Abstract
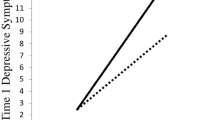
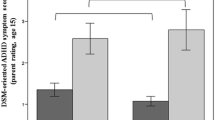
To investigate developmental changes in emotion dysregulation (ED) and associated symptoms of emotional lability, irritability, anxiety, and depression, among girls and boys with and without ADHD from childhood through adolescence. Data were collected from a sample of 8–18-year-old children with (n = 264; 76 girls) and without (n = 153; 56 girls) ADHD, with multiple time-points from a subsample of participants (n = 121). Parents and youth completed rating scales assessing child ED, emotional lability, irritability, anxiety, and depression. Mixed effects models were employed to examine effects and interactions of diagnosis, sex [biological sex assigned at birth], age among boys and girls with and without ADHD. Mixed effects analyses showed sexually dimorphic developmental patterns between boys and girls, such that boys with ADHD showed a greater reduction in ED, irritability, and anxiety with age compared to girls with ADHD, whose symptom levels remained elevated relative to TD girls. Depressive symptoms were persistently elevated among girls with ADHD compared to boys with ADHD, whose symptoms decreased with age, relative to same-sex TD peers. While both boys and girls with ADHD showed higher levels of ED during childhood (compared to their sex-matched TD peers), mixed effects analyses revealed substantial sexually dimorphic patterns of emotional symptom change during adolescence: Boys with ADHD showed robust improvements in emotional symptoms from childhood to adolescence while girls with ADHD continued to show high and/or increased levels of ED, emotional lability, irritability, anxiety and depression.







Similar content being viewed by others
References
Shaw P, Stringaris A, Nigg J, Leibenluft E (2014) Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry 171(3):276–293. https://doi.org/10.1176/appi.ajp.2013.13070966
August GJ, Realmuto GM, MacDonald AW, Nugent SM, Crosby R (1996) Prevalence of ADHD and comorbid disorders among elementary school children screened for disruptive behavior. J Abnorm Child Psychol 24(5):571–595. https://doi.org/10.1007/BF01670101
Thompson RA (1994) Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev 59(2–3):25–52
Sobanski E et al (2010) Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. J Child Psychol Psychiatry 51(8):915–923. https://doi.org/10.1111/j.1469-7610.2010.02217.x
Biederman J, Spencer TJ, Petty C (2012) Longitudinal course of deficient emotional self-regulation CBCL profile in youth with ADHD: prospective controlled study. Neuropsychiatr Treat 8:267–276. https://doi.org/10.2147/NDT.S29670
Eyre O, Riglin L, Leibenluft E, Stringaris A, Collishaw S, Thapar A (2019) Irritability in ADHD: association with later depression symptoms. Eur Child Adolesc Psychiatry 28(10):1375–1384. https://doi.org/10.1007/s00787-019-01303-x
Galera C et al (2020) Developmental profiles of childhood attention-deficit/hyperactivity disorder and irritability: association with adolescent mental health, functional impairment, and suicidal outcomes. J Child Psychol Psychiatry 62(2):232-243. https://doi.org/10.1111/jcpp.13270
Graziano PA, Garcia A (2016) Attention-deficit hyperactivity disorder and children’s emotion dysregulation: a meta-analysis. Clin Psychol Rev 46:106–123. https://doi.org/10.1016/j.cpr.2016.04.011
Bunford N, Evans SW, Langberg JM (2018) Emotion dysregulation is associated with social impairment among young adolescents with ADHD. J Atten Disord 22(1):66–82. https://doi.org/10.1177/1087054714527793
Sjowall D, Roth L, Lindqvist S, Thorell LB (2013) Multiple deficits in ADHD: executive dysfunction, delay aversion, reaction time variability, and emotional deficits. J Child Psychol Psychiatry 54(6):619–627. https://doi.org/10.1111/jcpp.12006
Anastopoulos AD, Smith TF, Garrett ME (2011) Self-regulation of emotion, functional impairment, and comorbidity among childrenwith AD/HD. J Atten Disord 15(7):583–592. https://doi.org/10.1177/1087054710370567
Gillberg C, Gillberg IC, Rasmussen P (2004) Co–existing disorders in ADHD –implications for diagnosisand intervention. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-004-1008-4
