Abstract
Purpose
The emergency midline laparotomy is a commonly performed procedure with a burst abdomen being a critical surgical complication requiring further emergency surgery. This study aimed to investigate the clinical outcomes of patients with burst abdomen after emergency midline laparotomy.
Methods
A single-center, prospective, observational cohort study of patients undergoing emergency midline laparotomy during a two-year period was done. Abdominal wall closure followed a standardized technique using monofilament, slowly absorbable suture in a continuous suturing technique with a suture-to-wound ratio of at least 4:1. Treatment of burst abdomen was surgical. Data, including intra-hospital postoperative complications, were collected and registered chronologically based on journal entries. The primary outcome was to describe postoperative complications, length of stay, and the overall morbidity based on the Comprehensive Complication Index (CCI), stratified between patients who did and did not suffer from a burst abdomen during admission.
Results
A total of 543 patients were included in the final cohort, including 24 patients with burst abdomen during admission. The incidence of burst abdomen after emergency midline laparotomy was 4.4%. Patients with a burst abdomen had a higher total amount of complications per patient (median of 3, IQR 1.3–5.8 vs. median of 1, IQR 0.0–3.0; p = 0.001) and a significantly higher CCI (median of 53.0, IQR 40.3–94.8 vs. median of 21.0, IQR 0.0–42.0; p = < 0.001).
Conclusion
Patients with burst abdomen had an increased risk of postoperative complications during admission as well as a longer and more complicated admission with multiple non-surgical complications.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Each year, approximately one out of 1100 of the population undergo emergency laparotomy, often due to high-risk surgical conditions such as bowel obstruction, gastrointestinal perforation, mesenteric ischemia, or other high-risk surgical conditions [1, 2]. Due to the need for maximum visibility of the peritoneal cavity, midline laparotomy is most often the strategy of choice in the emergency setting. However, emergency laparotomy is also associated with high rates of mortality, morbidity, and postoperative complications [2,3,4].
Burst abdomen is defined as a deep wound rupture of the sutured abdominal midline aponeurosis. The rate of burst abdomen is reported as 3.8–28.0% in emergency surgery [3, 5, 6] and a lower rate of 0.2–5.0% in elective surgery [7,8,9,10]. It is regularly described as a severe complication due to increased mortality [11,12,13], low quality of life [14] and decreased survival [10]. Multiple studies have focused on the identification of patients at higher risk of burst abdomen, finding male sex, old age, frailty, and comorbidities such as obesity, tobacco use, alcohol abuse, and hypertension to be risk factors [3, 4, 6, 7, 11, 15,16,17]. Emergency surgery and closure techniques are known as non-patient-related risk factors [3, 4, 6, 7, 11, 15, 17,18,19,20,21,22], but newer studies have also focused on the quality of the midline aponeurosis [23]. Despite a greater focus on defining patients at risk and decreasing the rate of burst abdomen, no studies have elaborated upon why exactly burst abdomen is dangerous or what organ-specific complications lead to the more protracted and complicated course of admission for patients with burst abdomen.
We hypothesized that patients with a burst abdomen have higher rates of mortality and morbidity due to a higher tendency for complications during admission as well as a different pattern of organ-specific complications compared to patients without a burst abdomen. The aim of this prospective, observational cohort study was to investigate the clinical consequences of a burst abdomen after emergency midline laparotomy and fill a gap in the current literature.
Methods
This study is a single-center, prospective, observational cohort study of patients undergoing emergency midline laparotomy at Copenhagen University Hospital, Herlev, in the years 2021 and 2022. Copenhagen University Hospital, Herlev, is a specialized tertiary university hospital with an emergency catchment area of 465.000 patients. The surgical department performs approximately 450 emergency midline laparotomies and an estimated 100 elective midline laparotomies annually, as the majority of elective surgery is planned as minimally invasive surgery. An emergency laparotomy bundle-of-care approach was implemented in the department in 2017 for patients presenting with acute abdominal pain and clinical suspicion of high-risk surgical conditions [3, 4]. The bundle includes preoperative standardized protocols, a standardized intraoperative approach, and, since 2021, a dedicated and highly specialized ward for postoperative care [24,25,26].
