Abstract
Objective
To evaluate the prevalence of signs and symptoms related to temporomandibular disorders (TMD) and orofacial pain in patients with indication for orthognathic surgery.
Methods
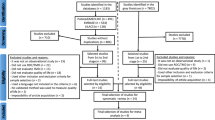
The search was carried out in seven electronic databases and gray literature. Studies that evaluated the frequency of signs and symptoms related to TMD and orofacial pain were included. The risk of bias was assessed using the Joanna Briggs Critical Appraisal tool. A meta-analysis of proportions with a random effect model was performed and the GRADE tool judged the certainty of evidence.
Results
After searching the databases, 1859 references were retrieved, 18 of which were selected for synthesis. The prevalence of individuals with at least one TMD symptom was 51% [CI95% = 44–58%], and 44% of the subjects had temporomandibular joint click/crepitus [CI95% = 37–52%]. Additionally, 28% exhibited symptoms related to muscle disorders [CI95% = 22–35%], 34% had disc displacement with or without reduction [CI95% = 25–44%], and 24% had inflammatory joint disorders [CI95% = 13–36%]. The prevalence of headache was 26% [CI95% = 8–51%]. The certainty of evidence was considered very low.
Conclusion
Approximately 1 in 2 patients with dentofacial deformity presents some sign and symptom related to TMD. Myofascial pain and headache may be present in approximately a quarter of patients with dentofacial deformity.
Clinical relevance
A multidisciplinary treatment is necessary for these patients, involving a professional with expertise in the management of TMD.







Similar content being viewed by others
Data availability
The datasets used and/or analyses during the current study are available from the corresponding author on reasonable request.
References
Al-Moraissi EA, Perez D, Ellis E 3rd (2017) Do patients with malocclusion have a higher prevalence of temporomandibular disorders than controls both before and after orthognathic surgery? A systematic review and meta-analysis. J Cranio-Maxillo-Facial Surg Off Publ Eur Assoc Cranio-Maxillo-Facial Surg 45:1716–1723. https://doi.org/10.1016/j.jcms.2017.07.015
AlWarawreh AM, AlTamimi ZH, Khraisat HM, Kretschmer W (2018) Prevalence of temporomandibular disorder symptoms among orthognathic patients in Southern Germany: retrospective study. Int J Dent 2018:. https://doi.org/10.1155/2018/4706487
Valesan LF, Da-Cas CD, Réus JC et al (2021) Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Investig 25:441–453. https://doi.org/10.1007/s00784-020-03710-w
Abrahamsson C, Henrikson T, Nilner M et al (2013) TMD before and after correction of dentofacial deformities by orthodontic and orthognathic treatment. Int J Oral Maxillofac Surg 42:752–758. https://doi.org/10.1016/j.ijom.2012.10.016
Sebastiani AM, Gerber JT, Bergamaschi IP et al (2021) Individuals requiring orthognathic surgery have more depression and pain than controls. Braz Oral Res 35:e091. https://doi.org/10.1590/1807-3107bor-2021.vol35.0091
De Araujo CM, Schroder AGD, De Araujo BMDM et al (2020) Impact of orthodontic-surgical treatment on quality of life: a meta-analysis. Eur J Orthod 42:281–289. https://doi.org/10.1093/ejo/cjz093
Bergamaschi IP, Cavalcante RC, Fanderuff M et al (2021) Orthognathic surgery in class II patients: a longitudinal study on quality of life, TMD, and psychological aspects. Clin Oral Investig 25:3801–3808. https://doi.org/10.1007/s00784-020-03709-3
Basso IB, Gonçalves FM, Martins AA et al (2022) Psychosocial changes in patients submitted to orthodontic surgery treatment: a systematic review and meta-analysis. Clin Oral Investig 26:2237–2251. https://doi.org/10.1007/s00784-021-04304-w
Page MJ, McKenzie JE, Bossuyt PM, et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:. https://doi.org/10.1136/bmj.n71
The Joanna Briggs Institute (2014) Joanna Briggs Institute Reviewers’ Manual
Guyatt GH, Oxman AD, Vist GE et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926. https://doi.org/10.1136/bmj.39489.470347.AD
Abrahamsson C, Henrikson T, Bondemark L, Ekberg EC (2015) Masticatory function in patients with dentofacial deformities before and after orthognathic treatment - a prospective, longitudinal, and controlled study. Eur J Orthod 37:67–72. https://doi.org/10.1093/ejo/cju011
Chung K, Richards T, Nicot R et al (2017) ENPP1 and ESR1 genotypes associated with subclassifications of craniofacial asymmetry and severity of temporomandibular disorders. Am J Orthod Dentofac Orthop 152:631–645. https://doi.org/10.1016/j.ajodo.2017.03.024
Farella M, Michelotti A, Bocchino T et al (2007) Effects of orthognathic surgery for class III malocclusion on signs and symptoms of temporomandibular disorders and on pressure pain thresholds of the jaw muscles. Int J Oral Maxillofac Surg 36:583–587. https://doi.org/10.1016/j.ijom.2007.02.001
