Abstract
Purpose
Females suffer higher rates of operative recurrence and chronic pain following groin hernia repair. Guidelines recommend minimally invasive (MIS) groin hernia repair as the preferred approach to reduce these adverse outcomes. It is unknown what proportion of females receive MIS hernia repair. Therefore, our goal was to investigate adoption of evidence-based practices in groin hernia repair using sex as a biological variable.
Methods
Retrospective cohort study of adults undergoing elective groin hernia repair (2014–2019) within a statewide quality improvement collaborative. Primary outcome was surgical approach. Multivariable logistic regression was performed to analyze the likelihood of undergoing MIS hernia repair. Secondary outcomes were 30-day adjusted rates of clinical and patient-reported outcomes (PROs). PROs included regret to undergo surgery among patients who completed post-operative surveys.
Results
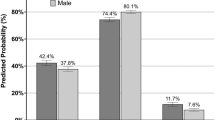
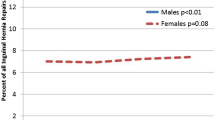
Among 23,723 patients, the majority (90.7%) were males. Compared to males, females less often underwent an MIS surgical approach (37.4% vs 45.1%, p < 0.0001). After adjustment for patient and clinical variables, females remained significantly less likely to undergo MIS groin hernia repair (aOR 0.88, 95% CI 0.80–0.97). Adjusted clinical outcomes were not different between males and females. Among 4325 patients who completed post-operative surveys, adjusted rates of regret to undergo surgery were higher among females (12.9% vs 8.5%, p = 0.003).
Conclusions
Even after adjusting for differences, females were less likely to receive guideline-concordant groin hernia repair and were more likely to regret surgery. Understanding the behaviors of surgeons who treat females with groin hernia may inform quality metrics to promote best practices in this population.
Similar content being viewed by others
References
Howard R, Telem D (2019) gender matters: mandating sex as a biologic variable in hernia research. Ann Surg 270:10–11
Geller SE, Adams MG, Carnes M (2006) Adherence to federal guidelines for reporting of sex and race/ethnicity in clinical trials. J Womens Health (Larchmt) 15:1123–1131
Rutkow IM (1998) Epidemiologic, economic, and sociologic aspects of hernia surgery in the United States in the 1990s. Surg Clin North Am 78(941–951):v–vi
Kockerling F et al (2019) Influencing factors on the outcome in female groin hernia repair: a registry-based multivariable analysis of 15,601 patients. Ann Surg 270:1–9
Wellwood J et al (1998) Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. BMJ 317:103–110
Neumayer L et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Fitzgibbons RJ Jr et al (2006) Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA 295:285–292
de Goede B et al (2018) Watchful waiting versus surgery of mildly symptomatic or asymptomatic inguinal hernia in men aged 50 years and older: a randomized controlled trial. Ann Surg 267:42–49
O’Dwyer PJ et al (2006) Observation or operation for patients with an asymptomatic inguinal hernia: a randomized clinical trial. Ann Surg 244:167–173
Siddaiah-Subramanya M, Ashrafi D, Memon B, Memon MA (2018) Causes of recurrence in laparoscopic inguinal hernia repair. Hernia 22:975–986
Burcharth J, Pommergaard HC, Bisgaard T, Rosenberg J (2015) Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov 22:303–317
Bullen NL, Massey LH, Antoniou SA, Smart NJ, Fortelny RH (2019) Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia 23:461–472
HerniaSurge G (2018) International guidelines for groin hernia management. Hernia 22:1–165
Burcharth J, Andresen K, Pommergaard HC, Bisgaard T, Rosenberg J (2014) Direct inguinal hernias and anterior surgical approach are risk factors for female inguinal hernia recurrences. Langenbecks Arch Surg 399:71–76
Vu JV et al (2019) Mechanisms of age and race differences in receiving minimally invasive inguinal hernia repair. Surg Endosc 33:4032–4037
Vu JV et al (2019) Surgeon utilization of minimally invasive techniques for inguinal hernia repair: a population-based study. Surg Endosc 33:486–493
