritis Rheumatol 66:121–129
Li J, Sarosi I, Cattley RC, Pretorius J, Asuncion F, Grisanti M, Morony S, Adamu S, Geng Z, Qiu W, Kostenuik P, Lacey DL, Simonet WS, Bolon B, Qian X, Shalhoub V, Ominsky MS, Zhu Ke H, Li X, Richards WG (2006) Dkk1-mediated inhibition of Wnt signaling in bone results in osteopenia. Bone 39:754–766
Morvan F, Boulukos K, Clement-Lacroix P, Roman Roman S, Suc-Royer I, Vayssiere B, Ammann P, Martin P, Pinho S, Pognonec P, Mollat P, Niehrs C, Baron R, Rawadi G (2006) Deletion of a single allele of the Dkk1 gene leads to an increase in bone formation and bone mass. J Bone Miner Res 21:934–945
Heiland GR, Appel H, Poddubnyy D, Zwerina J, Hueber A, Haibel H, Baraliakos X, Listing J, Rudwaleit M, Schett G, Sieper J (2012) High level of functional dickkopf-1 predicts protection from syndesmophyte formation in patients with ankylosing spondylitis. Ann Rheum Dis 71:572–574
Orsolini G, Adami G, Rossini M, Ghellere F, Caimmi C, Fassio A, Idolazzi L, Gatti D, Viapiana O (2018) Parathyroid hormone is a determinant of serum Dickkopf-1 levels in ankylosing spondylitis. Clin Rheumatol 37:3093–3098
Rossini M, Viapiana O, Adami S, Fracassi E, Idolazzi L, Dartizio C, Povino MR, Orsolini G, Gatti D (2015) In patients with rheumatoid arthritis, Dickkopf-1 serum levels are correlated with parathyroid hormone, bone erosions and bone mineral density. Clin Exp Rheumatol 33:77–83
Rossini M, Viapiana O, Idolazzi L, Ghellere F, Fracassi E, Troplini S, Povino MR, Kunnathully V, Adami S, Gatti D (2016) Higher level of Dickkopf-1 is associated with low bone mineral density and higher prevalence of vertebral fractures in patients with ankylosing spondylitis. Calcif Tissue Int 98:438–445
Wang SY, Liu YY, Ye H, Guo JP, Li R, Liu X, Li ZG (2011) Circulating Dickkopf-1 is correlated with bone erosion and inflammation in rheumatoid arthritis. J Rheumatol 38:821–827
Fassio A, Adami G, Gatti D, Orsolini G, Giollo A, Idolazzi L, Benini C, Vantaggiato E, Rossini M, Viapiana O (2019) Inhibition of tumor necrosis factor-alpha (TNF-alpha) in patients with early rheumatoid arthritis results in acute changes of bone modulators. Int Immunopharmacol 67:487–489
Kleyer A, Finzel S, Rech J, Manger B, Krieter M, Faustini F, Araujo E, Hueber AJ, Harre U, Engelke K, Schett G (2014) Bone loss before the clinical onset of rheumatoid arthritis in subjects with anticitrullinated protein antibodies. Ann Rheum Dis 73:854–860
Orsolini G, Caimmi C, Viapiana O, Idolazzi L, Fracassi E, Gatti D, Adami G, Rossini M (2017) Titer-dependent effect of anti-citrullinated protein antibodies on systemic bone mass in rheumatoid arthritis patients. Calcif Tissue Int 101:17–23
Shaw AT, Gravallese EM (2016) Mediators of inflammation and bone remodeling in rheumatic disease. Semin Cell Dev Biol 49:2–10
Fassio A, Idolazzi L, Viapiana O, Benini C, Vantaggiato E, Bertoldo F, Rossini M, Gatti D (2017) In psoriatic arthritis Dkk-1 and PTH are lower than in rheumatoid arthritis and healthy controls. Clin Rheumatol 36:2377–2381
Fassio A, Gatti D, Rossini M, Idolazzi L, Giollo A, Adami G, Gisondi P, Girolomoni G, Viapiana O (2019) Secukinumab produces a quick increase in WNT signalling antagonists in patients with psoriatic arthritis. Clin Exp Rheumatol 37:133–136
El-Zayadi AA, Jones EA, Churchman SM, Baboolal TG, Cuthbert RJ, El-Jawhari JJ, Badawy AM, Alase AA, El-Sherbiny YM, McGonagle D (2017) Interleukin-22 drives the proliferation, migration and osteogenic differentiation of mesenchymal stem cells: a novel cytokine that could contribute to new bone formation in spondyloarthropathies. Rheumatology (Oxford) 56:488–493