Jensen CM, Steinhausen H-C (2015) Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. ADHD Atten Deficit Hyperact Disord 7(1):27–38. https://doi.org/10.1007/s12402-014-0142-1
Jensen PS, Hinshaw SP, Kraemer HC (2001) ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry 40(2):147–158. https://doi.org/10.1097/00004583-200102000-00009
Spencer TJ, Biederman J, Mick E (2007) Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. J Pediatr Psychol 32(6):631–642. https://doi.org/10.1093/jpepsy/jsm005
Mick E, Spencer T, Wozniak J, Biederman J (2005) Heterogeneity of irritability in attention-deficit/hyperactivity disorder subjects with and without mood disorders. Biol Psychiatry 58(7):576–582. https://doi.org/10.1016/j.biopsych.2005.05.037
Rosen PJ, Walerius DM, Fogleman ND, Factor PI (2015) The association of emotional lability and emotional and behavioral difficulties among children with and without ADHD. ADHD Atten Deficit Hyperact Disord 7(4):281–294. https://doi.org/10.1007/s12402-015-0175-0
Seymour KE, Chronis-Tuscano A, Halldorsdottir T, Stupica B, Owens K, Sacks T (2012) Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. J Abnorm Child Psychol 40(4):595–606. https://doi.org/10.1007/s10802-011-9593-4
Hinshaw SP (2003) Impulsivity, emotion regulation, and developmental psychopathology: specificity versus generality of linkages. Ann N Acad Sci 1008(1):149–159. https://doi.org/10.1196/annals.1301.016
Spencer TJ, Faraone SV, Surman CB (2011) Toward defining deficient emotional self-regulation in children with attention-deficit/hyperactivity disorder using the child behavior checklist: a controlled study. Postgrad Med 123(5):50–59
J WM, CL C (2000) Social Functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. J Clin Child Psychol 29(1):30–42. https://doi.org/10.1207/S15374424jccp2901_4
Riley AW et al (2006) Factors related to health-related quality of life (HRQoL) among children with ADHD in Europe at entry into treatment. Eur Child Adolesc Psychiatry 15(S1):i38–i45. https://doi.org/10.1007/s00787-006-1006-9
Gisbert L, Richarte V, Corrales M (2018) The impact of emotional lability symptoms during childhood in adults with ADHD. J Atten Disord 22(6):581–590. https://doi.org/10.1177/1087054717719534
Tallberg P, Svanberg K, Hallin A-L, Rastam M, Gustafsson P, Perrin S (2022) The three-year outcome of emotional symptoms in clinically referred youth with ADHD and their relationship to neuropsychological functions. Scand J Child Adolesc Psychiatry Psychol 10(1):72–86. https://doi.org/10.2478/sjcapp-2022-0008
Quach JL, Nguyen CD, Williams KE, Sciberras E (2018) Bidirectional associations between child sleep problems and internalizing and externalizing difficulties from preschool to early adolescence. JAMA Pediatr. 172(2):e174363. https://doi.org/10.1001/jamapediatrics.2017.4363
Stern A, Agnew-Blais JC, Danese A (2020) Associations between ADHD and emotional problems from childhood to young adulthood: a longitudinal genetically sensitive study. J Child Psychol Psychiatry. https://doi.org/10.1111/jcpp.13217
Biederman J et al (2010) Adult psychiatric outcomes of girls with attention deficit hyperactivity disorder: 11-year follow-up in a longitudinal case-control study. Am J Psychiatry 167(4):409–417. https://doi.org/10.1176/appi.ajp.2009.09050736
Lahey BB, Lee SS, Sibley MH, Applegate B, Molina BSG, Pelham WE (2016) Predictors of adolescent outcomes among 4–6 year old children with attention-deficit/hyperactivity disorder. J Abnorm Psychol 125(2):168–181. https://doi.org/10.1037/abn0000086
Karalunas SL, Gustafsson HC, Fair D, Musser ED, Nigg JT (2019) Do we need an irritable subtype of ADHD? Replication and extension of a promising temperament profile approach to ADHD subtyping. Psychol Assess 31(2):236–247. https://doi.org/10.1037/pas0000664
Riglin L et al (2017) Investigating the genetic underpinnings of early-life irritability. Transl Psychiatry 7(9):e1241. https://doi.org/10.1038/tp.2017.212
Heidari S, Babor TF, De Castro P, Tort S, Curno M (2016) Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev 1(1):2. https://doi.org/10.1186/s41073-016-0007-6
Conners CK (2008) Conners third edition (Conners 3). Los Angel. CA West. Psychol. Serv.