Luo Y, Svensson P, Jensen JD et al (2014) Quantitative sensory testing in patients with or without ongoing pain one year after orthognathic surgery. J Oral Facial Pain Headache 28:306–316. https://doi.org/10.11607/ofph.1275
Mladenović I, Dodić S, Stošić S et al (2014) TMD in class III patients referred for orthognathic surgery: Psychological and dentition-related aspects. J Cranio-Maxillofacial Surg 42:1604–1609. https://doi.org/10.1016/j.jcms.2014.04.029
de Oliveira Freitas Passos DCB, Conti PCR, Filho HN, Berretin-Felix G (2015) The occurrence of temporomandibular disorders in subjects presented with dentofacial deformities/ Ocorrencia de disfuncao temporomandibular em individuos com deformidade dentofacial. Rev CEFAC Atualizacao Cient em Fonoaudiol e Educ 17:1215+
Sebastiani AM, Baratto-Filho F, Bonotto D et al (2016) Influence of orthognathic surgery for symptoms of temporomandibular dysfunction. Oral Surg Oral Med Oral Pathol Oral Radiol 121:119–125. https://doi.org/10.1016/j.oooo.2015.08.012
Sebastiani AM, de Lucas Corso PFC, Bonotto D et al (2018) Does orthognathic surgery improve myofacial pain in individuals with skeletal class III? One-year follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol 126:322–330. https://doi.org/10.1016/j.oooo.2018.03.020
Sebastiani AM, Dos Santos KM, Cavalcante RC et al (2020) Depression, temporomandibular disorders, and genetic polymorphisms in IL6 impact on oral health-related quality of life in patients requiring orthognathic surgery. Qual Life Res Int J Qual life Asp Treat Care Rehabil 29:3315–3323. https://doi.org/10.1007/s11136-020-02581-8
Roland-Billecart T, Raoul G, Kyheng M et al (2021) TMJ related short-term outcomes comparing two different osteosynthesis techniques for bilateral sagittal split osteotomy. J Stomatol Oral Maxillofac Surg 122:70–76. https://doi.org/10.1016/j.jormas.2020.03.018
Abrahamsson C, Ekberg E, Henrikson T et al (2009) TMD in consecutive patients referred for orthognathic surgery. Angle Orthod 79:621–627. https://doi.org/10.2319/060408-293.1
Di Paolo C, Pompa G, Arangio P et al (2017) Evaluation of temporomandibular disorders before and after orthognathic surgery: therapeutic considerations on a sample of 76 patients. J Int Soc Prev Community Dent 7:125–129. https://doi.org/10.4103/jispcd.JISPCD_443_16
Sahu GR, Kaur A, Rattan V et al (2022) Effect of orthognathic surgery on temporomandibular disorders: a prospective study. J Maxillofac Oral Surg 21:277–282. https://doi.org/10.1007/s12663-021-01644-8
Takahara N, Kabasawa Y, Sato M et al (2017) MRI changes in the temporomandibular joint following mandibular setback surgery using sagittal split ramus osteotomy with rigid fixation. Cranio - J Craniomandib Pract 35:38–45. https://doi.org/10.1080/08869634.2016.1143167
Toh AQJ, Leung YY (2022) The effect of orthognathic surgery on temporomandibular disorder. J Cranio-Maxillofacial Surg 50:218–224. https://doi.org/10.1016/j.jcms.2021.11.012
Jaramillo SP, Del Valle AF (2004) Signos y síntomas de desórdenes temporomandibulares antes y después de cirugía ortognática, comparación entre osteotomía sagital y osteotomía oblicua de rama. Rev Fac Odontol Univ Antioq 16(1):42–51
Catherine Z, Courvoisier DS, Scolozzi P (2016) Are condylar morphologic changes associated with temporomandibular disorders in patients with orthognathia? Oral Surg Oral Med Oral Pathol Oral Radiol 122:e44–e50. https://doi.org/10.1016/j.oooo.2016.03.006
Ho AMH, Phelan R, Mizubuti GB et al (2018) Bias in before-after studies: narrative overview for anesthesiologists. Anesth Analg 126:1755–1762. https://doi.org/10.1213/ANE.0000000000002705
Graff-Radford SB, Bassiur JP (2014) Temporomandibular disorders and headaches. Neurol Clin 32:525–537. https://doi.org/10.1016/j.ncl.2013.11.009
Author information
Authors and Affiliations
Contributions
M.R.G., R.D.S., A.X.F., carried out the article selection process, risk of bias analysis, and critical reading of the writing. F.M.G and W.V.N, carried out the construction of figures and tables, and critical reading of the writing. R.S.S., B.L.C.L., A.G.D.S., B.S.Z. performed the writing of the manuscript. C.M.A. coordinated the research, carried out the statistical analyzes and critical reading of the writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garcia, M.R., da Silva, R.D., Ferraz, A.X. et al. Prevalence of signs and symptoms related to temporomandibular disorders and orofacial pain in patients indicated for orthognathic surgery: a meta-analysis. Clin Oral Invest 27, 3307–3319 (2023). https://doi.org/10.1007/s00784-023-05110-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05110-2