Abstract
Purpose
The open posterior approach in the form of either a Stoppa or Wantz operation may be a good alternative technique particularly in the repair of complex inguinal hernias. The term “complex inguinal hernia” designates hernias with a combination of arduous features including large hernia defects, large to giant hernia sacs, multiple recurrences, and bilaterality. In this retrospective analysis, we investigated our results of open posterior repair in view of its feasibility in patients with complex inguinoscrotal hernias.
Methods
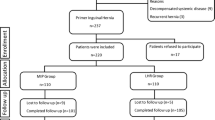
From a series of 845 inguinal hernia patients, we retrospectively reviewed the records of 60 patients with complex inguinal hernias whom were directed to open preperitoneal repair by either a Stoppa or Wantz procedure.
Results
More than 80% of cases were males with large to giant inguinoscrotal hernias. One half of patients had bilateral hernias, and one fourth had recurrent hernias. Early postoperative complications occurred in almost half of patients; however, most of them were minor. The most important early complication in this series was the full recurrences we encountered in the very next morning in two patients. Eighty-three percent of patients left hospital in the first 2 days averaging 1.8 days of hospital stay. The mesh:defect area ratio is < 7 in recurrent hernias while it is > 9 in nonrecurrent cases.
Conclusion
The open posterior approach to complex inguinal hernias facilitated both handling and repair of difficult hernias. It was very well tolerated by the patients, and yielded favorable postoperative results. We think the open posterior repair may be a method of choice in the repair of complex inguinal hernias.
Similar content being viewed by others
Availability of data and material
Our data are available for reviewers.
Code availability
Not applicable.
References
Vasiliadis K, Knaebel HP, Djakovic N, Nyarangi-dix J, Schmidt J, Büchler M (2010) Challenging surgical management of a giant inguinoscrotal hernia: report of a case. Surg Today 40:684–687
Iskandar M, Ferzli G (2018) Complex inguinal hernias. In: Bittner R, Bittner R, Köckerling F, Fitzgibbons RJ, LeBlanc KA, Mittal SK, Chowbey P (eds) Laparo-endoscopic hernia surgery, 1st edn. Springer-Verlag GmbH, Berlin, pp 171–182
Beitler JC, Gomes SM, Coelho ACJ, Manso JEF (2009) Complex inguinal hernia repairs. Hernia 13:61–66. https://doi.org/10.1007/s10029-008-0432-7
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Hidalgo Pascual M et al (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11:113–116
Andresen K, Rosenberg J (2017) Open preperitoneal groin hernia repair with mesh: a qualitative systematic review. Am J Surg 213:1153–1159
Yang B, Jiang Z, Li Y, Zong Z, Chen S (2015) Long-term outcome for open preperitoneal mesh repair of recurrent inguinal hernia. Int J Surg 19:134–136
Campanelli G, Pettinari D, Nicolosi FM, Cavalli M, Avesani EC (2006) Inguinal hernia recurrence: classification and approach. Hernia 10:159–161. https://doi.org/10.1007/s10029-005-0053-3
Campanelli G, Pettinari D, Cavalli M, Avesani EC (2006) Inguinal hernia recurrence: classification and approach. J Minim Access Surg 2:147–150. https://doi.org/10.4103/0972-9941.27728
Kurzer M, Belsham PA, Kark AE (2002) Prospective study of open preperitoneal mesh repair for recurrent inguinal hernia. Br J Surg 89:90–93
Pennylouise H, Mili D, Naveen C (2018) Loss of domain leading to intra-operative cardiorespiratory arrest during open repair of a giant inguinoscrotal hernia and hydrocele. JPRAS Open 16:1–5
Staubitz JI, Gassmann P, Kauff DW, Lang H (2017) Surgical treatment strategies for giant inguinoscrotal hernia—a case report with review of the literature. BMC Surg 17:135
Lin R, Lu F, Lin X, Yang Y, Chen Y, Huang H (2020) Transinguinal preperitoneal repair of giant inguinoscrotal hernias using Kugel mesh. J Visc Surg 157:372–377. https://doi.org/10.1016/j.jviscsurg.2020.01.007 (Epub 2020 Jan 31)
