Abstract
Objective
This review assessed the impact of oral conditions on Oral Health Related Quality of Life among Indians.
Methods
Databases, including PubMed and Scopus, CINAHL, Web of Science, PsycInfo were systematically searched for English Language studies conducted among Indians up to July 2022. Two independent reviewers assessed studies selected for retrieval for methodological quality using standardised quality assessment instruments for analytical cross-sectional studies in JBI SUMARI.
Results
Fourty one publications were included in this review (N = 23,090). Studies includes both cross sectional study and Randomized Controlled Trials. Based on the JBI critical appraisal tools, the quality of the included studies was low to high. Twenty-six studies were considered for the meta-analysis. Individuals with dental caries [OR: 3.54 (95% CI 2.24- 5.60), ten studies, 4945 participants] and malocclusion [ OR: 5.44 (95% CI 1.61, 18.39), six studies, 3720 participants] had poor OHRQoL compared to individuals without oral conditions.
Conclusions
Despite the various definitions of the exposures and instruments used to assess Oral Health-Related Quality of Life, our review found that people with dental caries and malocclusion have a significantly higher experience of poor quality of life.
Prospero Systematic Review Registration No.
CRD42021277874.
Similar content being viewed by others
Introduction
Oral health is a crucial indicator of general health, well-being, and Quality of life [1]. The World Health Organization (WHO) associates a "person's capacity to bite, chew, smile, and speak with their psychosocial status when defining oral health as a disorder-free state" [2]. Oral health conditions affect 3.5 billion people worldwide, according to the Global Burden of Disease Study 2017 [3]. Oral conditions are becoming more common in most lower- and middle-income countries as a result of increased urbanisation and lifestyle changes [4].
In India, the frequency of dental caries is 49%, 60%, and 84% among young children, adults, and the elderly [5]. Nearly half of the Indian population experiences levels of periodontal disease [6]. Complete tooth mortality is 10.7%, and partial tooth mobility is 58.8% [7]. The prevalence of malocclusion among children aged 8 to 15 is 35.40% [8]), and 15 states in India are endemic to fluorosis. Oral cancer is the most common in India, accounting for one-third of the global burden [9]. Oral conditions are linked with low Oral Health-Related Quality of Life (OHRQoL) [10].
"Oral Health-Related Quality of Life is integral to general health and well-being" [11]. 'Oral health status' nomenclature is now considered 'Oral Health-Related Quality of Life [12].
Quality of life (QoL) refers to a person's position in life "within the context of the culture and value systems in which they live and for their objectives, expectations, standards, and concerns" [13]. Quality of Life is a valid criterion for evaluating patients in many physical and mental healthcare areas, including dental health. Cohen and Jago [14] were among the first to advocate for the development of socio-dental indicators, as studies showed that oral conditions and their consequences interact with social life. The subjective assessment of OHRQoL "reflects people's comfort while eating, sleeping, and participating in social interaction; their sense of self-worth; and their satisfaction with their oral health" [15]. The OHRQoL is the outcome of a complex interaction between and among oral health problems, social and contextual attributes [16], and the rest of one's body [17].
Positive and negative perceptions of oral health and health outcomes have been incorporated into HRQoL and OHRQoL due to the growing emphasis on health policy that addresses health promotion and illness prevention [18]. The various tools available to assess the OHRQoL include the Early Childhood Oral Health Impact Scale (ECOHIS) [19], Child Oral Impact on Daily Performances (Child-OIDP) [20], Scale of Oral Health Outcomes (SOHO) [21], The Child Perceptions Questionnaire for children aged 8 to 10 years [22], The Child Perceptions Questionnaire for children aged 11 to 14 years (CPQ11-14) [23], Oral Health Impact Profile for 14 items (OHIP-14) [24], Oral Impacts on Daily Performances (OIDP) [25], Dental Impact on Daily Living (DIDL) [26], Geriatric Oral Health Assessment Index (GOHAI) [27], Dental Impact profile (DIP) [28], Social Impact on Dental Disease (SIDD) [28].
When identifying suitable treatment goals and outcomes, OHRQoL assessment allows a shift away from conventional medical/dental criteria and toward evaluation and care that focuses on a people's psychological and social experience as well as physical functionality [29]. Understanding the impact of oral problems on OHRQoL is crucial for the public health system, research, and decision-making on methods for improving and preventing oral health [2]. OHRQoL has been deemed a health priority by the U.S. Surgeon General [15], and "QoL concerns are now at the forefront of public health policy" [12].
Few systematic reviews have examined the effects of certain oral conditions on OHRQoL, Early Childhood Caries [30], Periodontal disease [31], Traumatic Dental Injuries (TDI) [32], and malocclusion [33]. An earlier review assessed impacts of oral disease on OHRQoL irrespective of geographical locations, with less representative Indian studies [34] and among the Latin American and Caribbean populations [2]. As OHRQoL is based on the social and cultural context [12] this review will helps in assessing impact of oral conditions on OHRQoL among Indians.
Over the last decade, several studies have assessed certain oral conditions affecting OHRQoL among the Indian population showing inconclusive impact. Therefore, a preliminary search was conducted using PROSPERO, MEDLINE, the Cochrane Database of Systematic Reviews, and the JBI Database of Systematic Reviews. This search revealed no systematic reviews with meta-analyses currently in progress or published on the effect of oral conditions on OHRQoL among Indians. Since OHRQoL is a subjective perception based on the social context, the evidence of oral conditions' impact is vital for health policy and programs. Patients' subjective evaluations of the healthcare decision-making process are changing the dynamics of healthcare delivery, current health monitoring, and research [35]. As a result, this study aimed to perform a systematic review of studies conducted in India to determine how oral conditions affected OHRQoL.
Review question
What is the Impact of oral conditions (E) on oral health and quality of life (O) when compared to individuals without oral conditions (C) among Indians (P)?
Methodology
For the systematic review report, the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines [36] were followed and registered in the prospective international register of systematic reviews (PROSPERO) under the registration number CRD42021277874.
