Abstract
Objectives
This study aims to determine the association between severe mental disorders and oral health among individuals over 18 years of age.
Methods
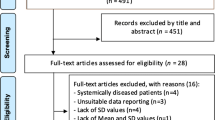
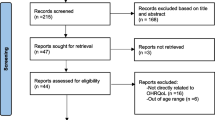
An electronic search was conducted in six electronic databases and gray literature. Qualitative and quantitative analyses were performed on studies that met the inclusion criteria. The methodology of the included studies was assessed using the Joanna Briggs Institute Critical Appraisal tool. A meta-analysis of proportions with a random effect was carried out. The certainty of evidence was evaluated using the GRADE tool.
Results
After searching the databases, 5,734 references were retrieved, and twenty articles were selected for synthesis. Considering the DMFT index between the groups with mental disorders and the control group, the values of the DMFT index were higher among individuals with schizophrenia [MD = 5.27; 95% CI = 4.13 – 6.42; I2 = 35%] and bipolar disorder [MD = 1.90; 95% CI = 0.87 – 2.93]. Values were lower among individuals with obsessive–compulsive disorder [MD = -0.85; 95% CI = -1.46—0.24]. The risk of bias was considered low for 16 studies, and four were classified with a moderate risk of bias. The certainty of evidence was very low.
Conclusion
Patients with schizophrenia and bipolar disorder exhibit increased frequency in the number of decayed, missing, or filled teeth. There was no effect in relation to periodontal probing depth, plaque index, and TMD, but the evidence is still uncertain for this outcome.
Clinical relevance
These findings underscore the need for a comprehensive health approach.




Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
World Health Organization (2017) Depression and other common mental disorders global health estimates. Geneva: World Health Organization. https://iris.who.int/handle/10665/254610
Santomauro DF, Mantilla Herrera AM, Shadid J et al (2021) Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet 398:1700–1712. https://doi.org/10.1016/S0140-6736(21)02143-7
Institute for Health Metrics and Evaluation (2022) Global health data exchange 2019. University of Washington. https://ghdx.healthdata.org/
Australian Bureau of Statistics (2022) National study of mental health and wellbeing, 2020-2022. Australian Government. https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/2020-2022. Accessed 11 Nov 2022
Patricio Marquez B V, Saxena S (2016) Making Mental Health a Global Priority. Cerebrum 1:2016:cer-10-16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5198754/
Patel V, Chisholm D, Parikh R et al (2016) Addressing the burden of mental, neurological, and substance use disorders: Key messages from Disease Control Priorities, 3rd edition. The Lancet 387:1672–1685
Necho M, Tsehay M, Birkie M et al (2021) Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Int J Soc Psychiatry 67:892–906
Qiu J, Shen B, Zhao M et al (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatr 33:e100213. https://doi.org/10.1136/gpsych-2020-100213
Chaix B, Delamon G, Guillemassé A et al (2020) Psychological distress during the COVID-19 pandemic in France: A national assessment of at-risk populations. Gen Psychiatr 33. https://doi.org/10.1136/gpsych-2020-100349
Daugherty B, Warburton K, Stahl SM (2020) A social history of serious mental illness. CNS Spectr 25:584–592
Fanelli G, Benedetti F, Kasper S et al (2021) Higher polygenic risk scores for schizophrenia may be suggestive of treatment non-response in major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry 108. https://doi.org/10.1016/j.pnpbp.2020.110170
Manji F, Fejerskovi O (1990) Dental caries in developing countries in relation to the appropriate use of fluoride. Journal of Dental Research 69:733–41. https://doi.org/10.1177/00220345900690S143
Abdalla-Aslan R, Findler M, Zini A, Almoznino G (2021) Caries experience, periodontal status, and metabolic morbidity in patients with psychiatric disorders. Quintessence Int (Berl) 52:516–526. https://doi.org/10.3290/j.qi.b1044091
