Abstract
Purpose
The objective of the study was to correlate different orthognathic surgical procedures with operating time and blood loss, reported from an accredited resident training institution.
Methods
Ninety-five patient records were evaluated retrospectively. Individual blood volume, percent blood volume lost (BVL), and estimated blood loss (EBL) for each patient were recorded and correlated with operating time (OT). Statistics included independent t tests, one-way analysis of variance, and linear regression.
Results
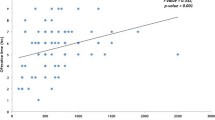
The mean OT for all procedures was 203 min with mean blood loss 556 ml. Mean EBL for males was 676 ml versus 468 ml for females. Overall BVL was 12.4 %, while for males, BVL was 13.3 % compared to 11.8 % for females. For a single orthognathic procedure (n = 45), mean OT 145 min., EBL 414 ml, and BVL 9.0 %; two procedures (n = 41), mean OT was 239 min., EBL 659 ml, and BVL 15 %; three procedures (n = 9), mean OT 328 min, EBL 793 ml, and BVL was 17 %.
Conclusion
Examination of individual procedures suggests a shorter OT for Le Fort I procedures with slightly greater EBL. Concomitant orthognathic procedures are associated with greater OT and EBL. Blood volume should be calculated for male and female patients separately. Percent BVL can be predicted based on OT using a basic equation.
Similar content being viewed by others
References
DuBois D, DuBois EF (1916) A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med 17:863–871
Medal.org Limited, Medical algorithms. http://www.medal.org. Accessed 6 September 2010
Kim SG, Park SS (2007) Incidence of complications and problems related to orthognathic surgery. J Oral Maxillofac Surg 65(12):2438–2444
Panula K, Finne K, Oikarinen K (2001) Incidence of complications and problems related to orthognathic surgery: a review of 655 patients. J Oral Maxillofac Surg 59(10):1128–1136
Kretschmer W, Köster U, Dietz K, Zoder W, Wangerin K (2008) Factors for intraoperative blood loss in bimaxillary osteotomies. J Oral Maxillofac Surg 66(7):1399–1403
Moenning JE, Bussard DA, Lapp TH, Garrison BT (1995) Average blood loss and the risk of requiring perioperative blood transfusion in 506 orthognathic surgical procedures. J Oral Maxillofac Surg 53(8):880–883
Rummasak D, Apipan B, Kaewpradup P (2011) Factors that determine intraoperative blood loss in bimaxillary osteotomies and the need for preoperative blood preparation. J Oral Maxillofac Surg 69(11):e456–e460
Yu CN, Chow TK, Kwan AS, Wong SL, Fung SC (2000) Intra-operative blood loss and operating time in orthognathic surgery using induced hypotensive general anaesthesia: prospective study. Hong Kong Med J 6(3):307–311
Praveen K, Narayanan V, Muthusekhar MR, Baig MF (2001) Hypotensive anaesthesia and blood loss in orthognathic surgery: a clinical study. Br J Oral Maxillofac Surg 39(2):138–140
Schaberg SJ, Kelly JF, Terry BC, Posner MA, Anderson EF (1976) Blood loss and hypotensive anesthesia in oral-facial corrective surgery. J Oral Surg 34(2):147–156
Zellin G, Rasmusson L, Pålsson J, Kahnberg KE (2004) Evaluation of hemorrhage depressors on blood loss during orthognathic surgery: a retrospective study. J Oral Maxillofac Surg 62(6):662–666
Choi WS, Irwin MG, Samman N (2009) The effect of tranexamic acid on blood loss during orthognathic surgery: a randomized controlled trial. J Oral Maxillofac Surg 67(1):125–133
Song G, Yang P, Hu J, Zhu S, Li Y, Wang Q (2013) The effect of tranexamic acid on blood loss in orthognathic surgery: a meta-analysis of randomized controlled trials. Oral Surg Oral Med Oral Pathol Oral Radiol 115(5):595–600
Hiippala ST, Strid LJ, Wennerstrand MI, Arvela JV, Niemelä HM, Mäntylä SK, Kuisma RP, Ylinen JE (1997) Tranexamic acid radically decreases blood loss and transfusions associated with total knee arthroplasty. Anesth Analg 84(4):839–844
Casati V, Guzzon D, Oppizzi M, Bellotti F, Franco A, Gerli C, Cossolini M, Torri G, Calori G, Benussi S, Alfieri O (2000) Tranexamic acid compared with high-dose aprotinin in primary elective heart operations: effects on perioperative bleeding and allogeneic transfusions. J Thorac Cardiovasc Surg 120(3):520–527
Jamieson WR, Dryden PJ, O’Connor JP, Sadeghi H, Ansley DM, Merrick PM (1997) Beneficial effect of both tranexamic acid and aprotinin on blood loss reduction in reoperative valve replacement surgery. Circulation 96(9 Suppl):II-96-100
Wells PS (2002) Safety and efficacy of methods for reducing perioperative allogeneic transfusion: a critical review of the literature. Am J Ther 9(5):377–388, Review
de Lange J, Baas EM, Horsthuis RB, Booij A (2008) The effect of nasal application of cocaine/adrenaline on blood loss in Le Fort I osteotomies. Int J Oral Maxillofac Surg 37(1):21–24
Kretschmer WB, Baciut G, Bacuit M, Zoder W, Wangerin K (2010) Intraoperative blood loss in bimaxillary orthognathic surgery with multisegmental Le Fort I osteotomies and additional procedures. Br J Oral Maxillofac Surg 48(4):276–280
Dhariwal DK, Gibbons AJ, Kittur MA, Sugar AW (2004) Blood transfusion requirements in bimaxillary osteotomies. Br J Oral Maxillofac Surg 42(3):231–235
Ueki K, Marukawa K, Shimada M, Nakagawa K, Yamamoto E (2005) The assessment of blood loss in orthognathic surgery for prognathia. J Oral Maxillofac Surg 63(3):350–354
Ash DC, Mercuri LG (1985) The relationship between blood ordered and blood administered in orthognathic surgery: a retrospective study. J Oral Maxillofac Surg 43(12):944–946
Samman N, Cheung LK, Tong AC, Tideman H (1996) Blood loss and transfusion requirements in orthognatic surgery. J Oral Maxillofac Surg 54(1):21–24
Gong SG, Krishnan V, Waack D (2002) Blood transfusions in bimaxillary orthognathic surgery: are they necessary? Int J Adult Orthodon Orthognath Surg 17(4):314–317
Messmer KF (1987) Acceptable hematocrit levels in surgical patients. World J Surg 11(1):41–46
Conflict of interest
Dr. Baur is a consultant for Novartis and Checkpoint Surgical LLC. Dr. Altay has provided consultancy for Checkpoint Surgical LLC in 2014. Other authors disclose no financial or personal relationships with other people or organizations. Initial findings of this study have been presented in the form of a poster at the annual meeting of the American Association of Oral and Maxillofacial Surgeons in 2008. There was no grant support for this study. All authors have viewed and agreed to the final form of the submission.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schneider, K.M., Altay, M.A., Demko, C. et al. Predictors of blood loss during orthognathic surgery: outcomes from a teaching institution. Oral Maxillofac Surg 19, 361–367 (2015). https://doi.org/10.1007/s10006-015-0503-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-015-0503-8