Cross-sectional studies and Randomised Controlled Trials that addressed associations between oral conditions (Dental caries, Gingivitis, Periodontal Disease, Malocclusion, Dental Fluorosis, Tooth Loss, and Prosthetic Need) and OHRQoL were included.
The outcome was the OHRQoL assessed by instruments such as CPQ 11-14 [23], ECOHIS [19], FIS (Family Impact Scale) [37], GOHAI [27], OHIA (Oral Health Impact in Adolescents) [38], OHIP-14 (Oral Health Impact Profile) [24], OIDP [25] and WHOQoL (World Health Organization Quality of Life) [39].
Literature search strategy
For the literature search, a three-step search strategy was used. An initial MEDLINE search was conducted using the keywords "Oral disease," "Quality of Life," and "Indian population." After combining keywords and synonyms with the Boolean terms "AND" and "OR," a search string was created. Second, text words from the title, abstract, and index terms of the identified studies were used to inform the development of a search strategy tailored to each information source. PubMed, Scopus, CINAHL, Web of Science, and PsycInfo were among the databases searched for published studies. To broaden the search, Google Scholar was also used. Supplementary material (S1) shows the search strategy of different databases. The third step involved reviewing the reference lists of all study chosen for critical appraisal in order to find additional information.
Study selection
Following the electronic search, all citations found were compiled and uploaded to Covidence, and duplicates were removed. Both titles and abstracts were evaluated by two investigators (A.J. and R.V.M.). In the event of ambiguity, the full text was read for a joint decision. The full texts of the abstracts that were screened were obtained and evaluated for eligibility. Any disagreement about whether a study should be included was discussed between the two reviewers until a mutual agreement was reached or a third reviewer (C.J.) was approached. Supplementary material (S2) shows the studies ineligible following full text review.
Assessment of the methodological quality
After the ineligible studies were excluded, the quality of the eligible studies was assessed by two independent reviewers (A.R.S. and S.V.K) using standardised critical appraisal instruments for analytical cross-sectional studies in JBI SUMARI. The same checklist was used for experimental studies to assess how baseline data was collected and analysed, as that was the desired outcome [40]. In the event of disagreement, a third reviewer's (C.J.) opinion was sought for further discussion. There were eight questions, with answers ranging from "yes," "no," "unclear," and "not applicable." Each study received an overall score based on several "Yes" responses ranging from 0 to 8. Finally, studies were classified based on their score: 0–3, low quality; 4–6, medium quality; and 7–8, high quality [36].
Data extraction
Data from the included studies were extracted using the customised tool. Each study's data was extracted by two independent reviewers (A.J. and R.V.M). The extracted data included specific details about the study's characteristics, population characteristics, and outcome measures. To ensure consistency during the extraction process, the two independent reviewers met and compared the extracted data from each included study in a Microsoft Word document. No studies necessitated additional information from the corresponding authors.
Data synthesis
Studies, where possible, were pooled in a statistical meta-analysis using JBI SUMARI software. Data were presented as either odds ratios (for binary outcome) and weighted (or standardized) mean differences (for continuous measures) and their 95% confidence intervals. The standard χ2, Tau2, and I2 tests were used to assess heterogeneity. To estimate the pooled effect, the random-effects model with heterogeneity taken from an inverse variance model was used. Subgroup analyses were conducted for dental caries based on the tool to assess the OHRQoL. When statistical pooling was impossible, or when there is less than four studies to pool the data the findings were presented in descriptive form.
Assessing the certainty of the findings
The two reviewers independently assessed the evidence's certainty using the Grading of Recommendations Assessment, Development and Evaluations (GRADE Approach). The certainty of the evidence for the comparison (oral conditions and Quality of Life) was classified as ‘moderate’ for dental caries and prosthetic need and 'very low' for malocclusion, gingivitis, periodontal disease and functional edentulism. There was a downgrade in the level of evidence due to the methodological quality of the studies, small sample size, and heterogeneity. A summary of the findings table using 'Gradepro' software was generated. Figure 1 shows the summary of the GRADE assessment for the binary outcome.
Results
Study inclusion
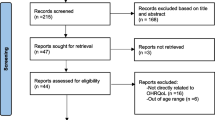
A comprehensive and detailed search of the literature yielded 2381 identified records, with 75 additional records found through other resources, for a total sample size of 2456 studies. 728 duplicates were removed from the 2456 articles, leaving 1728 records to be reviewed by title and abstract. After reviewing the titles and abstracts, we determined that 1545 did not meet our eligibility requirements. As a result, 183 articles were retrieved for full-text evaluation, 142 of which were rejected because they did not meet the eligibility criteria. Thus, 41 studies were considered for the systematic review: fifteen studies for qualitative synthesis and twenty-six studies for meta-analysis. The PRISMA flowchart search and review process for study selection and inclusion is depicted in Fig. 2.
Methodological quality
All the included studies underwent critical appraisal. No studies were excluded based solely on the assessment of methodological quality. Out of 41 studies, 16 studies were of high quality [41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56], 17 studies of medium quality [38, 57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72], and eight studies of low quality [73,74,75,76,77,78,79,80]. Only nine of 41 included studies had a low risk of bias. Most included studies used validated and reliable tools to measure exposure and outcome (Q3 and Q7). While most of the included studies failed to address the confounding issues (Q6). The methodological quality of all 41 publications evaluated is summarised in Table 1.
Characteristics of the included studies
Table 2 summarises the details of the current systematic review, which included 41 articles for descriptive analysis. Except for one study by Singh N et al. [49], which was a randomised controlled trial in which the baseline data was considered for the purpose of the analysis, all of the included studies were cross-sectional. The studies included were published between 2012 and 2022, and they were all in English.
According to age group, 15 studies assessed OHRQoL among childrens [41, 50, 53,54,55, 59,60,61,62, 64, 68, 70, 71, 79, 80], two was in adolescents [38, 56], 12 were in elderly population [42, 44, 45, 47, 57, 63, 65,66,67, 76,77,78] and 12 were in general population [43, 46, 48, 49, 51, 52, 58, 67, 72,73,74,75].