Torales J, Barrios I, González I (2017) Problemáticas de salud bucodental en personas con trastornos mentales. Medwave 17:e7045
Aldosari M, Helmi M, Kennedy EN et al (2020) Depression, periodontitis, caries and missing teeth in the USA, NHANES 2009–2014. Fam Med Community Health 8. https://doi.org/10.1136/fmch-2020-000583
Cademartori MG, Gastal MT, Nascimento GG et al (2018) Is depression associated with oral health outcomes in adults and elders? A systematic review and meta-analysis. Clin Oral Investig 22:2685–2702
Kisely S, Baghaie H, Lalloo R et al (2015) A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom Med 77:83–92
Yang M, Chen P, He MX et al (2018) Poor oral health in patients with schizophrenia: A systematic review and meta-analysis. Schizophr Res 201:3–9
Sun XN, Zhou JB, Li N (2021) Poor oral health in patients with schizophrenia: a meta-analysis of case-control studies. Psychiatr Q 92:135–145. https://doi.org/10.1007/s11126-020-09752-3
Page MJ, Moher D, Bossuyt PM et al (2021) PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. The BMJ 372. https://doi.org/10.1136/bmj.n160
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22:276–282
Aromataris E, Munn Z (Editors) (2020) JBI Manual for Evidence Synthesis. JBI. Available from https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-24-01
Abreu M, da Silva A, Cavalcanti R et al. (2022) Prevalence of chewing difficulty in older people in long-term care: A systematic review and meta-analysis. Gerodontology 40(1):10–25. https://doi.org/10.1111/ger.12617
Manheimer E (2012) Summary of findings tables: Presenting the main findings of cochrane complementary and alternative medicine-related reviews in a transparent and simple tabular format. Glob Adv Health Med 1:90–91
Luca M, Luca A, Grasso V, Calandra C (2014) Nothing to smile about. Neuropsychiatr Dis Treat 10:1999–2008
Cunha FA, Cota LOM, Cortelli SC et al (2019) Periodontal condition and levels of bacteria associated with periodontitis in individuals with bipolar affective disorders: A case-control study. J Periodontal Res 54:63–72. https://doi.org/10.1111/jre.12605
Kumar A, Kardkal A, Debnath S, Lakshminarayan J (2015) Association of periodontal health indicators and major depressive disorder in hospital outpatients. J Indian Soc Periodontol 19:507–511. https://doi.org/10.4103/0972-124X.167161
GurbuzOflezer O, Altinbas K, Delice M et al (2018) Oral health among patients with bipolar disorder. Oral Health Prev Dent 16:509–516. https://doi.org/10.3290/j.ohpd.a41662
Velasco-Ortega E, Monsalve-Guil L, Ortiz-Garcia I et al (2017) Dental caries status of patients with schizophrenia in Seville, Spain: a case-control study. BMC Res Notes 10:1–7. https://doi.org/10.1186/s13104-016-2368-9
Battistella CB, Guimarães TB, Quaglio CL et al (2016) Biopsychosocial factors of axis II of the research diagnostic criteria for temporomandibular disorders in individuals with muscular temporomandibular disorder and migraine. Revista Dor 17:19–23. https://doi.org/10.5935/1806-0013.20160006
Fredricson AS, Weiner CK, Adami J et al (2022) The role of mental health and behavioral disorders in the development of temporomandibular disorder: A SWEREG-TMD nationwide case-control study. J Pain Res 15:2641–2655. https://doi.org/10.2147/JPR.S381333
Albahli BF, Alrasheed NM, Alabdulrazaq RS et al (2021) Association between schizophrenia and periodontal disease in relation to cortisol levels: an ELISA-based descriptive analysis. Egypt J Neurol Psychiatr Neurosurg 57. https://doi.org/10.1186/s41983-021-00423-z
Rosa LK, Costa FS, Hauagge CM et al (2021) Oral health, organic and inorganic saliva composition of men with Schizophrenia: Case-control study. J Trace Elem Med Biol 66. https://doi.org/10.1016/j.jtemb.2021.126743
Djordjević V, Jovanović M, Miličić B et al (2016) Prevalence of dental caries in hospitalized patients with schizophrenia. Vojnosanit Pregl 73:1102–1108. https://doi.org/10.2298/VSP150917111D