The study was approved by the Capital Region of Demark (P-2020–1166, R-21038079) and the Danish Data Protection Agency (P-2021–431). The project did not qualify for ethics approval by Danish law, nor required informed consent, due to the observational nature of the study with no intervention or randomization carried out. The study was conducted and reported by The Reporting of Observational Studies in Epidemiology (STROBE) statement [27].
Abdominal wall closure and strategy of burst abdomen
In our department, closure of the abdominal wall after midline laparotomy has followed a standardized intraoperative strategy since June 2017 and has reduced the rate of burst abdomen since implementation [3, 4, 28]. Primary midline abdominal wall closure is carried out based on international recommendations, utilizing a slow-absorbable, monofilamentous suture in a continuous manner, taking small bites of 5–9 mm aponeurosis and small steps of 5 mm between each step securing a suture-to-wound ratio of at least 4:1 [3]. The abdominal wall closure technique is documented in the patient journal as a standard. Treatment of a burst abdomen is always intended surgically with the aim of early fascial closure, preferably at the first re-operation. A slow absorbable, monofilamenteous suture is used in a continuous manner taking large mass-closure bites of 2–3 cm with small steps of 5 mm between stitches [4]. Negative pressure wound therapy with or without mesh-mediated fascial traction is used in cases with unobtainable fascial closure and only until fascial closure is possible [4].
Data sources and management
Data were collected via the electronic journal system and included demographic data, American Society of Anaesthesiologists (ASA) score, the World Health Organization/Eastern Cooperative Oncology Group (WHO/ECOG) Performance Status [29], body mass index (BMI), pre-existing comorbidities, risk-factors such as tobacco- and alcohol habits, intra-hospital postoperative complications, length-of-stay, stay in the intensive care unit, and 30- and 90-day mortality. All complications were registered chronologically based on journal entries. Complications were placed within predefined subgroups based upon organ systems being surgical, wound-related, infectious, cerebral, pulmonary, cardiac, thromboembolic, renal, or other. All subgroups and individual complications are also described further in Supplementary Table 1. Complications were scored according to the Clavien-Dindo Classification, and a total score of the overall morbidity was conducted by the Comprehensive Complication Index [30].
Storage and management were performed using the REDCap (Research Electronic Data Capture) platform hosted at our department. The platform is a secure, web-based software designed to support data collection, storage, and management of research studies [31].
Participants and study size
Patients were evaluated for inclusion during a consecutive inclusion period from January 1st, 2021, to December 31st, 2022. Hereby expecting a study size of approximately 500–600 patients based on the annual normal in our hospital. Adult patients (≥ 18 years) undergoing emergency midline laparotomy during the study period were evaluated for inclusion. Patients were identified by reviewing the surgical log and the patient journals via our journal system (EPIC Hyperspace, Epic Systems Corp 2020). Patients who were underage (< 18 years) or had no Danish social security number were excluded. Patients in the group with burst abdomen were identified in the surgical log in case of surgical treatment of burst abdomen (after index emergency or emergent re-operation) or identified via the patient journal due to experiencing burst abdomen as a postoperative complication. Due to this design, burst abdomen was excluded as a complication in further analysis of complications between the groups.
Outcome measures
The primary outcome was to describe postoperative complications as well as overall morbidity based on the Comprehensive Complication Index (CCI) in our cohort, stratified between patients who did and did not suffer from a burst abdomen during admission. We aimed to describe the organ-specific complications in each group. Secondary outcomes included length-of-stay, stay in the intensive care unit during admission, days from primary operation to burst abdomen, and 30- and 90-day mortality.