Stringaris A et al (2012) The affective reactivity index: a concise irritability scale for clinical and research settings. J Child Psychol Psychiatry 53(11):1109–1117
DeSousa DA, Stringaris A, Leibenluft E, Koller SH, Manfro GG, Salum GA (2013) Cross-cultural adaptation and preliminary psychometric properties of the affective reactivity index in Brazilian youth: implications for DSM-5 measured irritability. Trends Psychiatry Psychother 35(3):171–180. https://doi.org/10.1590/S2237-60892013000300004
Mulraney MA, Melvin GA, Tonge BJ (2014) Psychometric properties of the affective reactivity index in Australian adults and adolescents. Psychol Assess 26(1):148–155. https://doi.org/10.1037/a0034891
Tseng W-L et al (2017) Test-retest reliability and validity of a frustration paradigm and irritability measures. J Affect Disord 212:38–45. https://doi.org/10.1016/j.jad.2017.01.024
Kovacs M (1992) Children’s depression inventory: manual. Multi-Health Systems North Tonawanda, NY
March JS, Parker JDA (2004) The multidimensional anxiety scale for children (MASC). The use of psychological testing for treatment planning and outcomes assessment: Instruments for children and adolescents. Lawrence Erlbaum Associates Publishers, pp 39–62
March JS, Parker JD, Sullivan K, Stallings P, Conners CK (1997) The multidimensional anxiety scale for children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 36(4):554–565. https://doi.org/10.1097/00004583-199704000-00019
Thor Olason D, Blondahl Sighvatsson M, Smari J (2004) Psychometric properties of the multidimensional anxiety scale for children (MASC) among icelandic schoolchildren. Scand J Psychol. 45(5):429–436. https://doi.org/10.1111/j.1467-9450.2004.00424.x
Baldwin JS, Dadds MR (2007) Reliability and validity of parent and child versions of the multidimensional anxiety scale for children in community samples. J Am Acad Child Adolesc Psychiatry 46(2):252–260. https://doi.org/10.1097/01.chi.0000246065.93200.a1
Ibrahim JG, Molenberghs G (2009) Missing data methods in longitudinal studies: a review. TEST 18(1):1–43. https://doi.org/10.1007/s11749-009-0138-x
Bates D, Mächler M, Bolker B, Walker S (2015) Fitting linear mixed-effects models using lme4”. J Stat Softw. https://doi.org/10.18637/jss.v067.i01
Brysbaert M, Stevens M (2018) Power analysis and effect size in mixed effects models: a tutorial. J Cogn. 1(1):9. https://doi.org/10.5334/joc.10
Owens EB, Hinshaw SP, Lee SS, Lahey BB (2009) Few girls with childhood attention-deficit/hyperactivity disorder show positive adjustment during adolescence. J Clin Child Adolesc Psychol 38(1):132–143. https://doi.org/10.1080/15374410802575313
Hinshaw SP, Owens EB, Zalecki C (2012) Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: continuing impairment includes elevated risk for suicide attempts and self-injury. J Consult Clin Psychol 80(6):1041–1051. https://doi.org/10.1037/a0029451
Dirlikov B, Rosch KS, Crocetti D, Denckla MB, Mahone EM, Mostofsky SH (2015) Distinct frontal lobe morphology in girls and boys with ADHD. Neuroimage Clin 7:222–229
Etkin A, Egner T, Kalisch R (2011) Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn Sci 15(2):85–93