Studies also evaluated the impact of oral conditions over OHRQoL, classified according to exposure to one or more oral conditions, dental caries, gingivitis, periodontal disease, edentulism, malocclusion, dental fluorosis, bruxism and prosthetic need. Studies related to dental caries are (n = 20) [38, 41, 43, 48, 50, 51, 53, 55, 57,58,59,60,61,62, 66, 68, 69, 73, 75, 77], Gingivitis (n = 6) [38, 42, 51, 58, 69, 79], Periodontal Disease assessed by Loss of Attachment (n = 9) [42, 43, 47, 48, 51, 67, 69, 72, 74], Periodontal Disease assessed by Community Periodontal Index (n = 10) [42, 43, 46,47,48, 51, 57, 67, 69, 74], malocclusion (n = 10) [38, 43, 49, 54, 56, 58,59,60, 64, 80], Dental fluorosis (n = 2) [43, 70], Bruxism (n = 2) [52, 71], Functional Edentulism/Edentulism (n = 9) [45, 57, 58, 65, 66, 69, 76,77,78], Prosthetic need (n = 6) [43, 44, 63, 66, 69, 78].
The quality-of-life measurement instruments used in the different studies was as follows; CPQ11-14 [70, 79], ECOHIS [59, 61, 62, 68], OHIP-14 [45, 46, 49, 51, 52, 56, 57, 63, 64, 67, 71,72,73,74,75, 80], OIDP [41, 43, 48, 53, 60], OHIA [38], WHOQoL [76], Michigan Oral Health related quality of life scale [50], FIS [54], Child Oral Health Impact Profile (COHIP) [55] and GOHAI [42, 44, 47, 58, 65, 66, 69, 77, 78], the most frequent being OHIP-14 (n = 16) and GOHAI (n = 9).
Dental caries and OHRQoL
Twenty studies with a total sample of 10,650 individuals assessed the relationship between dental caries and OHRQoL. Eleven studies assessed dental caries with binary outcome and nine studies with continuous measures. Four studies evaluated OHRQoL with GOHAI or OHIP-14, and dental caries was assessed with WHO criteria.
-
a
Dental caries and QoL (Binary outcome)
Individuals with dental caries have nearly four times the chances of having a poor OHRQoL compared to those without dental caries [ OR:3.54 (95% CI 2.24, 5.60), ten studies, 4945 participants], but there was substantial heterogeneity (91%) across the studies (Fig. 3).
-
b
Dental caries and QoL (Continuous data measured by OHIP-14/ ECOHIS/ Michigan Oral Health Quality of Life)
OHRQoL favoured individuals without dental caries when assessed using OHIP-14, ECOHIS, and Michigan Oral Health Quality of Life [SMD: 0.87 (95% CI 0.34, 1.40), six studies, 4511 participants], I2 = 98% (Fig. 4). Babu et al. [59] with 300 individuals was not considered for meta-analysis as one of event in the binary outcome was zero.
-
iii
Dental caries and QoL (GOHAI)
All the three studies [58, 66, 77] were QoL assessed by the GOHAI showed that individuals with decayed teeth is associated with the poor QoL (P < 0.05).
Gingivitis and OHRQoL
Seven studies with 3679 individuals assessed the impact of gingivitis and OHRQoL.
-
a
Gingivitis and QoL (Binary outcome)
Of the 3 studies, only one study reported a significant association of gingivitis on OHRQoL [OR 1.39 (1.09, 1.67)] [69] and other two studies found no significant association [38, 79].
-
b
Gingivitis and QoL (Continuous data measured by GOHAI)
Appukuttan et, al. 2016 [58] found that individuals with gingivitis had poor OHRQoL (P<0.05) and other study reported no significant association (P=0.08) [42].
-
c
Gingivitis and QoL (Continuous data measured by OHIP-14)
Individuals with gingivitis had no impact on OHRQoL when assessed with OHIP-14 (P= 0.0762) [51].
Periodontal Disease assessed by Loss of Attachment (LOA) and OHRQoL
Nine studies with 6289 individuals assessed the relationship between periodontal disease assessed by LOA and OHRQoL.
-
a
Periodontal disease- LOA and QoL (Continuous data measured by OHIP-14/ OIDP)
No difference in OHRQoL between the groups was observed for studies with continuous measures, when OHRQoL assessed with OHIP-14 and OIDP [ SMD: -0.04 (95% CI -2.01, 1.92), four studies, 3414 participants], I2 = 100% (Fig. 5).
-
b
Periodontal disease- LOA and QoL (Binary outcome)
Two studies found there is a significant association between individuals with periodontal disease and OHRQoL [48, 74] and another study by Nagarajappa et al. 2015 denied the association (P=0.687) [43]
-
iii
Periodontal disease- LOA and QoL (Continuous data measured by GOHAI)
One study reported that periodontal diseases had a significant negative impact on OHRQoL [47] and other study by Marya et al. 2020 failed to find a significant association [42].
Periodontal Disease assessed by Community Periodontal Index (CPI) and OHRQoL
Overall, ten studies with 6,300 individuals evaluated the impact between periodontal disease assessed by CPI and OHRQoL. In most studies, OHIP-14 is used to assess the OHRQoL and WHO criteria to measure Periodontal Disease.
-
a
Periodontal disease- CPI and QoL (Continuous data measured by OHIP-14/ OIDP)
There was no difference between two groups when OHRQoL assessed using OHIP- 14 and OIDP scale [ SMD: -0.18 (95% CI -0.53, 0.18), four studies, 3064 participants], I2= 92% (Fig. 6).
-
b
Periodontal disease- CPI and QoL (Binary outcome)
Of the four studies, 3 studies found that individuals with periodontal disease had a negative impact on the OHRQoL [43, 48, 74] and a study by Shivakumar et al. 2018 failed to establish the association [69].
-
iii
Periodontal disease- CPI and QoL (Continuous data measured by GOHAI)
Community Periodontal Index scores showed a negative correlation with OHRQoL [47]. No significant relation was seen between OHRQoL periodontal pocket (P > 0.05) [42].
Functional Edentulism and OHRQoL
Six studies with 1504 individuals assessed the relationship between functional edentulism and OHRQoL.