Li CH, Xu LL, Jian LL, Yu RH, Zhao JX, Sun L, Du GH, Liu XY (2018) Stattic inhibits RANKL-mediated osteoclastogenesis by suppressing activation of STAT3 and NF-kappaB pathways. Int Immunopharmacol 58:136–144
Li CH, Zhao JX, Sun L, Yao ZQ, Deng XL, Liu R, Liu XY (2013) AG490 inhibits NFATc1 expression and STAT3 activation during RANKL induced osteoclastogenesis. Biochem Biophys Res Commun 435:533–539
Park JS, Kwok SK, Lim MA, Kim EK, Ryu JG, Kim SM, Oh HJ, Ju JH, Park SH, Kim HY, Cho ML (2014) STA-21, a promising STAT-3 inhibitor that reciprocally regulates Th17 and Treg cells, inhibits osteoclastogenesis in mice and humans and alleviates autoimmune inflammation in an experimental model of rheumatoid arthritis. Arthritis Rheumatol 66:918–929
Holland SM, DeLeo FR, Elloumi HZ, Hsu AP, Uzel G, Brodsky N, Freeman AF, Demidowich A, Davis J, Turner ML, Anderson VL, Darnell DN, Welch PA, Kuhns DB, Frucht DM, Malech HL, Gallin JI, Kobayashi SD, Whitney AR, Voyich JM, Musser JM, Woellner C, Schaffer AA, Puck JM, Grimbacher B (2007) STAT3 mutations in the hyper-IgE syndrome. N Engl J Med 357:1608–1619
Minegishi Y, Saito M, Tsuchiya S, Tsuge I, Takada H, Hara T, Kawamura N, Ariga T, Pasic S, Stojkovic O, Metin A, Karasuyama H (2007) Dominant-negative mutations in the DNA-binding domain of STAT3 cause hyper-IgE syndrome. Nature 448:1058–1062
Cuthbert RJ, Watad A, Fragkakis EM, Dunsmuir R, Loughenbury P, Khan A, Millner PA, Davison A, Marzo-Ortega H, Newton D, Bridgewood C, McGonagle DG (2019) Evidence that tissue resident human enthesis gammadeltaT-cells can produce IL-17A independently of IL-23R transcript expression. Ann Rheum Dis 78:1559–1565
Ono T, Okamoto K, Nakashima T, Nitta T, Hori S, Iwakura Y, Takayanagi H (2016) IL-17-producing gammadelta T cells enhance bone regeneration. Nat Commun 7:10928
Sherlock JP, Joyce-Shaikh B, Turner SP, Chao CC, Sathe M, Grein J, Gorman DM, Bowman EP, McClanahan TK, Yearley JH, Eberl G, Buckley CD, Kastelein RA, Pierce RH, Laface DM, Cua DJ (2012) IL-23 induces spondyloarthropathy by acting on ROR-gammat+ CD3+CD4-CD8- entheseal resident T cells. Nat Med 18:1069–1076
Jo S, Wang SE, Lee YL, Kang S, Lee B, Han J, Sung IH, Park YS, Bae SC, Kim TH (2018) IL-17A induces osteoblast differentiation by activating JAK2/STAT3 in ankylosing spondylitis. Arthritis Res Ther 20:115
Xu L, Zhang L, Zhang H, Yang Z, Qi L, Wang Y, Ren S (2018) The participation of fibroblast growth factor 23 (FGF23) in the progression of osteoporosis via JAK/STAT pathway. J Cell Biochem 119:3819–3828
Alexander KA, Tseng HW, Fleming W, Jose B, Salga M, Kulina I, Millard SM, Pettit AR, Genet F, Levesque JP (2019) Inhibition of JAK1/2 tyrosine kinases reduces neurogenic heterotopic ossification after spinal cord injury. Front Immunol 10:377
Parra-Izquierdo I, Castanos-Mollor I, Lopez J, Gomez C, San Roman JA, Sanchez Crespo M, Garcia-Rodriguez C (2018) Calcification induced by type I interferon in human aortic valve interstitial cells is larger in males and blunted by a Janus kinase inhibitor. Arterioscler Thromb Vasc Biol 38:2148–2159
LaBranche TP, Jesson MI, Radi ZA, Storer CE, Guzova JA, Bonar SL, Thompson JM, Happa FA, Stewart ZS, Zhan Y, Bollinger CS, Bansal PN, Wellen JW, Wilkie DP, Bailey SA, Symanowicz PT, Hegen M, Head RD, Kishore N, Mbalaviele G, Meyer DM (2012) JAK inhibition with tofacitinib suppresses arthritic joint structural damage through decreased RANKL production. Arthritis Rheum 64:3531–3542