Statistical analysis
Categorical data were presented as frequencies and percentages. To investigate differences in categorical variables, Pearson’s chi-squared test or two-tailed Fisher’s exact test was used depending on cell count. Continuous data were expressed as mean (standard deviation, SD) and median (interquartile range, IQR). The distribution of continuous data was assessed by visual inspection of histograms and QQ plots. Groups were compared with an unpaired t-test or a Mann–Whitney U test depending on the normality of data distribution. Missing data were reported (Table 1) and only occurred in the baseline data; BMI, Performance Status, tobacco- and alcohol habits. All statistical tests were two-sided. P values ≤ 0.05 were considered statistically significant. Statistical analyses were performed using IBM SPSS statistics for Windows Ver. 29.0.1.0.
Results
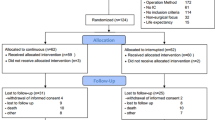
During the two-year study period, a total of 544 adult patients underwent emergency midline laparotomy in our department. One patient was excluded due to not fulfilling the inclusion criteria of having a Danish social security number allowing for follow-up. The final cohort consisted of 543 individual patients who were eligible for further analyses (Fig. 1). In the cohort, a total of 24 patients (4.4% of 543 patients) experienced a burst abdomen after emergency midline laparotomy. Eighteen (3.3%) patients had burst abdomen after an index emergency laparotomy and six (1.1%) patients from emergent re-operation after elective surgery.
The basic characteristics of the study population are outlined in Table 1. Baseline demographic variables were mostly comparable between the two groups, i.e. patients with a burst abdomen and patients without a burst abdomen, except for male sex being predominant among patients suffering from burst abdomen (18 of 24 patients, 72.0% vs. 255 of 519 patients, 49.1%; p = 0.020) as well as more often demonstrating a high ASA score of III-IV (5 of 24, 20.8% vs. 37 of 519, 7.1%; p = 0.031). We also found slight differences in atrial fibrillation being more common in the group without a burst abdomen (68 of 519, 13.1% vs. 0 of 24, 0.0%; p = 0.059) and chronic renal failure being more common in the group with a burst abdomen (3 of 24, 12.5% vs. 16 of 519, 3.1%; p = 0.046). There were no patients with missing data in the group with a burst abdomen. The group without a burst abdomen had minimal missing data of BMI, WHO Performance Status, tobacco use, and alcohol habits of 1.2%, 0.6%, 0.4%, and 0.8%, respectively.
Regarding the 24 patients with a burst abdomen, a total of 21 (87.5%) had a successful closure of the abdominal wall. Of the remaining three patients, one patient died before closure and two were not able to undergo further surgery and a conservative strategy was chosen instead. We found that the primary closure technique followed the standardized method in 23 (95.8%) patients and had a median suture-to-wound-ratio of 5:1 (minimum 4:1 and maximum 6:1). The standardized regimen with mass-closure technique was followed in 17 (70.9%) patients and a median suture-to-wound ratio was found to be 15:1 (minimum 10:1 and maximum 22:1). Data on abdominal wall closure for the patients with burst abdomen can be seen in Table 2.
An overview of clinical outcomes is listed in Table 3. In the group of patients with a burst abdomen, we found that 21 of 24 patients (87.5%) had postoperative complications other than burst abdomen during admission, which was seen to be an increased tendency compared to the 358 of 519 patients in the rest of the cohort (69.0%). Yet the data was not significant (p = 0.067). Patients with a burst abdomen had a higher total amount of complications per patient (median of 3 and IQR of 1.3–5.8 vs. median of 1 and IQR of 0.0–3.0; p = 0.001). Furthermore, the group with a burst abdomen also had a significantly higher Comprehensive Complication Index (CCI) than the rest of the cohort without a burst abdomen (median of 53.0 and IQR of 40.3–94.8 vs. median of 21.0 and IQR of 0.0–42.0; p = < 0.001) referring to an overall greater score of postoperative morbidity. The cumulative risk of complications was generally higher in the group with a burst abdomen, especially after the fifth postoperative day – and patients with a burst abdomen were found to have more complications on the eight postoperative day than the patients without a burst abdomen had on the 30th postoperative day (Fig. 2). For the group of patients with burst abdomen, we stratified the number and type of complications before and after burst abdomen, which is shown in Table 4. The median number of days from index surgery to burst abdomen was seven days (IQR 4.5–9.8 days). The patients tended to have approximately the same amount of overall complications before and after burst abdomen (median of 1 and IQR of 0.0–2.8 vs. median of 1 and IQR of 0.0–3.0). However, a difference was seen regarding CCI before and after burst abdomen, with an overall greater score of morbidity after burst abdomen (median 10.5 and IQR of 0.0–39.4 before vs., median of 41.6 and IQR of 0.0–90.0). Differences before and after burst abdomen were seen regarding some organ-specific complications, with the biggest differences seen in cardiac complications (1 of 24 patients, 4.2%, before and 6 of 24 patients, 25.0%, after). A schematic illustration of stay and outcomes for all patients with a burst abdomen is shown in Fig. 3.