Sanford Z, Weltz AS, Singh D, Hanley R, Todd D, Belyansky I (2019) Minimally invasive multidisciplinary approach to chronic giant inguinoscrotal hernias. Surg Innov 26:427–431
Cavalli M, Biondi A, Bruni PG, Campanelli G (2015) Giant inguinal hernia: the challenging hug technique. Hernia 19:775–783
Haskins IN, Rosen MJ (2017) Inguinal hernia recurrence in inguinal hernia surgery. In: Campanelli G (ed) The art of hernia, 1st edn. Springer-Verlag, Italy, pp 151–156
Beets GL, van Geldere D, Baeten CG, Go PM (1996) Long-term results of giant prosthetic reinforcement of the visceral sac for complex recurrent inguinal hernia. Br J Surg 83:203–206
Ertem M, Gok H, Ozben V, Hatipoglu E, Yildiz E (2018) Can volumetric measurement be used in the selection of treatment for inguinoscrotal hernias? Turk J Surg 34:13–16
Stoppa RE (1995) The preperitoneal approach and prosthetic repair of groin hernias. In: Nyhus LM, Condon RE (eds) Hernia, 4th edn. JB Lippincott Company, Philadelphia, pp 188–206
Wantz GE (1995). In: Nyhus LM, Condon RE (eds) Special Comment: personal experience with the Stoppa technique, 4th edn. JB Lippincott Company, Philadelphia, pp 206–210
Malazgirt Z, Ozkan K, Dervisoglu A, Kaya E (2000) Comparison of Stoppa and Lichtenstein techniques in the repair of bilateral inguinal hernias. Hernia 4:264–267
Wolloscheck T, Konerding MA (2009) Dimensions of the myopectineal orifice: a human cadaver study. Hernia 13:639–642. https://doi.org/10.1007/s10029-009-0559-1
Tulloh B, de Beaux A (2016) Defects and donuts: the importance of the mesh:defect area ratio. Hernia 20:893–895. https://doi.org/10.1007/s10029-016-1524-4
Eisenberg D, Hwa K, Wren SM (2015) Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair instead of face-to-face clinic visit. JSLS 19:e2014.00205. https://doi.org/10.4293/JSLS.2014.00205
Trakarnsagna A, Chinswangwatanakul V, Methasate A, Swangsri J, Phalanusitthepha C, Parakonthun T, Taweerutchana V, Akaraviputh T (2014) Giant inguinal hernia: report of a case and reviews of surgical techniques. Int J Surg Case Rep 5:868–872
Sahsamanis G, Samaras S, Basios A, Katis K, Dimitrakopoulos G (2016) Treatment of a half century year old giant inguinoscrotal hernia. A case report. Int J Surg Case Rep 25:51–54
Muysoms FE et al (2009) (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414. https://doi.org/10.1007/s10029-009-0518-x
LeBlanc K (2016) Proper mesh overlap is a key determinant in hernia recurrence following laparoscopic ventral and incisional hernia repair. Hernia 20:85–99. https://doi.org/10.1007/s10029-015-1399-9
Hauters P, Desmet J, Gherardi D, Dewaele S, Poilvache H, Malvaux P (2017) Assessment of predictive factors for recurrence in laparoscopic ventral hernia repair using a bridging technique. Surg Endosc 31:3656–3663. https://doi.org/10.1007/s00464-016-5401-0
Kallinowski F, Harder F, Gutjahr D, Raschidi R, Silva TG, Vollmer M, Nessel R (2017) Assessing the GRIP of ventral hernia repair: how to securely fasten dis classified meshes. Front Surg 2017(4):78. https://doi.org/10.3389/fsurg.2017.00078
Hollinsky C, Sandberg S, Koch T, Seidler S (2008) Biomechanical properties of lightweight versus heavyweight meshes for laparoscopic inguinal hernia repair and their impact on recurrence rates. Surg Endosc 22:2679–2685. https://doi.org/10.1007/s00464-008-9936-6
Wu F, Zhang X, Liu Y, Cao D, Yu Y, Ma Y (2020) Lightweight mesh versus heavyweight mesh for laparo-endoscopic inguinal hernia repair: a systematic review and meta-analysis. Hernia 24:31–39
Bakker WJ, Aufenacker TJ, Boschman JS, Burgmans JPJ (2021) Heavyweight mesh is superior to lightweight mesh in laparo-endoscopic inguinal hernia repair: a meta-analysis and trial sequential analysis of randomized controlled trials. Ann Surg 273:890–899
Mehendale FV, Taams KO, Kingsnorth AN (2000) Repair of a giant inguinoscrotal hernia. Br J Surg 53:525–529