-
a
Functional edentulism and QoL (Continuous data measured by GOHAI)
No significant association on OHRQoL was found between individual’s with and without functional edentulism when QoL measured by GOHAI [ SMD: 0.31 (95% CI -0.37, 0.99), four studies, 1146 participants], I2= 96% (Fig. 7).
-
b
Functional edentulism and QoL (Binary outcome)
One study found a significant association between functional edentulism [45] and OHRQoL; another study failed to prove the association [69].
Edentulism and OHRQoL
Four studies with 749 individuals evaluated the relationship between edentulism and OHRQoL.
-
a
Edentulism and QoL (Binary outcome)
Edentulism does not have any impact on the OHRQoL [69].
-
b
Edentulism and QoL (Continuous data measured by GOHAI/ WHOQoL)
One study reported that edentulism negatively influenced quality of life [76]. The study by Appukuttan et al. 2016 reported that edentulism did not affect quality of life [58].
-
iii
Edentulism and QoL (Continuous data measured by OHIP-14)
A study by Ajai et al. 2020. There is no significant association on OHRQoL between individuals with and without edentulism on OHRQoL [57].
Malocclusion and OHRQoL
Ten studies with 5687 individuals assesses the impact of malocclusion on OHRQoL.
-
a
Malocclusion and QoL (Binary outcome)
The statistically significant difference was observed between two groups: individuals with malocclusion and without malocclusion [ OR: 5.44 (95% CI 1.61, 18.39), six studies, 3720 participants], I2= 96% (Fig. 8). Babu et al. [59] with 300 individuals was also not considered for meta-analysis as one event in the binary outcome was zero.
-
b
Malocclusion and QoL (Continuous data measured by GOHAI)
There is no significant difference on OHRQoL between individuals with and without malocclusion [58].
-
iii
Malocclusion and QoL (continuous data measured by OHIP-14 / ECOHIS/ FIS)
Malocclusion had a significant negative influence on the OHRQoL [54, 56].
Dental Fluorosis and OHRQoL
Two studies with 3000 individuals assesses the impact of dental fluorosis on OHRQoL.
-
a
Dental fluorosis and QoL (continuous data measured by OIDP/ CPQ 11-14)
There is a significant difference between individuals with and without fluorosis on the OHRQoL [43, 70].
Bruxism and OHRQoL
Two studies with 284 individuals assesses the impact of bruxism on OHRQoL.
-
a
Bruxism and QoL (continuous data measured by OHIP-14)
Bruxers have poor OHRQoL than non-bruxers [52, 71].
Prosthetic need and OHRQoL
Six studies with 3045 individuals assesses the impact of prosthetic need on OHRQoL.
-
a
Prosthetic need and QoL (Binary outcome)
Individuals with prosthetic need is significantly associated with the poor OHRQoL [43, 69].
-
b
Prosthetic need and QoL (continuous data measured by GOHAI)
Of the three studies, only one study found that there is no significant difference between indivduals with prosthetic need and without prosthetic need [78] and other two studies proved the association [44, 66].
-
c
Prosthetic need and QoL (continuous data measured by OHIP-14)
The prosthetic need was significantly related to various components of OHRQOL [63].
Subgroup analysis
-
1.
Dental caries
-
a
Based on the scale (direction of the scores) used to measure OHRQoL (Binary outcome)
-
a
People with dental caries had poor OHRQoL [ OR: 4.73 (95% CI 2.91, 7.68), seven studies, 4114 participants], I2= 90% (Fig. 9).
-
b
Based on the age group for adolescence (10–19 years) (Binary outcome)
Individuals with dental caries had poor OHRQoL [ OR: 3.92 (95% CI 2.06, 7.48), five studies, 3171 participants], I2= 93% (Fig. 10).
-
iii
Based on the age group for children (3–5 years) (Continuous data- measured by ECOHIS, and Michigan Oral Health Quality of Life)
Early childhood caries is significantly associated with the poor OHRQoL [50, 61, 62].
-
2.
Periodontal disease- CPI and QoL (Continuous data measured by OHIP-14 and OIDP)
No significant association between periodontal disease measured by Community Periodontal Index and OHRQoL for the age group between 20 to 79 years [46, 51, 67].
Table 3 Summarizes the description of outcome measurement and oral health conditions with measure of effect.
Discussion
The purpose of this study was to conduct a systematic analysis of the effect of oral conditions on OHRQoL in Indians. To the best of our knowledge, no systematic review with meta-analysis has assessed the impact of oral conditions on quality of life; this is the first. Because of the implications for oral health disparities and access to care, this evidence is required for healthcare decision-making. Given the disparities in the availability, quality, and access to oral health care in India, comparing OHRQoL across groups may help patients, healthcare providers, and policymakers make better decisions [35].
The review demonstrated that the experience of poor OHRQoL is higher among individuals with dental caries, and malocclusion. Pooled evidence confirms that these oral conditions hurt the general state of well-being.
Meta-analysis was performed separately for binary outcome and continuous measures, considering the odds ratio and standard mean difference. OHRQoL assessment scales has different interpretation based on the scores. For example, for GOHAI, COHIP, and WHOQoL, as the score increases, there is an increase on on OHRQoL. Nevertheless, OHIP-14, OIDP, CPQ 11-14, ECOHIS, FIS and Michigan oral health quality of life decreases OHRQoL as the score increases. Hence, for continuous results, scales were divided into two groups based on the direction of the score and a meta-analysis was performed. For binary outcome, all the scales were considered together for meta-analysis irrespective of the direction of the score.
Dental caries and OHRQoL
Dental caries was found to be associated with impaired OHRQoL in the current review. This is consistent with findings of the systematic review by Nora et al. [30] and Zaror et al. [81]. Impact of dental caries on the OHRQoL increases, primarily due to pain and damage to aesthetics, which affect individual social interactions. Moreover, severe dental caries can result in missing school days and having more significant financial expenditures, negatively impacting the OHRQoL of the children's families. Studies included in this systematic review used different caries diagnostic indexes ( dmft/ DMFT, PUFA, WHO criteria), which can interfere with the pooled data summary. Furthermore, there are variations in the criteria to define the severity of dental caries (DMFT > 1, only considered decayed component etc.). This lack of tool standardisation to measure both exposure and outcome can affect the findings.