Cumulative risk of complications in each group. Chart of the cumulative risk of complications for the group with burst abdomen (blue) and the rest of the cohort without burst abdomen (red). The x-axis shows postoperative days from day of surgery (day 0) to the 30th postoperative day. The y-axis shows the cumulative risk of complications as a ratio of each group (24 patients with burst abdomen and 519 patients without)
Schematic presentation of outcomes for patients with burst abdomen. Illustration of the individual stay and outcomes for all 24 patients with burst abdomen. The x-axis shows postoperative days from day of surgery (day 0) to the 30th postoperative day. The y-axis shows the individual patients from 1 to 24 in chronological order according to day of surgery. Icons illustrate outcomes during stay with cross indicating complications, lightning strike indicating day of burst abdomen, house indicating discharge from hospital and headstone indicating in-hospital mortality
Wound-related complications (9 of 24 patients, 37.5% vs. 69 of 519 patients, 13.3%; p = 0.004), pulmonary complications (11 of 24, 45.8% vs. 105 of 519, 20.2%; p = 0.005) and cardiac complications (7 of 24, 29.2% vs. 57 of 519, 11.0%; p = 0.015) were more common in the group with a burst abdomen compared to the group without. The distribution of organ-specific postoperative complications is listed in Supplementary Table 1. Patients with a burst abdomen suffered more from postoperative wound infection (4 of 24, 16.7% vs. 18 of 519, 3.5%; p = 0.013). Bronchospasm (3 of 24, 12.0% vs. 8 of 519, 1.5%; p = 0.010) and postoperative bowel obstruction occurred more often in patients with a burst abdomen (2 of 24, 8.3% vs. 5 of 519, 1.0%; p = 0.034). Excluding burst abdomen, we found no significant difference in surgical complications between the two groups (11 of 24, 45.8% vs. 143 of 519, 27.6%; p = 0.064).
Regarding postoperative mortality rates, a clinical but not significant difference was observed in patients with burst abdomen having a higher mortality rate at 30 days (5 of 24 patients, 20.8% vs. 59 of 519 patients, 11.4%; p = 0.186) and 90 days (7 of 24, 29.2% vs. 93 of 519, 17.9%; p = 0.178) after index surgery. Patients with a burst abdomen stayed longer before discharge (median stay of 22 days and IQR of 12.5–34.3 vs. median of 7 days and IQR of 5.0–13.0; p = < 0.001). The rate of admissions to the intensive care unit during admission were comparable between the two groups (7 of 24, 29.2% vs. 93 of 519, 17.9%; p = 0.178).
Discussion
In this prospective study of 543 patients undergoing emergency midline laparotomy from January 1st, 2021, to December 31st, 2022, we found that patients experiencing the surgical complication burst abdomen had an increased tendency to suffer from further cardiopulmonary and wound-related complications during admission and had an overall higher score of morbidity based on the Comprehensive Complication Index (CCI).