Vidal B, Cascao R, Finnila MAJ, Lopes IP, da Gloria VG, Saarakkala S, Zioupos P, Canhao H, Fonseca JE (2018) Effects of tofacitinib in early arthritis-induced bone loss in an adjuvant-induced arthritis rat model. Rheumatology (Oxford) 57:1461–1471
Bokarewa MI, Erlandsson MC (2018) Bone remodelling: locus minori or unappreciated potential of tofacitinib? Rheumatology (Oxford) 57:1318–1320
Gaber T, Brinkman A, Damerau A (2019) Tofacitinib promotes fundamental processes of bone healing. Ann Rheum Dis 78(suppl 2):A109
Strand V, Kavanaugh A, Kivitz AJ, van der Heijde D, Kwok K, Akylbekova E, Soonasra A, Snyder M, Connell C, Bananis E, Smolen JS (2018) Long-term radiographic and patient-reported outcomes in patients with rheumatoid arthritis treated with tofacitinib: ORAL Start and ORAL Scan post-hoc analyses. Rheumatol Ther 5:341–353
Conaghan PG, Ostergaard M, Bowes MA, Wu C, Fuerst T, van der Heijde D, Irazoque-Palazuelos F, Soto-Raices O, Hrycaj P, Xie Z, Zhang R, Wyman BT, Bradley JD, Soma K, Wilkinson B (2016) Comparing the effects of tofacitinib, methotrexate and the combination, on bone marrow oedema, synovitis and bone erosion in methotrexate-naive, early active rheumatoid arthritis: results of an exploratory randomised MRI study incorporating semiquantitative and quantitative techniques. Ann Rheum Dis 75:1024–1033
Dohn UM, Ejbjerg BJ, Hasselquist M, Narvestad E, Court-Payen M, Szkudlarek M, Moller J, Thomsen HS, Ostergaard M (2007) Rheumatoid arthritis bone erosion volumes on CT and MRI: reliability and correlations with erosion scores on CT, MRI and radiography. Ann Rheum Dis 66:1388–1392
Kitano M, Kitano S, Sekiguchi M, Azuma N, Hashimoto N, Tsunoda S, Matsui K, Sano H (2016) AB0394 early effect of tofacitinib on osteoclast regulator in rheumatoid arthritis [abstract]. Ann Rheum Dis 75:1040
Maeshima K, Yamaoka K, Kubo S, Nakano K, Iwata S, Saito K, Ohishi M, Miyahara H, Tanaka S, Ishii K, Yoshimatsu H, Tanaka Y (2012) The JAK inhibitor tofacitinib regulates synovitis through inhibition of interferon-gamma and interleukin-17 production by human CD4+ T cells. Arthritis Rheum 64:1790–1798
van der Heijde D, Gladman DD, FitzGerald O, Kavanaugh A, Graham D, Wang C, Fallon L (2019) Radiographic progression according to baseline C-reactive protein levels and other risk factors in psoriatic arthritis treated with tofacitinib or adalimumab. J Rheumatol 46:1089–1096
Nash P, Coates LC, Kivitz AJ Safety and efficacy of tofacitinib, an oral Janus kinase inhibitor, in patients with active psoriatic arthritis: interim data from OPAL Balance, an open-label, long-term extension study. ACR Annual Meeting 2017, Abstract #64778
Acknowledgments
Medical writing support was provided by Lorenza Lanini, an independent medical writer, on behalf of Health Publishing & Services Srl.
Funding
This work was funded by Pfizer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This is a review article for which ethical approval was not required.
Disclosures
Giovanni Orsolini and Maurizio Rossini received an honorarium from Pfizer in connection with the development of this manuscript. The authors declare they have no conflicts of interest in this work. Ilaria Bertoldi is a Pfizer employee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Orsolini, G., Bertoldi, I. & Rossini, M. Osteoimmunology in rheumatoid and psoriatic arthritis: potential effects of tofacitinib on bone involvement. Clin Rheumatol 39, 727–736 (2020). https://doi.org/10.1007/s10067-020-04930-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-04930-x