Jacobson LA, Peterson DJ, Rosch KS, Crocetti D, Mori S, Mostofsky SH (2015) Sex-based dissociation of white matter microstructure in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 54(11):938–946
Hong S-B et al (2014) Subthreshold attention-deficit/hyperactivity disorder is associated with functional impairments across domains: a comprehensive analysis in a large-scale community study. Eur Child Adolesc Psychiatry 23(8):627–636. https://doi.org/10.1007/s00787-013-0501-z
Ohan JL, Johnston C (2005) Gender appropriateness of symptom criteria for attention-deficit/hyperactivity disorder, oppositional-defiant disorder, and conduct disorder. Child Psychiatry Hum Dev 35(4):359–381. https://doi.org/10.1007/s10578-005-2694-y
Quinn PO (2008) Attention-deficit/hyperactivity disorder and its comorbidities in women and girls: an evolving picture. Curr Psychiatry Rep 10(5):419–423. https://doi.org/10.1007/s11920-008-0067-5
Chung W et al (2019) Trends in the prevalence and incidence of attention-deficit/hyperactivity disorder among adults and children of different racial and ethnic groups. JAMA Netw Open 2(11):e1914344–e1914344. https://doi.org/10.1001/jamanetworkopen.2019.14344
Bölte S, Neufeld J, Marschik PB, Williams ZJ, Gallagher L, Lai M-C (2023) Sex and gender in neurodevelopmental conditions. Nat Rev Neurol. https://doi.org/10.1038/s41582-023-00774-6
Assari S (2021) Emotional, behavioral, and cognitive correlates of attention deficit and hyperactive disorder (ADHD) screening and diagnosis history: sex/gender differences. J Neurol Neuromed 6(1):1–12. https://doi.org/10.29245/2572.942X/2021/1.1278
Gordon CT, Hinshaw SP (2019) “Executive functions in girls with and without childhood ADHD followed through emerging adulthood: developmental trajectories. J Clin Child Adolesc Psychol. https://doi.org/10.1080/15374416.2019.1602840
Zelazo PD and Cunningham WA (2007) “Executive function: mechanisms underlying emotion regulation,” Publ. Online.
Barkley RA, Fischer M (2010) The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. J Am Acad Child Adolesc Psychiatry 49(5):503–513. https://doi.org/10.1097/00004583-201005000-00011
Funding
This research was supported by the National Institutes of Health (SM: R01MH078160 and R01MH085328; KR: K23MH101322 and R03MH119457; KES: K23MH107734 and the Brain and Behavior Foundation NARSAD Young Investigator’s Award awarded to Dr. Seymour).
Author information
Authors and Affiliations
Contributions
KSR, SHM, KSR conceptualized the study, analyzed and interpreted the data, and wrote the manuscript. ACD, LR, and YZ analyzed and interpreted the data and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
This work was prepared while Dr. Karen Seymour was employed at Johns Hopkins University and Kennedy Krieger Institute. She is currently employed at the National Institutes of Health, Center for Scientific Review. The opinions expressed in this article are the author's own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De Ronda, A.C., Rice, L., Zhao, Y. et al. ADHD-related sex differences in emotional symptoms across development. Eur Child Adolesc Psychiatry (2023). https://doi.org/10.1007/s00787-023-02251-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00787-023-02251-3