The rate of burst abdomen after index emergency midline laparotomy was 3.3%, which has remained constant since the standardization of our technique for midline abdominal wall closure after emergency surgery [3]. Including six patients suffering from burst abdomen after emergent re-operation, we had a total of 24 patients with burst abdomen in our cohort. This group had a greater total number of complications during admission and a clinically increased risk of complications in general. We found that the cumulative risk of complications was generally higher (as demonstrated in Fig. 2). This has not been previously described in the literature. Regarding organ-specific complications, wound-related and cardiopulmonary complications were notably high among patients suffering from burst abdomen. Surgical site occurrences (i.e. seroma, hematoma, infection, or rupture) are recognized as risk factors for the development of burst abdomen in the literature [7, 11, 13, 15,16,17, 32], and a higher incidence of these among patients with burst abdomen was somewhat expected. In our study, patients were equally likely to have wound complications before or after a burst abdomen. Furthermore, we found that burst abdomen mostly occurred on the seventh postoperative day, which correlates to earlier studies [33]. The event of a burst abdomen seemed to accelerate the rate of complications with an overall higher score of morbidity. This tendency is also shown in Fig. 2 with the cumulative risk having a steady rise in complications from the fifth to tenth postoperative day.
Closure of the abdominal wall of the patients with burst abdomen was successful in 87.5% of cases. Our standardized method of primary closure was followed in 95.8% of cases. It is known from the literature, that some patients might have an increased risk of burst abdomen prior to surgery. We found that male sex and high ASA scores were more common among patients suffering from burst abdomen compared to the rest of the cohort without burst abdomen. These are known risk factors for burst abdomen [3, 4, 15, 17] and a higher incidence was expected. We did not find any significant difference regarding BMI, age, WHO Performance Status, tobacco use, alcohol habits, or liver cirrhosis in our study. Yet, these have been described as risk factors in both the literature [3, 6, 7, 11, 15,16,17] and earlier studies from our group [23, 34, 35]. Patients at risk might benefit from an individualized closure technique. In recent years, studies have focused on the use of prophylactic mesh augmentation at the index laparotomy to reduce risk of a burst abdomen [36,37,38] and incisional hernia [37,38,39,40,41,42,43]. Results have been promising, but further studies are needed to investigate possible methods and identify which patients might benefit the most [28, 44]. Additionally, multiple risk factors for development of incisional hernia have been found including male sex, tobacco use, obesity, diabetes etc., but more data is needed [43, 45,46,47]. Patients with burst abdomen had a longer length of stay compared to the rest of the cohort. We observed no statistically significant variation in 30- or 90-day mortality rates; nevertheless, there was a discernible clinical distinction.
This prospective, observational cohort study does hold some limitations. Due to data selection from a two-year period and burst abdomen being a rare outcome, we do recognize that our sample size of patients with burst abdomen is small, with 24 cases. This, as well as our study being a single-center cohort study, results in some uncertainty regarding underpowering of data for comparisons as well as data being generalizable. Missing data regarding BMI, WHO Performance Status, tobacco use, and alcohol habits were 0.4–1.2%. However, as this is a prospective study conducted in a center serving a larger population in Denmark, we do believe our data represents a general tendency, although further studies with a larger sample size are needed. This study emphasizes a void in the current literature as to why exactly a burst abdomen is dangerous.
In conclusion, patients with burst abdomen have an increased risk of postoperative complications during admission as well as a longer and more complicated stay with multiple non-surgical complications. Further studies, preferably with larger sample sizes, are needed to confirm and elaborate upon our findings.
Data availability
Data are not publicly available due to being sensitive data but can be available in anonymized format on request to the corresponding author.
