Abstract
Purpose
The causes of burst abdomen after midline laparotomy remain uncertain. Obesity is a suspected risk factor. The purpose of this study was to investigate the association between abdominal subcutaneous obesity (ASO) and burst abdomen in patients undergoing emergency midline laparotomy.
Methods
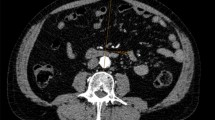
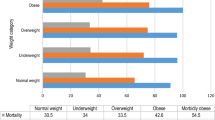
We conducted a single-centre, retrospective, matched case–control study of patients undergoing emergency midline laparotomy from May 2016 to August 2021. Patients suffering from burst abdomen were matched 1:4 with controls based on age and sex. Abdominal wall closure was standardized in the study period with the small bites, small stitches technique. ASO was defined as the highest sex-specific quartile (≥ 75%) of subcutaneous fat layer evaluated on CT. The primary outcome was the association between ASO and burst abdomen, stratified between cases and controls. Secondary outcomes included 30- and 90-day mortality, length of stay, and suspected risk factors of burst abdomen, assessed by multivariate analysis across cases and controls.
Results
A total of 475 patients were included in this study, with 95 cases matched to 380 controls. Liver cirrhosis, active smoking, and high alcohol consumption were more common among cases in an unadjusted analysis. Liver cirrhosis (odds ratio (OR) 3.32, p = 0.045) and active smoking (OR 1.98, p = 0.009) remained significant in a multivariate analysis and were associated with burst abdomen. One hundred twenty-four patients had ASO. ASO was not significantly associated with burst abdomen (OR 1.11, p = 0.731).
Conclusion
ASO was not found to be associated with an increased risk of burst abdomen after emergency midline laparotomy.


Similar content being viewed by others
References
Webster C, Neumayer L, Smout R et al (2003) Prognostic models of abdominal wound dehiscence after laparotomy. J Surg Res 109:130–137. https://doi.org/10.1016/s0022-4804(02)00097-5
Bloemen A, van Dooren P, Huizinga BF, Hoofwijk AGM (2011) Randomized clinical trial comparing polypropylene or polydioxanone for midline abdominal wall closure. Br J Surg 98:633–639. https://doi.org/10.1002/bjs.7398
Kenig J, Richter P, Lasek A et al (2014) The efficacy of risk scores for predicting abdominal wound dehiscence: a case-controlled validation study. BMC Surg 14:65. https://doi.org/10.1186/1471-2482-14-65
Marwah S, Marwah N, Singh M et al (2005) Addition of rectus sheath relaxation incisions to emergency midline laparotomy for peritonitis to prevent fascial dehiscence. World J Surg 29:235–239. https://doi.org/10.1007/s00268-004-7538-6
Kim JJ, Liang MK, Subramanian A et al (2011) Predictors of relaparotomy after nontrauma emergency general surgery with initial fascial closure. Am J Surg 202:549–552. https://doi.org/10.1016/j.amjsurg.2011.06.023
Tolstrup M-B, Watt SK, Gögenur I (2017) Reduced rate of dehiscence after implementation of a standardized fascial closure technique in patients undergoing emergency laparotomy. Ann Surg 265:821–826. https://doi.org/10.1097/SLA.0000000000001762
van Ramshorst GH, Eker HH, van der Voet JA et al (2013) Long-term outcome study in patients with abdominal wound dehiscence: a comparative study on quality of life, body image, and incisional hernia. J Gastrointest Surg Off J Soc Surg Aliment Tract 17:1477–1484. https://doi.org/10.1007/s11605-013-2233-2
Carlson MA (1997) Acute wound failure. Surg Clin North Am 77:607–636. https://doi.org/10.1016/s0039-6109(05)70571-5
Riou JP, Cohen JR, Johnson H (1992) Factors influencing wound dehiscence. Am J Surg 163:324–330. https://doi.org/10.1016/0002-9610(92)90014-i
Yılmaz KB, Akıncı M, Doğan L et al (2013) A prospective evaluation of the risk factors for development of wound dehiscence and incisional hernia. Ulus Cerrahi Derg 29:25–30. https://doi.org/10.5152/UCD.2013.06
Smart P, Mann GB (2003) Meta-analysis of techniques for closure of midline abdominal incisions (Br J Surg 2002; 89: 1350–1356). Br J Surg 90:370. https://doi.org/10.1002/bjs.4159
Seiler CM, Bruckner T, Diener MK et al (2009) Interrupted or continuous slowly absorbable sutures for closure of primary elective midline abdominal incisions: a multicenter randomized trial (INSECT: ISRCTN24023541). Ann Surg 249:576–582. https://doi.org/10.1097/SLA.0b013e31819ec6c8
Gislason H, Viste A (1999) Closure of burst abdomen after major gastrointestinal operations–comparison of different surgical techniques and later development of incisional hernia. Eur J Surg Acta Chir 165:958–961. https://doi.org/10.1080/110241599750008071
López-Cano M, García-Alamino JM, Antoniou SA et al (2018) EHS clinical guidelines on the management of the abdominal wall in the context of the open or burst abdomen. Hernia J Hernias Abdom Wall Surg 22:921–939. https://doi.org/10.1007/s10029-018-1818-9
Muysoms FE, Antoniou SA, Bury K et al (2015) European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia J Hernias Abdom Wall Surg 19:1–24. https://doi.org/10.1007/s10029-014-1342-5
Israelsson LA, Jonsson T (1993) Suture length to wound length ratio and healing of midline laparotomy incisions. Br J Surg 80:1284–1286. https://doi.org/10.1002/bjs.1800801020
Israelsson LA, Jonsson T (1997) Overweight and healing of midline incisions: the importance of suture technique. Eur J Surg Acta Chir 163:175–180