Share DA et al (2011) How a regional collaborative of hospitals and physicians in Michigan cut costs and improved the quality of care. Health Aff (Millwood) 30:636–645
Birkmeyer NJ et al (2005) Partnering with payers to improve surgical quality: the Michigan plan. Surgery 138:815–820
Campbell DA Jr, Kubus JJ, Henke PK, Hutton M, Englesbe MJ (2009) The Michigan surgical quality collaborative: a legacy of Shukri Khuri. Am J Surg 198:S49-55
Englesbe MJ, Dimick JB, Sonnenday CJ, Share DA, Campbell DA Jr (2007) The Michigan surgical quality collaborative: will a statewide quality improvement initiative pay for itself? Ann Surg 246:1100–1103
Campbell DA Jr et al (2008) Surgical site infection prevention: the importance of operative duration and blood transfusion–results of the first American College of Surgeons-National Surgical Quality Improvement Program Best Practices Initiative. J Am Coll Surg 207:810–820
Brehaut JC et al (2003) Validation of a decision regret scale. Med Decis Making 23:281–292
Trout A, Magnusson AR, Hedges JR (2000) Patient satisfaction investigations and the emergency department: what does the literature say? Acad Emerg Med 7:695–709
Aspinal F, Addington-Hall J, Hughes R, Higginson IJ (2003) Using satisfaction to measure the quality of palliative care: a review of the literature. J Adv Nurs 42:324–339
Berkowitz R et al (2021) The impact of complications and pain on patient satisfaction. Ann Surg 273:1127–1134
Howard R et al (2019) Costs associated with modifiable risk factors in ventral and incisional hernia repair. JAMA Netw Open 2:E1916330
Henriksen NA et al (2020) Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Americas Hernia Society. Br J Surg 107:171–190
Kubasiak JC et al (2017) The effect of tobacco use on outcomes of laparoscopic and open ventral hernia repairs: a review of the NSQIP dataset. Surg Endosc 31:2661–2666
Ehlers AP, Vitous CA, Sales A, Telem DA (2020) Exploration of factors associated with surgeon deviation from practice guidelines for management of inguinal hernias. JAMA Netw Open 3:e2023684
Vitous CA et al (2020) Exploration of surgeon motivations in management of abdominal wall hernias: a qualitative study. JAMA Netw Open 3:e2015916
Jafri SM et al (2020) Surgeon attitudes and beliefs toward abdominal wall hernia repair in female patients of childbearing age. JAMA Surg 155:528–530
Howard R et al (2019) Optimizing postoperative opioid prescribing through quality-based reimbursement. JAMA Netw Open 2:e1911619
Howard R et al (2021) Development and implementation of preoperative optimization for high-risk patients with abdominal wall hernia. JAMA Netw Open 4:e216836
Fortunato L et al (2020) Regret and quality of life after mastectomy with or without reconstruction. Clin Breast Cancer 21(3):162
Strong, E et al. (2021) Patient decision-making and regret in pilonidal sinus surgery: a mixed-methods study. Colorectal Dis
Cohan JN et al (2021) Factors associated with decision regret among patients with diverticulitis in the elective setting. J Surg Res 261:159–166
Acknowledgements
APE, JRT, GHD, and JFW have no disclosures. RH receives unrelated funding from the Blue Cross Blue Shield of Michigan Foundation and the National Institute of Diabetes and Digestive and Kidney Diseases (5T32DK108740-05). JD receives grant funding from the NIH, AHRQ, Blue Cross Blue Shield of Michigan Foundation, and is a cofounder of ArborMetrix, Inc. DT receives funding from AHRQ K08HS025778-01A1 and receives consulting fees from Medtronic. The content of this study is solely the responsibility of the authors. No funder or sponsor had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. APE had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standards
All procedures performed in this study were in accordance with the ethical standards of the instiutinoa and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ehlers, A.P., Thumma, J.R., Howard, R. et al. Guideline-discordant care among females undergoing groin hernia repair: the importance of sex as a biologic variable. Hernia 26, 823–829 (2022). https://doi.org/10.1007/s10029-021-02543-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02543-0