Abstract
Objectives
Opiorphin is an analgesic peptide released by salivary glands and capsaicin an agonist of TRPV1 receptors eliciting burning sensations. The primary objective of this study was to assess opiorphin release after stimulation of the tongue by capsaicin (STC). The secondary objectives were to compare opiorphin release after STC in 3 groups of subjects [healthy (CTRL), Burning Mouth Syndrome (BMS), painful Temporomandibular disorders (TMDp)] and pain evoked by STC in these 3 groups.
Materials and methods
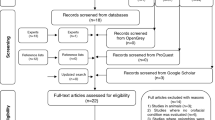
Salivary opiorphin was assessed with high-performance liquid chromatography at 3 different time points (baseline, after 5 min and 20 min of STC). Pain was self-reported on a (0–10) numeric rating scale.
Results
Three groups (N = 16) of adults were recruited at the Clinical Hospital Centre and School of Dental Medicine in Zagreb. Opiorphin levels were higher (1) in TMDp compared to CTRL in 1st (2.23 ± 1.72 pg/ul vs. 0.67 ± 0.44 pg/ul, p = 0.002) and 3rd sampling (2.44 ± 2.01 pg/ul vs. 0.74 ± 0.52 pg/ul, p = 0.020) and (2) within BMS group at 3rd sampling vs. baseline (p < 0.025). Pain scores were higher in BMS compared to TMDp (p < 0.025) and CTRL (p < 0.025).
Conclusion
This study evidenced (1) a differential basal amount of opiorphin in two pain conditions and control subjects (2) a differential kinetic of release of opiorphin after STC in CTRL, BMS and TMDp (3) a differential pain perception after STC in BMS and TMDp vs. CTRL, which can provide a readout for animal models.
Clinical relevance
The specific regulation of opiorphin release in patients with orofacial painful conditions provides valuable insights for clinicians and researchers in physiology and pathology and encourages further research in this area.
Trial registration
ClinicalTrials.gov NCT04694274. Registered on 01/05/2021.



Similar content being viewed by others
Data availability
All data associated with this study are presented in the paper.
References
Craig AD (2003) A new view of pain as a homeostatic emotion. Trends Neurosci 26(6):303–307. https://doi.org/10.1016/s0166-2236(03)00123-1
Donnelly CR, Chen O, Ji RR (2020) How do sensory neurons sense Danger signals? Trends Neurosci 43(10):822–838. https://doi.org/10.1016/j.tins.2020.07.008
Green BG (2012) Chemesthesis and the chemical senses as components of a chemofensor complex. Chem Senses 37(3):201–206. https://doi.org/10.1093/chemse/bjr119
Houghton JW, Carpenter G, Hans J, Pesaro M, Lynham S, Proctor G (2020) Agonists of orally expressed TRP channels stimulate salivary secretion and modify the salivary proteome. Mol Cell Proteomics: MCP 19(10):1664–1676. https://doi.org/10.1074/mcp.RA120.002174
Roper SD (2014) TRPs in taste and chemesthesis. Handb Exp Pharmacol 223:827–871. https://doi.org/10.1007/978-3-319-05161-1_5
Simon SA, Gutierrez R (2017) TRP Channels at the Periphery of the Taste and Trigeminal Systems. In: Emir TLR, editor. Neurobiology of TRP Channels. Boca Raton (FL): CRC Press/Taylor & Francis [cited 2020 Oct 8]. (Frontiers in Neuroscience). http://www.ncbi.nlm.nih.gov/books/NBK476105/
Kichko TI, Neuhuber W, Kobal G, Reeh PW (2018) The roles of TRPV1, TRPA1 and TRPM8 channels in chemical and thermal sensitivity of the mouse oral mucosa. Eur J Neurosci 47(3):201–210. https://doi.org/10.1111/ejn.13799
Slack JP (2016) Molecular Pharmacology of Chemesthesis - ScienceDirect [cited 2020 Oct 8]. https://www.sciencedirect.com/science/article/pii/B9780128016947000214