References
Shapter SL, Paul MJ, White SM (2012) Incidence and estimated annual cost of emergency laparotomy in England: is there a major funding shortfall? Anaesthesia 67:474–478. https://doi.org/10.1111/j.1365-2044.2011.07046.x
Tengberg LT, Cihoric M, Foss NB et al (2017) Complications after emergency laparotomy beyond the immediate postoperative period - a retrospective, observational cohort study of 1139 patients. Anaesthesia 72:309–316. https://doi.org/10.1111/anae.13721
Tolstrup M-B, Watt SK, Gögenur I (2017) Reduced Rate of Dehiscence After Implementation of a Standardized Fascial Closure Technique in Patients Undergoing Emergency Laparotomy. Ann Surg 265:821–826. https://doi.org/10.1097/SLA.0000000000001762
Jensen TK, Gögenur I, Tolstrup M-B (2020) Standardized Surgical Primary Repair for Burst Abdomen Reduces the Risk of Fascial Redehiscence. Ann Surg. https://doi.org/10.1097/SLA.0000000000003766
Marwah S, Marwah N, Singh M et al (2005) Addition of rectus sheath relaxation incisions to emergency midline laparotomy for peritonitis to prevent fascial dehiscence. World J Surg 29:235–239. https://doi.org/10.1007/s00268-004-7538-6
Kim JJ, Liang MK, Subramanian A et al (2011) Predictors of relaparotomy after nontrauma emergency general surgery with initial fascial closure. Am J Surg 202:549–552. https://doi.org/10.1016/j.amjsurg.2011.06.023
Webster C, Neumayer L, Smout R et al (2003) Prognostic models of abdominal wound dehiscence after laparotomy. J Surg Res 109:130–137. https://doi.org/10.1016/s0022-4804(02)00097-5
Bloemen A, van Dooren P, Huizinga BF, Hoofwijk AGM (2011) Randomized clinical trial comparing polypropylene or polydioxanone for midline abdominal wall closure. Br J Surg 98:633–639. https://doi.org/10.1002/bjs.7398
Kenig J, Richter P, Lasek A et al (2014) The efficacy of risk scores for predicting abdominal wound dehiscence: a case-controlled validation study. BMC Surg 14:65. https://doi.org/10.1186/1471-2482-14-65
Jensen KK, Oma E, van Ramshorst GH et al (2022) Abdominal wound dehiscence is dangerous: a nationwide study of 14,169 patients undergoing elective open resection for colonic cancer. Hernia J Hernias Abdom Wall Surg 26:75–86. https://doi.org/10.1007/s10029-020-02350-z
Riou JP, Cohen JR, Johnson H (1992) Factors influencing wound dehiscence. Am J Surg 163:324–330. https://doi.org/10.1016/0002-9610(92)90014-i
Carlson MA (1997) Acute wound failure. Surg Clin North Am 77:607–636. https://doi.org/10.1016/s0039-6109(05)70571-5
Kenig J, Richter P, Żurawska S et al (2012) Risk factors for wound dehiscence after laparotomy - clinical control trial. Pol Przegl Chir 84:565–573. https://doi.org/10.2478/v10035-012-0094-0
van Ramshorst GH, Eker HH, van der Voet JA et al (2013) Long-term outcome study in patients with abdominal wound dehiscence: a comparative study on quality of life, body image, and incisional hernia. J Gastrointest Surg Off J Soc Surg Aliment Tract 17:1477–1484. https://doi.org/10.1007/s11605-013-2233-2
van Ramshorst GH, Nieuwenhuizen J, Hop WCJ et al (2010) Abdominal wound dehiscence in adults: development and validation of a risk model. World J Surg 34:20–27. https://doi.org/10.1007/s00268-009-0277-y
Walming S, Angenete E, Block M et al (2017) Retrospective review of risk factors for surgical wound dehiscence and incisional hernia. BMC Surg 17:19. https://doi.org/10.1186/s12893-017-0207-0
Yilmaz KB, Akıncı M, Doğan L et al (2013) A prospective evaluation of the risk factors for development of wound dehiscence and incisional hernia. Ulus Cerrahi Derg 29:25–30. https://doi.org/10.5152/UCD.2013.06
Albertsmeier M, Hofmann A, Baumann P et al (2021) Effects of the short-stitch technique for midline abdominal closure: short-term results from the randomised-controlled ESTOIH trial. Hernia J Hernias Abdom Wall Surg. https://doi.org/10.1007/s10029-021-02410-y