Jensen TK, Gögenur I, Tolstrup M-B (2020) Standardized surgical primary repair for burst abdomen reduces the risk of fascial redehiscence. Ann Surg. https://doi.org/10.1097/SLA.0000000000003766
van Ramshorst GH, Nieuwenhuizen J, Hop WCJ et al (2010) Abdominal wound dehiscence in adults: development and validation of a risk model. World J Surg 34:20–27. https://doi.org/10.1007/s00268-009-0277-y
Walming S, Angenete E, Block M et al (2017) Retrospective review of risk factors for surgical wound dehiscence and incisional hernia. BMC Surg 17:19. https://doi.org/10.1186/s12893-017-0207-0
Söderbäck H, Gunnarsson U, Martling A et al (2019) Incidence of wound dehiscence after colorectal cancer surgery: results from a national population-based register for colorectal cancer. Int J Colorectal Dis 34:1757–1762. https://doi.org/10.1007/s00384-019-03390-3
Nattenmüller J, Böhm J, Bagdassarjan A et al (2019) CT-quantified adipose tissue distribution: risk or protective factor for complications after rectal cancer surgery? Obes Facts 12:259–271. https://doi.org/10.1159/000499320
Amri R, Bordeianou LG, Sylla P, Berger DL (2014) Obesity, outcomes and quality of care: body mass index increases the risk of wound-related complications in colon cancer surgery. Am J Surg 207:17–23. https://doi.org/10.1016/j.amjsurg.2013.05.016
Peponis T, Bohnen JD, Muse S et al (2018) Interrupted versus continuous fascial closure in patients undergoing emergent laparotomy: a randomized controlled trial. J Trauma Acute Care Surg 85:459–465. https://doi.org/10.1097/TA.0000000000001970
Diener MK, Voss S, Jensen K et al (2010) Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg 251:843–856. https://doi.org/10.1097/SLA.0b013e3181d973e4
Deerenberg EB, Harlaar JJ, Steyerberg EW et al (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet Lond Engl 386:1254–1260. https://doi.org/10.1016/S0140-6736(15)60459-7
Israelsson LA, Jonsson T (1994) Physical properties of self locking and conventional surgical knots. Eur J Surg Acta Chir 160:323–327
Albertsmeier M, Hofmann A, Baumann P et al (2022) Effects of the short-stitch technique for midline abdominal closure: short-term results from the randomised-controlled ESTOIH trial. Hernia 26(1):87–95. https://doi.org/10.1007/s10029-021-02410-y.
Chang Y-WW, Murphy K, Yackzan D et al (2021) Abdominal wall thickness is a predictor for surgical site infections in patients undergoing colorectal operations. Am Surg 87:1155–1162. https://doi.org/10.1177/0003134820956932
O’Meara L, Ahmad SB, Glaser J et al (2015) Outcomes of primary fascial closure after open abdomen for nontrauma emergency general surgery patients. Am J Surg 210:1126–1130. https://doi.org/10.1016/j.amjsurg.2015.06.030 (discussion 1130-1131)
Thorup T, Tolstrup M-B, Gögenur I (2019) Reduced rate of incisional hernia after standardized fascial closure in emergency laparotomy. Hernia J Hernias Abdom Wall Surg 23:341–346. https://doi.org/10.1007/s10029-019-01893-0
Rothman KJ (2005) (2008) BMI-related errors in the measurement of obesity. Int J Obes 32(Suppl 3):S56–59. https://doi.org/10.1038/ijo.2008.87
Hasselager R, Gögenur I (2014) Core muscle size assessed by perioperative abdominal CT scan is related to mortality, postoperative complications, and hospitalization after major abdominal surgery: a systematic review. Langenbecks Arch Surg 399:287–295. https://doi.org/10.1007/s00423-014-1174-x
Israelsson LA (1996) The absorbable knot is smaller and stronger. An easy and safe method for continuous suture technique. Lakartidningen 93:2341–2342
Park C-M, Koh Y, Jeon K et al (2014) Impact of Eastern Cooperative Oncology Group Performance Status on hospital mortality in critically ill patients. J Crit Care 29:409–413. https://doi.org/10.1016/j.jcrc.2014.01.016
Todd B (2017) New CDC guideline for the prevention of surgical site infection. Am J Nurs 117:17. https://doi.org/10.1097/01.NAJ.0000521963.77728.c0
Guo S, DiPietro LA (2010) Factors affecting wound healing. J Dent Res 89:219–229. https://doi.org/10.1177/0022034509359125
Tengberg LT, Cihoric M, Foss NB et al (2017) Complications after emergency laparotomy beyond the immediate postoperative period - a retrospective, observational cohort study of 1139 patients. Anaesthesia 72:309–316. https://doi.org/10.1111/anae.13721
Madsen G, Fischer L, Wara P (1992) Burst abdomen–clinical features and factors influencing mortality. Dan Med Bull 39:183–185
Author information
Authors and Affiliations
Contributions
Madeline Kvist, Jakob Burcharth, and Thomas Korgaard Jensen contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Madeline Kvist, Yousef Wirenfeldt Nielsen, and Thomas Korgaard Jensen. The first draft of the manuscript was written by Madeline Kvist, and all authors commented on previous versions of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper is not based on previous communication to a society or meeting.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kvist, M., Burcharth, J., Nielsen, Y.W. et al. Abdominal subcutaneous obesity and the risk of burst abdomen: a matched case–control study. Langenbecks Arch Surg 407, 3719–3726 (2022). https://doi.org/10.1007/s00423-022-02682-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02682-7