Arendt-Nielsen L, Carstens E, Proctor G, Boucher Y, Clavé P, Albin Nielsen K, Nielsen TA, Reeh PW (2022) The role of TRP Channels in Nicotinic provoked Pain and Irritation from the oral cavity and Throat: translating Animal Data to humans. Nicotine Tob Res 24(12):1849–1860. https://doi.org/10.1093/ntr/ntac054
Simons CT, Klein AH, Carstens E (2019) Chemogenic subqualities of Mouthfeel. Chem Senses 44(5):281–288. https://doi.org/10.1093/chemse/bjz016
Boudreau SA, Wang K, Svensson P, Sessle BJ, Arendt-Nielsen L (2009) Vascular and psychophysical effects of topical capsaicin application to orofacial tissues. J Orofac Pain 23(3):253–264
Gazerani P, Andersen OK, Arendt-Nielsen L (2007) Site-specific, dose-dependent, and sex-related responses to the experimental pain model induced by intradermal injection of capsaicin to the foreheads and forearms of healthy humans. J Orofac Pain 21(4):289–302
Rougeot C, Rosinski-Chupin I, Mathison R, Rougeon F (2000) Rodent submandibular gland peptide hormones and other biologically active peptides. Peptides 21(3):443–455. https://doi.org/10.1016/S0196-9781(00)00158-3
Wisner A, Dufour E, Messaoudi M, Nejdi A, Marcel A, Ungeheuer MN et al (2006) Human opiorphin, a natural antinociceptive modulator of opioid-dependent pathways. Proc Natl Acad Sci USA 21(47):17979–17984. https://doi.org/10.1073/pnas.0605865103
Rosa M, Arsequell G, Rougeot C, Calle LP, Marcelo F, Pinto M et al (2012) Structure-activity relationship study of opiorphin, a human dual ectopeptidase inhibitor with antinociceptive properties. J Med Chem 9(3):1181–1188. https://doi.org/10.1021/jm2012112
Sitbon P, Van Elstraete A, Hamdi L, Juarez-Perez V, Mazoit JX, Benhamou D et al (2016) STR-324, a stable Analog of Opiorphin, causes Analgesia in Postoperative Pain by activating endogenous opioid receptor-dependent pathways. Anesthesiology 125(5):1017–1029. https://doi.org/10.1097/ALN.0000000000001320
Van Elstraete A, Sitbon P, Hamdi L, Juarez-Perez V, Mazoit JX, Benhamou D et al (2018) The Opiorphin Analog STR-324 decreases sensory hypersensitivity in a rat model of Neuropathic Pain. Anesth Analg 126(6):2102–2111. https://doi.org/10.1213/ANE.0000000000002413
Luo P, Li X, Gao Y, Chen Z, Zhang Q, Wang Z et al (2022) Central administration of human opiorphin alleviates dextran sodium sulfate-induced colitis in mice through activation of the endogenous opioid system. Front Pharmacol 13:904926. https://doi.org/10.3389/fphar.2022.904926
Porporatti AL, Oliveira Machado AA, Alajbeg I, Alajbeg IZ, Paszynka E, Dmitrzak-Weglarz M et al (2022) Opiorphin as a biomarker of orofacial conditions: a meta-analysis. Sci Rep 13(1):15533. https://doi.org/10.1038/s41598-023-42051-y
Zlendić M, Vrbanović E, Tomljanović M, Gall Trošelj K, Đerfi KV, Alajbeg IZ (2023) Association of oral behaviours and psychological factors with selected genotypes in pain-related TMD. Oral Dis. https://doi.org/10.1111/odi.14583
Vandenbroucke JP, Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ et al (2014) Strengthening the reporting of Observational studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg 12(12):1500–1524. https://doi.org/10.1016/j.ijsu.2014.07.014
Haefeli M, Elfering A (2006) Pain assessment. Eur Spine J 15(Suppl 1):S17–24. https://doi.org/10.1007/s00586-005-1044-x