Rehm D, Progiante P, Pattussi M et al (2019) Depression and Somatization in Patients with Temporomandibular Disorders in a Population-Based Cross-Sectional Study in Southern Brazil. Int J Prosthodont 32:248–250. https://doi.org/10.11607/ijp.6209
Arnaiz A, Zumárraga M, Díez-Altuna I et al (2011) Oral health and the symptoms of schizophrenia. Psychiatry Res 188:24–28. https://doi.org/10.1016/j.psychres.2010.09.012
Krunić J, Stojanović N, Ivković N, Stojić D (2013) Salivary flow rate and decayed, missing, and filled teeth (DMFT) in female patients with schizophrenia on chlorpromazine therapy. J Dent Sci 8:418–424. https://doi.org/10.1016/j.jds.2013.05.004
Moghadam SA, Masjedi O, Fakour SR, Moghaddam AA (2016) The association between psychological disorders and periodontitis. Int J High Risk Behav Addict 5:0–4. https://doi.org/10.5812/ijhrba.21684
Moharrami M, Perez A, Mohebbi SZ et al (2022) Oral health status of individuals with obsessive-compulsive disorder considering oral hygiene habits. Spec Care Dentist 42:41–48. https://doi.org/10.1111/scd.12632
Scepanovic M, Djordjevic V, Stasevic-Karlicic I et al (2021) Oral health of prosthetic rehabilitated patients with schizophrenia. Srp Arh Celok Lek 149:275–281. https://doi.org/10.2298/sarh201109002s
D’Avilla BM, Pimenta MCB, Furletti VF et al (2019) Comorbidity of TMD and malocclusion: Impacts on quality of life, masticatory capacity and emotional features. Braz J Oral Sci 18:1–10. https://doi.org/10.20396/BJOS.V18I0.8657272
Huang YK, Wang YH, Chang YC (2020) Chronic periodontitis is associated with the risk of bipolar disorder: A population-based cohort study. Int J Environ Res Public Health 17. https://doi.org/10.3390/ijerph17103466
Chang KH, Hsu YC, Chiu IM et al (2020) Association between periodontitis and bipolar disorder: A nationwide cohort study. Medicine (United States) 99. https://doi.org/10.1097/MD.0000000000021423
Gurbuz O, Alatas G, Kurt E (2009) Prevalence of temporomandibular disorder signs in patients with schizophrenia. J Oral Rehabil 36:864–871. https://doi.org/10.1111/j.1365-2842.2009.02008.x
Al-Mobeeriek A (2012) Oral health status among psychiatric patients in Riyadh, Saudi Arabia. West Indian Med J 61:549–554. https://doi.org/10.7727/wimj.2012.006
dos Santos D L N, Galvão-Moreira L V, Ribeiro M L, et al (2018) Perspectiva multiprofissional sobre a saúde bucal de pacientes de uma instituição psiquiátrica. Revista De Pesquisa Em Saúde 19- 29-32
Kisely S, Sawyer E, Siskind D, Lalloo R (2016) The oral health of people with anxiety and depressive disorders - A systematic review and meta-analysis. J Affect Disord 200:119–132
Acknowledgements
To the Center of Advanced Studies in Systematic Review and Meta-analysis (NARSM) for the support in the construction of the study
Funding
No specific grant was given to this research by funding organizations in the public, private, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
J.R, A. B, L.L, B.A, contributed to conception, design, data acquisition, drafted and critically revised the manuscript; J.N, O.F, M.R contributed to the writing and critical review of the study; J.R, B.A, K.T contributed to the writing, evaluation by the GRADE tool and prepared figures; K.T and C.A, coordinated the team, performed the meta-analyses and critically reviewed the article. All authors gave final approval and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable.
Consent for publication
All authors consent to the publication of this work.
Competing interests
The authors declare no competing interests.
Registration
The protocol for this systematic review was registered at the PROSPERO® website (International Prospective Register of Systematic Review—Center for Reviews and Dissemination University of York) under no. CRD42021276419.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rangel, J.P.A., Borges, A.F.M., Leão, L.O. et al. Oral health of people with emotional disorders: A systematic review and meta-analysis. Clin Oral Invest 28, 274 (2024). https://doi.org/10.1007/s00784-024-05642-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05642-1