Smart P, Mann GB (2003) Meta-analysis of techniques for closure of midline abdominal incisions (Br J Surg 2002; 89: 1350–1356). Br J Surg 90:370. https://doi.org/10.1002/bjs.4159
Peponis T, Bohnen JD, Muse S et al (2018) Interrupted versus continuous fascial closure in patients undergoing emergent laparotomy: A randomized controlled trial. J Trauma Acute Care Surg 85:459–465. https://doi.org/10.1097/TA.0000000000001970
Diener MK, Voss S, Jensen K et al (2010) Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg 251:843–856. https://doi.org/10.1097/SLA.0b013e3181d973e4
Deerenberg EB, Harlaar JJ, Steyerberg EW et al (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet Lond Engl 386:1254–1260. https://doi.org/10.1016/S0140-6736(15)60459-7
Kvist M, Henriksen NA, Burcharth J et al (2023) Rectus diastasis increases risk of burst abdomen in emergency midline laparotomies: a matched case-control study. Hernia J Hernias Abdom Wall Surg 27:353–361. https://doi.org/10.1007/s10029-022-02719-2
Kokotovic D, Jensen TK (2023) Acute abdominal pain and emergency laparotomy: bundles of care to improve patient outcomes. Br J Surg 110:1594–1596. https://doi.org/10.1093/bjs/znad224
Kokotovic D, Burcharth J (2023) Enhanced recovery after emergency laparotomy. Br J Surg 110:538–540. https://doi.org/10.1093/bjs/znad056
Tolstrup M-B, Jensen TK, Gögenur I (2023) Intraoperative Surgical Strategy in Abdominal Emergency Surgery. World J Surg 47:162–170. https://doi.org/10.1007/s00268-022-06782-9
Cuschieri S (2019) The STROBE guidelines Saudi J Anaesth 13:S31–S34. https://doi.org/10.4103/sja.SJA_543_18
Muysoms FE, Antoniou SA, Bury K et al (2015) European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia J Hernias Abdom Wall Surg 19:1–24. https://doi.org/10.1007/s10029-014-1342-5
Park C-M, Koh Y, Jeon K et al (2014) Impact of Eastern Cooperative Oncology Group Performance Status on hospital mortality in critically ill patients. J Crit Care 29:409–413. https://doi.org/10.1016/j.jcrc.2014.01.016
Slankamenac K, Graf R, Barkun J et al (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7. https://doi.org/10.1097/SLA.0b013e318296c732
Harris PA, Taylor R, Minor BL et al (2019) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Gislason H, Grønbech JE, Søreide O (1995) Burst abdomen and incisional hernia after major gastrointestinal operations–comparison of three closure techniques. Eur J Surg Acta Chir 161:349–354
Madsen G, Fischer L, Wara P (1992) Burst abdomen–clinical features and factors influencing mortality. Dan Med Bull 39:183–185
Jensen TK, Nielsen YW, Gögenur I, Tolstrup M-B (2022) Sarcopenia is associated with increased risk of burst abdomen after emergency midline laparotomy: a matched case-control study. Eur J Trauma Emerg Surg Off Publ Eur Trauma Soc 48:4189–4196. https://doi.org/10.1007/s00068-022-01958-3
Kvist M, Burcharth J, Nielsen YW, Jensen TK (2022) Abdominal subcutaneous obesity and the risk of burst abdomen: a matched case-control study. Langenbecks Arch Surg 407:3719–3726. https://doi.org/10.1007/s00423-022-02682-7
Lima HVG, Rasslan R, Novo FCF et al (2020) Prevention of Fascial Dehiscence with Onlay Prophylactic Mesh in Emergency Laparotomy: A Randomized Clinical Trial. J Am Coll Surg 230:76–87. https://doi.org/10.1016/j.jamcollsurg.2019.09.010
Ulutas ME, Sahin A, Simsek G et al (2023) Does onlay mesh placement in emergency laparotomy prevent incisional hernia? A prospective randomized double-blind study. Hernia J Hernias Abdom Wall Surg 27:883–893. https://doi.org/10.1007/s10029-023-02770-7
Marcolin P, Poli M, de Figueiredo S, Oliveira Trindade B et al (2024) Prophylactic mesh augmentation in emergency laparotomy closure: a meta-analysis of randomized controlled trials with trial sequential analysis. Hernia J Hernias Abdom Wall Surg. https://doi.org/10.1007/s10029-023-02943-4