Mayagoitia JC, Suarez D, Arenas JC, Diaz de Leon V (2006) Preoperative progressive pneumoperitoneum in patients with abdominal wall hernias. Hernia 10:213–217
Piskin T, Aydin C, Barut B, DiricanA KC (2010) Preoperative progressive pneumoperitoneum for giant inguinal hernias. Ann Saudi Med 30:317–320
Patsas A, Tsiaousis P, Papaziogas B, Koutelidakis I, Goula J, Atmatzidis K (2010) Repair of a giant inguinoscrotal hernia. Hernia 14:305–307
Tang FX, Zong Z, Xu JB, Ma N, Zhou TC, Chen S (2020) Combination of preoperative progressive pneumoperitoneum and botulinum toxin A enables the laparoscopic transabdominal preperitoneal approach for repairing giant inguinoscrotal hernias. J Laparoendosc Adv Surg Tech A 30:260–266
Valliattu AJ, Kingsnorth AN (2008) Single-stage repair of giant inguinoscrotal hernias using the abdominal wall component separation technique. Hernia 12:329–330
Hamad A, Marimuthu K, Mothe B, Hanafy M (2013) Repair of massive inguinal hernia with loss of abdominal domain using laparoscopic component separation technique. J Surg Case Rep 3:rjt008. https://doi.org/10.1016/j.ijscr.2016.05.039.
Oprea V, Mardale S, Buia F et al (2021) The influence of transversus abdominis muscle release (TAR) for complex incisional hernia repair on the intraabdominal pressure and pulmonary function. Hernia 25:1601–1609. https://doi.org/10.1007/s10029-021-02395-8
Miller DB, Reed L (2020) Successful outcome of a giant inguinoscrotal hernia: a novel two-staged repair using preoperative progressive pneumoperitoneum and transversus abdominis release. J Surg Case Rep 2020:12. https://doi.org/10.1093/jscr/rjaa511
Belyansky I, Zahiri HR, Sanford Z, Weltz AS, Park A (2018) Early operative outcomes of endoscopic (eTEP access) robotic-assisted retromuscular abdominal wall hernia repair. Hernia 22:837–847. https://doi.org/10.1007/s10029-018-1795-z
Kudsi OY, Gokcal F (2021) Lateral approach totally extraperitoneal (TEP) robotic retromuscular ventral hernia repair. Hernia 25:211–222. https://doi.org/10.1007/s10029-019-02082-9
Ferzli GS, Khoury GE (2006) Treating recurrence after a totally extraperitoneal approach. Hernia 10:341–346
Ertem M, Ozben V, Gok H, Ozveri E (2013) Relaparoscopic treatment of recurrences after previous laparoscopic inguinal hernia repair. Minim Invasive Surg 2013:260131
Bisgaard T, Bay-Nielsen M, Kehlet H (2008) Re-recurrence after operation for recurrent inguinal hernia. A nationwide 8-year study on the role of the type of repair. Ann Surg 247:707–711
Thapar V, Rao P, Prabhu R, Desai C, Singh AS, Supe AN (2000) Giant prosthesis for reinforcement of visceral sac for complex bilateral and recurrent inguinal hernias: a prospective evaluation. J Postgrad Med 46:80–82
Funding
No specific funding was acquired for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed extensively to the work presented in this paper. Their roles are given below. Design of the work: ZM and KY. Acquisition of data: KY, MFG, AA and HO. Interpretation of data: ZM, KY, and IK. Drafting/critical revision: ZM, KY, and IK. Final approval: ZM.
Corresponding author
Ethics declarations
Conflict of interest
All of the authors declare that they have no conflict of interest.
Ethics approval
This retrospective study was approved by the Council on Ethics in Human Research of Istinye University, Istanbul Turkey (June 29, 2021 21-64), and have therefore been performed in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
The informed consent of hernia patients have been taken during hospitalization prior to their inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Malazgirt, Z., Yildirim, K., Karabicak, I. et al. Retrospective analysis of open preperitoneal mesh repair of complex inguinal hernias. Hernia 26, 1121–1130 (2022). https://doi.org/10.1007/s10029-022-02595-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-022-02595-w