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP et al (2014) Diagnostic criteria for Temporomandibular disorders (DC/TMD) for clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache 28(1):6–27. https://doi.org/10.11607/jop.1151
Salarić I, Sabalić M, Alajbeg I (2017) Opiorphin in burning mouth syndrome patients: a case-control study. Clin Oral Investig 21(7):2363–2370. https://doi.org/10.1007/s00784-016-2031-9
Ngom PI, Dubray C, Woda A, Dallel R (2001) A human oral capsaicin pain model to assess topical anesthetic-analgesic drugs. Neurosci Lett 28(3):149–152. https://doi.org/10.1016/s0304-3940(01)02401-6
Dessirier JM, O’Mahony M, Sieffermann JM, Carstens E (1998) Mecamylamine inhibits nicotine but not capsaicin irritation on the tongue: psychophysical evidence that nicotine and capsaicin activate separate molecular receptors. Neurosci Lett 9(2):65–68. https://doi.org/10.1016/s0304-3940(97)00930-0
Brkljačić L, Sabalić M, Salarić I, Jerić I, Alajbeg I, Nemet I (2011) Development and validation of a liquid chromatography-tandem mass spectrometry method for the quantification of opiorphin in human saliva. J Chromatogr B Analyt Technol Biomed Life Sci 15(32):3920–3926. https://doi.org/10.1016/j.jchromb.2011.11.003
Boucher Y, Braud A, Dufour E, Agbo-Godeau S, Baaroun V, Descroix V et al (2016) Opiorphin levels in fluids of burning mouth syndrome patients: a case-control study. Clin Oral Investig 21(7):2157–2164. https://doi.org/10.1007/s00784-016-1991-0
Ruangsri S, Jorns TP, Chaiyarit P (2019) Opiorphin Level in Unstimulated Whole Saliva of Burning Mouth Syndrome Patients. Journal of the medical association of Thailand 102(4):63
Hu X, Ayed C, Chen J, Fisk I, Yang N (2022) The role of capsaicin stimulation on the physicochemical properties of saliva and aroma release in model aqueous and oil systems. Food Chem 30:386:132824. https://doi.org/10.1016/j.foodchem.2022.132824
Cairns BE (2010) Pathophysiology of TMD pain–basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil 37(6):391–410. https://doi.org/10.1111/j.1365-2842.2010.02074.x
Kolkka M, Forssell H, Virtanen A, Puhakka A, Pesonen U, Jääskeläinen SK (2019) Neurophysiology and genetics of burning mouth syndrome. Eur J Pain 23(6):1153–1161. https://doi.org/10.1002/ejp.1382
Mendak-Ziółko M, Konopka T, Bogucki ZA (2012) Evaluation of select neurophysiological, clinical and psychological tests for burning mouth syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol 114(3):325–332. https://doi.org/10.1016/j.oooo.2012.04.004
Cairns BE (2022) The contribution of autonomic mechanisms to pain in temporomandibular disorders: a narrative review. J Oral Rehabil 49(11):1115–1126. https://doi.org/10.1111/joor.13370
Javelot H, Messaoudi M, Garnier S, Rougeot C (2010) Human opiorphin is a naturally occurring antidepressant acting selectively on enkephalin-dependent delta-opioid pathways. J Physiol Pharmacology: Official J Pol Physiological Soc 61(3):355–362
Maraschin JC, Rangel MP, Bonfim AJ, Kitayama M, Graeff FG, Zangrossi H et al (2016) Opiorphin causes a panicolytic-like effect in rat panic models mediated by µ-opioid receptors in the dorsal periaqueductal gray. Neuropharmacology 101:264–270. https://doi.org/10.1016/j.neuropharm.2015.09.008
Mokhtar M, Singh P (2022) Neuroanatomy, Periaqueductal Gray. In: StatPearls. StatPearls Publishing; [cited 2023 May 16]. https://www.ncbi.nlm.nih.gov/books/NBK554391/
Yang QZ, Lu SS, Tian XZ, Yang AM, Ge WW, Chen Q (2011) The antidepressant-like effect of human opiorphin via opioid-dependent pathways in mice. Neurosci Lett 489(2):131–135. https://doi.org/10.1016/j.neulet.2010.12.002