Gingivitis, periodontal disease, and OHRQoL
We have found that Periodontal diseases had no impact on OHRQoL, which is similar to the findings by Wong et al. [31].
Dose–response effect OHRQoL.
The periodontal disease assessment is based on an ordinal scale, and periodontal disease was considered as present for: score 1(bleeding), score 2; calculus present, score3; shallow pocket, score 4; deep pockets. OHRQoL was affected differently depending on the severity of the disease, with severe periodontitis showing a more pronounced adverse effect than mild to moderate periodontitis. OHRQoL is primarily impacted by the esthetic and functional elements of periodontitis. Compared to periodontitis, gingivitis has a smaller effect on OHRQoL, with its main effects being pain, toothbrushing challenges.
Malocclusion, dental fluorosis, Bruxism and OHRQoL
Our results concluded that there is a significant difference between the two groups concerning malocclusion, affecting quality of life with regard to the appearance of their dentition, self-esteem related to oral health, and interaction with peers. Findings from our study is consistent with the study by Kragt et, al. 2016 [82]. The association of malocclusion and OHRQOL can be due to long-term untreated malocclusions that can result in temporomandibular disorders or trauma. Malocclusion can also results in functional problems like problems with speaking, mastication and subsequent problems restricted food choice [82].
Dental fluorosis rarely causes oral symptoms unless co-morbid disorders such dental caries, enamel fracture, attrition, and dentin hypersensitivity are present, its impact is mainly perceived on a person's assessment of their appearance. Bruxism is associated with the OHRQoL as it can increase the temporomandibular joint load, resulting in signs and symptoms of temporomandibular disorders.
Edentulism, prosthetic need, and OHRQoL
OHRQoL is negatively associated with prosthetic need. Because partially edentulous patients with denture deficiencies face increased cognitive challenges, such as eating, speaking, avoiding smiling, and other psychological and societal consequences, these significant differences in the experience of oral impacts were expected.
Heterogeneity
Heterogeneity was more than 90% since different tools were used to measure both exposure (oral conditions) and outcome (OHRQoL). This review included studies of a wide range of age groups and different populations (within country variation), which might have contributed to clinical heterogeneity. Lack of attention to methodological aspects- such as identification of confounding factors, measurement of exposure, and outcome- may have compromised the studies' validity and methodological heterogeneity.
Implications for research and practice
The tools assessing the OHRQoL need standardisation, more explicitly validated to the local population for being used. This is because the people's perceptions vary for oral conditions among the individuals, thereby attributing heterogeneity. The categorisation of the disease condition does not reflect the pathological process since oral conditions, especially periodontal disease, are chronic and cross-sectional studies cannot establish the temporal relationship.
Strengths and limitations
This review included all the oral conditions and comprehensively assessed both binary outcome and continuous measures. Each study had a distinct methodology, depending on the age group, the criteria used to diagnose oral disorders, the instrument used to measure OHRQoL, and the association measures that were reported in the research. Only few studies were identified for oral conditions such as gingivitis, periodontitis, edentulism, fluorosis, bruxism, and prosthetic need. Classifying oral conditions, especially periodontal disease, is ambiguous and unable to relate to the quality-of-life assessment. Meta- analysis was performed based on the direction of scores of Quality-of-Life instruments, without considering the cut off value, as criteria defining quality of life and score ranges of each scales were different. Another limitation was that, Even though a wide range of oral conditions has been included in the study, dental trauma was not included in the study.
Conclusion
Despite the different definitions of the exposures and variety of instruments used to measure OHRQoL, the review demonstrates that the experience of poor quality of life is substantially higher among individuals with dental caries and malocclusion. Due to the poor methodological quality of the research, the limited sample size, and the variability of the included studies, the evidence was low.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- Child-OIDP:
-
Child Oral Impact on Daily Performances
- COHIP:
-
Child Oral Health Impact Profile
- CPQ11-14:
-
Child Perceptions Questionnaire for children aged 11 to 14 years
- DAI:
-
Dental Aesthetic Index
- DIDL:
-
Dental Impact on Daily Living
- DIP:
-
Dental Impact profile
- DMFT/ dmft:
-
Decayed, Missing, Filled Tooth
- ECOHIS:
-
Early Childhood Oral Health Impact Scale
- FIS:
-
Family Impact Scale
- GOHAI:
-
Geriatric Oral Health Assessment Index
- GRADE Approach:
-
Grading of Recommendations Assessment, Development and Evaluations
- HRQoL:
-
Health Related Quality of Life
- IOTN:
-
Index of Orthodontic Treatment Need
- OHIA:
-
Oral Health Impact in Adolescents
- OHIP-14:
-
Oral Health Impact Profile for 14 years
- OHRQoL:
-
Oral Health-Related Quality of Life
- OIDP:
-
Oral Impacts on Daily Performances
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- PROSPERO:
-
Prospective International Register of Systematic Reviews
- PUFA:
-
Pulpal involvement, Ulceration, Fistula, Abscess;
- QoL:
-
Quality of Life
- SIDD:
-
Social Impact on Dental Disease
- SOHO:
-
Scale of Oral Health Outcomes
- TDI:
-
Traumatic Dental Injuries
- TFI:
-
Thylstrup–Fejerskov Index
- WHO:
-
World Health Organization
- WHOQoL:
-
World Health Organization Quality of Life
References
Oral Health and Quality of Life | FDI. Cited 2022 Jun 23. Available from: https://www.fdiworlddental.org/oral-health-and-quality-life.
Yactayo-Alburquerque MT, Alen-Méndez ML, Azañedo D, Comandé D, Hernández-Vásquez A. Impact of oral diseases on oral health-related quality of life: A systematic review of studies conducted in Latin America and the Caribbean. PLoS ONE. 2021;16(6):e0252578.
Dye BA. The Global Burden of Oral Disease: Research and Public Health Significance. J Dent Res. 2017;96(4):361–3.
Weekly-Bulletin-EW-07–2020.pdf. Cited 2022 May 9. Available from: https://www.moh.gov.jm/wp-content/uploads/2020/03/Weekly-Bulletin-EW-07-2020.pdf.