Jairam AP, López-Cano M, Garcia-Alamino JM et al (2020) Prevention of incisional hernia after midline laparotomy with prophylactic mesh reinforcement: a meta-analysis and trial sequential analysis. BJS Open 4:357–368. https://doi.org/10.1002/bjs5.50261
Pizza F, D’Antonio D, Ronchi A et al (2021) Prophylactic sublay non-absorbable mesh positioning following midline laparotomy in a clean-contaminated field: randomized clinical trial (PROMETHEUS). Br J Surg 108:638–643. https://doi.org/10.1093/bjs/znab068
Valverde S, Arbós MA, Quiles MT et al (2021) Use of a bioabsorbable mesh in midline laparotomy closure to prevent incisional hernia: randomized controlled trial. Hernia J Hernias Abdom Wall Surg. https://doi.org/10.1007/s10029-021-02435-3
Frassini S, Calabretto F, Granieri S, et al (2023) Prophylactic mesh augmentation after laparotomy for elective and emergency surgery: meta-analysis. BJS Open 7:zrad060. https://doi.org/10.1093/bjsopen/zrad060
Bravo-Salva A, Argudo-Aguirre N, González-Castillo AM et al (2021) Long-term follow-up of prophylactic mesh reinforcement after emergency laparotomy. A retrospective controlled study BMC Surg 21:243. https://doi.org/10.1186/s12893-021-01243-x
Frassini S, Cobianchi L, Fugazzola P et al (2023) ECLAPTE: Effective Closure of LAParoTomy in Emergency-2023 World Society of Emergency Surgery guidelines for the closure of laparotomy in emergency settings. World J Emerg Surg WJES 18:42. https://doi.org/10.1186/s13017-023-00511-w
Goodenough CJ, Ko TC, Kao LS et al (2015) Development and validation of a risk stratification score for ventral incisional hernia after abdominal surgery: hernia expectation rates in intra-abdominal surgery (the HERNIA Project). J Am Coll Surg 220:405–413. https://doi.org/10.1016/j.jamcollsurg.2014.12.027
Fischer JP, Basta MN, Mirzabeigi MN et al (2016) A Risk Model and Cost Analysis of Incisional Hernia After Elective, Abdominal Surgery Based Upon 12,373 Cases: The Case for Targeted Prophylactic Intervention. Ann Surg 263:1010–1017. https://doi.org/10.1097/SLA.0000000000001394
Cherla DV, Moses ML, Mueck KM et al (2017) External Validation of the HERNIAscore: An Observational Study. J Am Coll Surg 225:428–434. https://doi.org/10.1016/j.jamcollsurg.2017.05.010
Funding
Open access funding provided by Copenhagen University.
Author information
Authors and Affiliations
Contributions
Madeline Kvist and Jakob Burcharth contributed to the study conception and design. Material preparation, data collection and analysis were performed by Madeline Kvist, Thomas Korgaard Jensen and Christian Snitkjær. The first draft of the manuscript was written by Madeline Kvist. All authors commented on previous versions of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Ethical aprroval
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. This research project was approved by the Danish Data Protection Agency (P-2021-431) and the Capital Region of Demark (P-2020-1166, R-21038079). The project did not qualify for ethics approval by Danish law.
Human and animal rights
No animals were used for this study.
Informed consent
Informed consent was not required due to the retrospective and observational nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper is not based on previous communication to a society or meeting.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kvist, M., Jensen, T.K., Snitkjær, C. et al. The clinical consequences of burst abdomen after emergency midline laparotomy: a prospective, observational cohort study. Hernia (2024). https://doi.org/10.1007/s10029-024-03104-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10029-024-03104-x