Sestile CC, Maraschin JC, Rangel MP, Santana RG, Zangrossi H, Graeff FG et al (2017) B2-kinin receptors in the dorsal periaqueductal gray are implicated in the panicolytic-like effect of opiorphin. Prog Neuropsychopharmacol Biol Psychiatry 79(Pt B):493–498
Slade GD, Ohrbach R, Greenspan JD, Fillingim RB, Bair E, Sanders AE et al (2016) Painful temporomandibular disorder: Decade of Discovery from OPPERA studies. J Dent Res 95(10):1084–1092. https://doi.org/10.1177/0022034516653743
Jääskeläinen SK (2018) Is burning mouth syndrome a neuropathic pain condition? Pain 159(3):610–613. https://doi.org/10.1097/j.pain.0000000000001090
Porporatti AL, Schroder ÂGD, Lebel A et al (2023) Is burning mouth syndrome associated with stress? A meta-analysis. J Rehabil. https://doi.org/10.1111/joor.13536
Ozdogan S, Sonmez C, Yolcu D, Gungormus M (2020) Tear Opiorphin levels in Ocular Pain caused by corneal foreign body. Cornea 39(11):1377–1380. https://doi.org/10.1097/ICO.0000000000002383
Grushka M (1987) Clinical features of burning mouth syndrome. Oral Surg Oral Med Oral Pathol 63(1):30–36. https://doi.org/10.1016/0030-4220(87)90336-7
Forssell H, Jääskeläinen S, Tenovuo O, Hinkka S (2002) Sensory dysfunction in burning mouth syndrome. Pain 99(1–2):41–47. https://doi.org/10.1016/s0304-3959(02)00052 – 0
Lauria G, Majorana A, Borgna M, Lombardi R, Penza P, Padovani A et al (2005) Trigeminal small-fiber sensory neuropathy causes burning mouth syndrome. Pain 115(3):332–337. https://doi.org/10.1016/j.pain.2005.03.028
Simons CT, Carstens E (2020) 3.20 - Oral Chemesthesis and Taste. In: Fritzsch B, editor. The Senses: A Comprehensive Reference (Second Edition). Oxford: Elsevier; [cited 2023 May 18]. pp. 398–422. https://www.sciencedirect.com/science/article/pii/B9780128093245241382
Silvestre FJ, Silvestre-Rangil J, Tamarit-Santafé C, Bautista D (2012) Application of a capsaicin rinse in the treatment of burning mouth syndrome. Med Oral Patol Oral Cir Bucal 17(1):e1–4. https://doi.org/10.4317/medoral.17219
Jørgensen MR, Pedersen AML (2017) Analgesic effect of topical oral capsaicin gel in burning mouth syndrome. Acta Odontol Scand 75(2):130–136. https://doi.org/10.1080/00016357.2016.1269191
Winocur E, Gavish A, Halachmi M, Eli I, Gazit E (2000) Topical application of capsaicin for the treatment of localized pain in the temporomandibular joint area. J Orofac Pain 14(1):31–36
Campbell BK, Fillingim RB, Lee S, Brao R, Price DD, Neubert JK (2017) Effects of High-Dose Capsaicin on TMD subjects: a Randomized Clinical Study. JDR Clin Trans Res 2(1):58–65. https://doi.org/10.1177/2380084416675837
Baad-Hansen L, List T, Kaube H, Jensen TS, Svensson P (2006) Blink reflexes in patients with atypical odontalgia and matched healthy controls. Exp Brain Res 172(4):498–506. https://doi.org/10.1007/s00221-006-0358-1
Boucher Y, Carstens MI, Sawyer CM, Zanotto KL, Merrill AW, Carstens E (2013) Capsaicin avoidance as a measure of chemical hyperalgesia in orofacial nerve injury models. Neurosci Lett 24543:37–49. https://doi.org/10.1016/j.neulet.2013.02.060
Boucher Y, Simons CT, Carstens MI, Carstens E (2014) Effects of gustatory nerve transection and/or ovariectomy on oral capsaicin avoidance in rats. Pain 155(4):814–820. https://doi.org/10.1016/j.pain.2014.01.020