Janakiram C, Antony B, Joseph J, Ramanarayanan V. Prevalence of Dental Caries in India among the WHO Index Age Groups: A Meta-Analysis. JCDR. 2018. Cited 2022 Jan 16. Available from: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2018&volume=12&issue=8&page=ZE08&issn=0973-709x&id=11956.
Janakiram C, Mehta A, Venkitachalam R. Prevalence of periodontal disease among adults in India: A systematic review and meta-analysis. J Oral Biol Craniofacial Res. 2020;10(4):800–6.
Venkat M, Janakiram C, Ramanarayanan V. Prevalence of tooth mortality among adults in India: A systematic review and meta-analysis. Contemp Clin Dent. 2021;12(4):339.
Balachandran P, Janakiram C. Prevalence of malocclusion among 8–15 years old children, India – A systematic review and meta-analysis. J Oral Biol Craniofac Res. 2021;11(2):192–9.
Borse V, Konwar AN, Buragohain P. Oral cancer diagnosis and perspectives in India. Sensors International. 2020;1:100046.
Alsumait A, ElSalhy M, Raine K, Cor K, Gokiert R, Al-Mutawa S, et al. Impact of dental health on children’s oral health-related quality of life: a cross-sectional study. Health Qual Life Outcomes. 2015;13(1):98.
Tanaka T, Takahashi K, Hirano H, Kikutani T, Watanabe Y, Ohara Y, et al. Oral Frailty as a Risk Factor for Physical Frailty and Mortality in Community-Dwelling Elderly. J Gerontol A. 2018;73(12):1661–7.
Sischo L, Broder HL. Oral Health-related Quality of Life. J Dent Res. 2011;90(11):1264–70.
Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual Life Res. 1993;2(2):153–9.
Cohen LK, Jago JD. Toward the formulation of sociodental indicators. Int J Health Serv. 1976;6(4):681–98.
Oral Health in America: A Report of the Surgeon General. National Institute of Dental and Craniofacial Research; 2000. 338 p.
Locker D, Jokovic A, Tompson B. Health-Related Quality of Life of Children Aged 11 to 14 Years with Orofacial Conditions. Cleft Palate Craniofac J. 2005;42(3):260–6.
Atchison KA, Shetty V, Belin TR, Der-Martirosian C, Leathers R, Black E, et al. Using patient self-report data to evaluate orofacial surgical outcomes. Commun Dent Oral Epidemiol. 2006;34(2):93–102.
Broder HL, Wilson-Genderson M. Reliability and convergent and discriminant validity of the Child Oral Health Impact Profile (COHIP Child?s version). Commun Dent Oral Epidemiol. 2007;35(s1):20–31.
Pahel BT, Rozier RG, Slade GD. Parental perceptions of children’s oral health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual Life Outcomes. 2007;30(5):6.
Gherunpong S, Tsakos G, Sheiham A. Developing and evaluating an oral health-related quality of life index for children; the CHILD-OIDP. Community Dent Health. 2004;21(2):161–9.
Tsakos G, Blair YI, Yusuf H, Wright W, Watt RG, Macpherson LMD. Developing a new self-reported scale of oral health outcomes for 5-year-old children (SOHO-5). Health Qual Life Outcomes. 2012;10(1):62.
Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent. 2004;26(6):512–8.
Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and Reliability of a Questionnaire for Measuring Child Oral-health-related Quality of Life. J Dent Res. 2002;81(7):459–63.
Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25(4):284–90.
Adulyanon S, Vourapukjaru J, Sheiham A. Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol. 1996;24(6):385–9.
Deepan Kumar CV, Mohamed S, Janakiram C, Joseph J. Validation of dental impact on daily living questionnaire among tribal population of India. Contemp Clin Dent. 2015;6(Suppl 1):S235–41.
Atchison KA, Dolan TA. Development of the Geriatric Oral Health Assessment Index. J Dent Educ. 1990;54(11):680–7.
Bettie NF, Ramachandiran H, Anand V, Sathiamurthy A, Sekaran P. Tools for evaluating oral health and quality of life. J Pharm Bioallied Sci. 2015;7(Suppl 2):S414–9.
Christie MJ, French D, Sowden A, West A. Development of child-centered disease-specific questionnaires for living with asthma. Psychosomatic Med. 1993;55(6):541–8.
Nora ÂD, da Silva RC, de Oliveira RR, Soares FZM, Minatel Braga M, Lenzi TL. Is Caries Associated with Negative Impact on Oral Health-Related Quality of Life of Pre-school Children? A Systematic Review and Meta-Analysis. Pediatr Dent. 2018;40(7):403–11.
Wong LB, Yap AU, Allen PF. Periodontal disease and quality of life: Umbrella review of systematic reviews. J Periodontal Res. 2021;56(1):1–17.
Zaror C, Martínez-Zapata MJ, Abarca J, Díaz J, Pardo Y, Pont À, et al. Impact of traumatic dental injuries on quality of life in preschoolers and schoolchildren: A systematic review and meta-analysis. Community Dent Oral Epidemiol. 2018;46(1):88–101.
Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod. 2015;37(3):238–47.
Haag DG, Peres KG, Balasubramanian M, Brennan DS. Oral Conditions and Health-Related Quality of Life: A Systematic Review. J Dent Res. 2017;96(8):864–74.
Inglehart MR, Bagramian RA. Oral health related quality of life: an introduction. Oral health related quality of life Chicago: Quintessence Publishing Co, Inc.; 2002. p. 1–6.
Peres KG, Cascaes AM, Nascimento GG, Victora CG. Effect of breastfeeding on malocclusions: a systematic review and meta-analysis. Acta Paediatr. 2015;104(S467):54–61.
de S Barbosa T, Gavião MBD. Evaluation of the family impact scale for use in Brazil. J Appl Oral Sci. 2009;17(5):397–403.
Baiju RMP, Peter E, Varghese NO, Varughese JM, Sivaram R, Narayan V. Development and initial validation of an oral health-related quality of life scale for older adolescents. Indian J Dent Res. 2019;30(6):826–33.
WHOQOL - Measuring Quality of Life| The World Health Organization. Cited 2022 Jan 16. Available from: https://www.who.int/tools/whoqol.
Nath S, Poirier BF, Ju X, Kapellas K, Haag DG, Ribeiro Santiago PH, et al. Dental Health Inequalities among Indigenous Populations: A Systematic Review and Meta-Analysis. Caries Res. 2021;55(4):268–87.
Kumar S, Kumar A, Badiyani B, Kumar A, Basak D, Ismail MB. Oral health impact, dental caries experience, and associated factors in 12–15-year-old school children in India. Int J Adolesc Med Health. 2015;29(2). Cited 2022 Jun 29. Available from: https://www.degruyter.com/document/doi/https://doi.org/10.1515/ijamh-2015-0041/html.
Marya CM, Grover HS, Tandon S, Taneja P, Gupta A, Marya V. Gender-wise comparison of oral health-related quality of life and its relationship with periodontal status among the Indian elderly. J Indian Soc Periodontol. 2020;24(1):72–9.
Nagarajappa R, Batra M, Sanadhya S, Daryani H, Ramesh G. Relationship between oral clinical conditions and daily performances among young adults in India – A cross sectional study. JEGH. 2015;5(4):347.
Pillai RS, Mathur VP, Jain V, Shah N, Kalra S, Kumar P, et al. Association between dental prosthesis need, nutritional status and quality of life of elderly subjects. Qual Life Res. 2015;24(12):2863–71.
Pushpanjali K, Mohan M, Renuka P. Assessing impact of oral diseases on oral health related quality of life of institutionalized elderly using OHIP-14 in Bengaluru: A cross sectional study. IOSR-JDMS. 2013;6(6):57–64.
Rajagopalachari U, Sonde L, Puranik M. Impact of oral health on quality of life among police personnel in Bengaluru City, India: A cross-sectional survey. J Indian Assoc Public Health Dent. 2015;13(1):42.
Rekhi A, Marya CM, Oberoi SS, Nagpal R, Dhingra C, Kataria S. Periodontal status and oral health-related quality of life in elderly residents of aged care homes in Delhi: Periodontal status and OHRQoL in elderly. Geriatr Gerontol Int. 2016;16(4):474–80.
Saxena A, Nagarajappa R, Ramesh G. Oral Impact on Daily Performance among School Teachers in Kanpur, India: A Cross-sectional Study. JCDR. 2018. Cited 2022 Jun 29. Available from: https://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2018&volume=12&issue=11&page=ZC27&issn=0973-709x&id=12286.
Siluvai S, Kshetrimayum N, Reddy CVK, Siddanna S, Manjunath M, Rudraswamy S. Malocclusion and related quality of life among 13- to 19-year-old students in Mysore City - a cross-sectional study. Oral Health Prev Dent. 2015;13(2):135–41.
Singh N, Dubey N, Rathore M, Pandey P. Impact of early childhood caries on quality of life: Child and parent perspectives. J Oral Biol Craniofacial Res. 2020;10(2):83–6.
Sreela LS, Balan A, Peter E. Association between Oral Health Status and Quality Of Life in Kerala: a population based cross-sectional study. J Adv Med Dent Scie Res. 2020;8(7):8.
Thetakala R, Chandrashekar B, Sunitha S, Maurya M, Sharma P, Shubhi G. Bruxism and oral health-related quality of life among male inmates in a penal institution, Mysore: A cross-sectional study. Indian J Dent Res. 2018;29(3):275.
Usha GV, Thippeswamy H, Nagesh L. Validity and reliability of Oral Impacts on Daily Performances Frequency Scale: a cross-sectional survey among adolescents. J Clin Pediatr Dent. 2012;36(3):251–6.
Vinayagamoorthy K, Pentapati KC, Urala A, Acharya S. Validation of an Indian (Kannada) translation of the Family Impact Scale questionnaire and the impact of malocclusion on the families of adolescent school children. Int Dent J. 2020;70(4):259–65.
Kumar VS, Karuveettil V, Joseph J, Yeturu SK, Suseela RP, Janakiram C. Association of Dental Caries and Oral Health Impact Profile in 12-Year-Old School Children: A Cross-Sectional Study. JCDR. 2018. Cited 2022 Aug 29. Available from: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2018&volume=12&issue=9&page=ZC12&issn=0973-709x&id=11984.
Mary AV, Mahendra J, John J, Moses J, Ebenezar AVR, Kesavan R. Oral Health Practices, Status and Effect of Malocclusion on Quality of Life of College Going Individuals in Chennai, India. JCDR. 2019. Cited 2022 Aug 29. Available from: https://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2019&volume=13&issue=1&page=ZC05&issn=0973-709x&id=12432.
Saxena A, Nagarajappa R, Naik D, Abid M, Ramesh G. Assessing the effect of oral diseases on oral health related quality of life of institutionalized elderly using Oral Health Impact Profile (OHIP-14) questionnaire: a pilot study. Rocz Panstw Zakl Hig. 2020;71(3):349-353. https://doi.org/10.32394/rpzh.2020.0130.
Appukuttan DP, Tadepalli A, Victor DJ, Dharuman S. Oral Health Related Quality of Life among Tamil Speaking Adults Attending a Dental Institution in Chennai, Southern India. JCDR. 2016. Cited 2022 Jun 25. Available from: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2016&volume=10&issue=10&page=ZC114&issn=0973-709x&id=8693.
Babu NSV, Moureen AA, Bhanushali PV. Comparative Evaluation of Impact of Dental Caries, Malocclusion and Developmental Defects on Preschooler’s Quality of. Life. 2017;4(11):5.
Basavaraj P, Sunil MK, Nagarajappa R, Ashish S, Ramesh G. Correlation Between Oral Health and Child-OIDP Index in 12- and 15-Year-Old Children From Modinagar. India Asia Pac J Public Health. 2014;26(4):390–400.
Ghanghas M, Manjunath BC, Kumar A, Shyam R, Phogat R, Panghal V. Validation of the Hindi version of the early childhood oral health impact scale among 3–5-year-old preschool children in Rohtak city, Haryana. J Indian Soc Pedod Prev Dent. 2019;37(4):333–8.