Yilmaz Z, Renton T, Yiangou Y, Zakrzewska J, Chessell IP, Bountra C et al (2007) Burning mouth syndrome as a trigeminal small fibre neuropathy: increased heat and capsaicin receptor TRPV1 in nerve fibres correlates with pain score. J Clin Neurosci 14(9):864–871. https://doi.org/10.1016/j.jocn.2006.09.002
Just T, Steiner S, Pau HW Oral pain perception and taste in burning mouth syndrome (2010). J Oral Pathol Med 39(1):22–27. https://doi.org/10.1111/j.1600-0714.2009.00824.x
Gremeau-Richard C, Pionchon P, Mulliez A, Dualé C, Dallel R (2022) Enhanced pain facilitation rather than impaired pain inhibition in burning mouth syndrome female patients. J Headache Pain 23(1):143. https://doi.org/10.1186/s10194-022-01516-7
Grushka M, Sessle BJ, Howley TP (1987) Psychophysical assessment of tactile, pain and thermal sensory functions in burning mouth syndrome. Pain 28(2):169–184 10.1016/0304–3959(87)90114-X
Yang G, Su S, Jie H, Baad-Hansen L, Wang K, Yan S et al (2019) Somatosensory profiling of patients with burning Mouth Syndrome and correlations with psychologic factors. J Oral Facial Pain Headache 33(3):278–286. https://doi.org/10.11607/ofph.2358
Wolowski A, Schwarzbach N, Hörning H (2021) Thermal quantitative sensory testing in burning mouth syndrome. Clin Oral Investig 25(5):3059–3066. https://doi.org/10.1007/s00784-020-03626-5
Ozasa K, Noma N, Young A, Korczeniewska OA, Eliav E, Imamura Y (2022) Potential differences in somatosensory function during premenopause and early and late postmenopause in patients with burning mouth syndrome: an observational case-control study. J Dent Sci 17(1):399–406. https://doi.org/10.1016/j.jds.2021.08.010
Dufour E, Villard-Saussine S, Mellon V, Leandri R, Jouannet P, Ungeheuer M et al (2013) Opiorphin Secretion Pattern in Healthy Volunteers: Gender Difference and Organ Specificity. Biochemistry & Analytical Biochemistry [cited 2016 Jan 19]. http://www.omicsonline.org/biochemistry-and-analytical-biochemistry-abstract.php?abstract_id=15749
Acknowledgements
This research was funded by the Croatian Science Foundation Project “Genetic polymorphisms and their association with temporomandibular disorders”, grant number [IP-2019-04-6211] and by LabNOF recurrent funding.
Author information
Authors and Affiliations
Contributions
I.Z.A. conducted the research, wrote the manuscript, performed statistical analysis of the data, interpreted the results, managed the Croatian team and workflow, coordinated the analytical laboratory, and recruited TMD patients. E.V. wrote the manuscript, conducted the clinical portion of the experiment, recruited TMD patients, and presented the results. I.A. established the clinical portion of the experiment, recruited BMS patients, and provided research guidance. I.O. conducted the clinical portion of the experiment, presented the results, and analyzed the data. K.N. conducted the clinical portion of the experiment and presented the results. A.M. conducted the clinical portion of the experiment. Y.B. conceived the idea, designed and conceptualized the study, wrote a major part of the manuscript, and edited it. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alajbeg, I.Z., Vrbanovic, E., Alajbeg, I. et al. Time-course of pain and salivary opiorphin release in response to oral capsaicin differ in burning mouth syndrome patients, temporomandibular disorders patients and control subjects. Clin Oral Invest 28, 246 (2024). https://doi.org/10.1007/s00784-024-05653-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05653-y