Jaggi A, Marya CM, Nagpal R, Oberoi SS, Kataria S, Taneja P. Impact of Early Childhood Caries on Oral Health-related Quality of Life Among 4–6-year-old Children Attending Delhi Schools: A Cross-sectional Study. Int J Clin Pediatr Dent. 2019;12(3):215–21.
Joseph AG, Janakiram C, Mathew A. Prosthetic Status, Needs and Oral Health Related Quality of Life (OHRQOL) in the Elderly Population of Aluva, India. JCDR. 2016 Cited 2022 Jun 29. Available from: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2016&volume=10&issue=11&page=ZC05&issn=0973-709x&id=8768.
Manjith C, Karnam SK, Manglam S, Praveen M, Mathur A. Oral Health-Related Quality of Life (OHQoL) among Adolescents Seeking Orthodontic Treatment. J Contemp Dent Pract. 2012;13(3):294–8.
Neelamana S, Janakiram C, Varma B. Oral health status and related quality of life among elderly tribes in India. J Family Med Prim Care. 2020;9(12):5976–81.
Rekhi A, Marya CM, Nagpal R, Oberoi SS. Assessment of Oral Health Related Quality of Life Among the Institutionalised Elderly in Delhi. India Oral Health Prevent Dent. 2018;16(1):59–66.
Sanadhya S, Dobaria N, Aapaliya P, Choudhary G, Jain S, Sharma N. Assessment and comparison of clinical dental status and its impact on oral health-related quality of life among rural and urban adults of Udaipur, India: A cross-sectional study. J Basic Clin Pharma. 2015;6(2):50.
Sharna N, Ramakrishnan M, Samuel V, Ravikumar D, Cheenglembi K, Anil S. Association between Early Childhood Caries and Quality of Life: Early Childhood Oral Health Impact Scale and Pufa Index. Dent J. 2019;7(4):95.
Shivakumar K, Patil S, Kadashetti V, Raje V. Oral health-related quality of life of institutionalized elderly in Satara District, India. J Datta Meghe Inst Med Sci Univ. 2018;13(4):183–9.
Shyam R, Bhadravathi Chaluvaiah M, Kumar A, Pahwa M, Rani G, Phogat R. Impact of dental fluorosis on the oral health related quality of life among 11- to 14-year-old school children in endemic fluoride areas of Haryana (India). Int Dent J. 2020;70(5):340–6.
Suguna S, Gurunathan D. Quality of life of children with sleep bruxism. J Family Med Prim Care. 2020;9(1):332.
Yadav T, Chopra P, Kapoor S. Association between chronic periodontitis and oral health–related quality of life in Indian adults. J Int Oral Health. 2019;11(5):280.
Abhishek KN, Shamarao S, Jain J, Haridas R, Ajagannanavar SL, Khanapure SC. Impact of caries prevalence on oral health-related quality of life among police personnel in Virajpet, South India. J Int Soc Prev Community Dent. 2014;4(3):188–92.
Abhishek KN, Jain J, Shamarao S, Khanapure SC. Impact of periodontal status on oral health-related quality of life among police personnel in Virajpet. India J Invest Clin Dent. 2016;7(2):193–7.
Jain M, Kaira LS, Sikka G, Singh S, Gupta A, Sharma R, Sawla L, Mathur A. How do age and tooth loss affect oral health impacts and quality of life? A study comparing two state samples of gujarat and rajasthan. J Dent (Tehran). 2012;9(2):135–44.
Marina M, Ariga P, Ganapathy DM, Mallikarjuna AV. The impact of edentulism on quality of life among South Indian geriatric patients. Drug Invention Today. 2019;11(3):3.
Rekhi A, Mehra A, Gomes A, Bisht S, Chahal G, Dadwal H. Dentition Status and its effect on the Oral Health Related Quality of Life in a Rural Elderly Population: A Cross Sectional Study. Epidem Int. 2015;1(1):12–5.
Shetty VD, Bijle MNA, Patilshankargouda. The Relationship between prosthetic status and the Geriatric Oral Health Assessment Index in a Group of Institutionalized elderly of an Indian City: A cross-sectional study. J Contemp Dent Pract. 2013;14(6):1173–7.
Singh O, Reddy V, Sharma L, Pradhan D, Srivastava R. Association of gingivitis with children oral health-related quality of life in Lucknow: A cross-sectional study. J Family Med Prim Care. 2020;9(2):1177.
Singh T, Bhagia P, Gupta U, Passi D, Goyal J, Yadav G, et al. Effect of orthodontic treatment needs on oral health related quality of life among the young population in Delhi NCR-region of North India. J Family Med Prim Care. 2019;8(2):550.
Zaror C, Matamala-Santander A, Ferrer M, Rivera-Mendoza F, Espinoza-Espinoza G, Martínez-Zapata MJ. Impact of early childhood caries on oral health-related quality of life: A systematic review and meta-analysis. Int J Dent Hyg. 2022;20(1):120–35.
Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM. The impact of malocclusions on oral health-related quality of life in children—a systematic review and meta-analysis. Clin Oral Investig. 2016;20(8):1881–94.
Acknowledgements
Not applicable
Funding
None.
Author information
Authors and Affiliations
Contributions
“All authors contributed to the study conception, design, Interpretatation of the results and reviewing. Data extraction and Data analysis were performed by A.J. [Anju James], C.J. [Chandrashekar Janakiram] and R.V. M [R.V. Meghana]. The quality assessment were performed by the C.J. [Chandrashekar Janakiram], S.V.K. [S. Vijay Kumar] and A.R.S. [Anitha R Sagarkar]. The first draft of the manuscript was written by A.J. [Anju James] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.”
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: S1.
Search strategy.
Additional file 2: Appendix II.
Studies ineligible following full- text review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
James, A., Janakiram, C., Meghana, R.V. et al. Impact of oral conditions on oral health-related quality of life among Indians- a systematic review and Meta-analysis. Health Qual Life Outcomes 21, 102 (2023). https://doi.org/10.1186/s12955-023-02170-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-023-02170-6