Abstract
Objectives
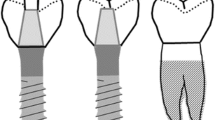
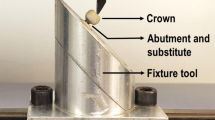
The aim of this study was to investigate the in vitro fatigue and fracture force of temporary implant-supported anterior crowns made of different materials with different abutment total occlusal convergence (TOC), with/without a screw channel, and with different types of fabrication.
Materials and methods
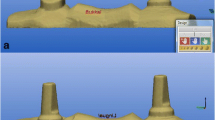
One hundred ninety-two implant-supported crowns were manufactured (4° or 8° TOC; with/without screw channel) form 6 materials (n = 8; 2 × additive, 3 × subtractive, 1 × automix; reference). Crowns were temporarily cemented, screw channels were closed (polytetrafluoroethylene, resin composite), and crowns were stored in water (37 °C; 10 days) before thermal cycling and mechanical loading (TCML). Fracture force was determined. Statistics: Kolmogorov–Smirnov, ANOVA; Bonferroni; Kaplan–Meier; log-rank; α = 0.05.
Results
Failure during TCML varied between 0 failures and total failure. Mean survival was between 1.8 × 105 and 4.8 × 105 cycles. The highest impact on survival presented the material (η2 = 0.072, p < .001). Fracture forces varied between 265.7 and 628.6 N. The highest impact on force was found for the material (η2 = 0.084, p < .001).
Conclusion
Additively and subtractively manufactured crowns provided similar or higher survival rates and fracture forces compared to automix crowns. The choice of material is decisive for the survival and fracture force. The fabrication is not crucial. A smaller TOC led to higher fracture force. Manually inserted screw channels had negative effects on fatigue testing.
Clinical relevance
The highest stability has been shown for crowns with a low TOC, which are manufactured additively and subtractively. In automix-fabricated crowns, manually inserted screw channels have negative effects.




Similar content being viewed by others
References
Albrektsson T, Donos N (2012) Implant survival and complications. The third EAO consensus conference 2012. Clin Oral Implants Res 23(Suppl 6):63–65. https://doi.org/10.1111/j.1600-0501.2012.02557.x
Pjetursson BE, Heimisdottir K (2018) Dental implants - are they better than natural teeth? Eur J Oral Sci 126(Suppl 1):81–87. https://doi.org/10.1111/eos.12543
Burns DR, Beck DA, Nelson SK (2003) A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the committee on research in fixed prosthodontics of the academy of fixed prosthodontics. J Prosthet Dent 90:474–497. https://doi.org/10.1016/s0022-3913(03)00259-2
Perry RD, Magnuson B (2012) Provisional materials: key components of interim fixed restorations. Compend Contin Educ Dent 33(59–60):62
González-Martín O, Lee E, Weisgold A et al. (2020) Contour management of implant restorations for optimal emergence profiles: guidelines for immediate and delayed provisional restorations. Int J Periodontics Restorative Dent 40:61–70. https://doi.org/10.11607/prd.4422
Kerby RE, Knobloch LA, Sharples S et al (2013) Mechanical properties of urethane and bis-acryl interim resin materials. J Prosthet Dent 110:21–28. https://doi.org/10.1016/S0022-3913(13)60334-0
Bauer R, Zacher J, Strasser T et al (2023) Dependence of the survival of 3D-printed temporary materials on the filler content. Int J Comput Dent 0:1–14. https://doi.org/10.3290/j.ijcd.b3759607
John P, Muthukumar B, Kumar MV (2015) Comparison of the effect of dentin bonding, dentin sealing agents on the microleakage of provisional crowns fabricated with direct and indirect technique-an invitro study. J Clin Diagn Res 9:ZC54–7. https://doi.org/10.7860/JCDR/2015/13534.6122
Hahnel S, Krifka S, Behr M et al (2019) Performance of resin materials for temporary fixed denture prostheses. J Oral Sci 61:270–275. https://doi.org/10.2334/josnusd.18-0150
Luthardt RG, Stössel M, Hinz M et al (2000) Clinical performance and periodontal outcome of temporary crowns and fixed partial dentures: a randomized clinical trial. J Prosthet Dent 83:32–39. https://doi.org/10.1016/s0022-3913(00)70086-2
Piplani A, Suresh Sajjan MC, Ramaraju AV et al (2016) An in-vitro study to compare the temperature rise in the pulp chamber by direct method using three different provisional restorative materials. J Indian Prosthodont Soc 16:36–41. https://doi.org/10.4103/0972-4052.161569
Kim S, Watts D (2004) Polymerization shrinkage-strain kinetics of temporary crown and bridge materials. Dent Mater 20:88–95. https://doi.org/10.1016/S0109-5641(03)00101-5
Balkenhol M, Knapp M, Ferger P et al (2008) Correlation between polymerization shrinkage and marginal fit of temporary crowns. Dent Mater 24:1575–1584. https://doi.org/10.1016/j.dental.2008.07.001
Alt V, Hannig M, Wöstmann B et al (2011) Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent Mater 27:339–347. https://doi.org/10.1016/j.dental.2010.11.012
Peng C-C, Chung K-H, Yau H-T et al (2020) Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J Prosthet Dent 123:514–522. https://doi.org/10.1016/j.prosdent.2019.02.024
Tahayeri A, Morgan M, Fugolin AP et al (2018) 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater 34:192–200. https://doi.org/10.1016/j.dental.2017.10.003
Zimmermann M, Ender A, Egli G et al (2018) Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin Oral Investig 23:2777–2784. https://doi.org/10.1007/s00784-018-2717-2
Lee W-S, Lee D-H, Lee K-B (2017) Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J Adv Prosthodont 9:265–270. https://doi.org/10.4047/jap.2017.9.4.265
Kurbad A (2013) CAD/CAM-based polymer provisionals as treatment adjuncts. Int J Comput Dent 16:327–346
Schnutenhaus S, Neveling U, Luthardt RG (2018) Digital implantological workflow for a CAD/CAM immediate long-term temporary restoration for the edentulous maxilla. Int J Comput Dent 21:133–146
Abdullah AO, Pollington S, Liu Y (2018) Comparison between direct chairside and digitally fabricated temporary crowns. Dent Mater J 37:957–963. https://doi.org/10.4012/dmj.2017-315
Kessler A, Reymus M, Hickel R et al (2019) Three-body wear of 3D printed temporary materials. Dent Mater 35:1805–1812. https://doi.org/10.1016/j.dental.2019.10.005
Revilla-León M, Meyers MJ, Zandinejad A et al (2019) A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J Esthet Restor Dent 31:51–57. https://doi.org/10.1111/jerd.12438
Abdullah AO, Tsitrou EA, Pollington S (2016) Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns. J Appl Oral Sci 24:258–263. https://doi.org/10.1590/1678-775720150451
Berli C, Thieringer FM, Sharma N et al (2020) Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices. J Prosthet Dent 124:780–786. https://doi.org/10.1016/j.prosdent.2019.10.024
Rosentritt M, Raab P, Hahnel S et al (2017) In-vitro performance of CAD/CAM-fabricated implant-supported temporary crowns. Clin Oral Investig 21:2581–2587. https://doi.org/10.1007/s00784-017-2057-7
Rosentritt M, Hahnel S, Engelhardt F et al (2017) In vitro performance and fracture resistance of CAD/CAM-fabricated implant supported molar crowns. Clin Oral Investig 21:1213–1219. https://doi.org/10.1007/s00784-016-1898-9
Rosentritt M, Behr M, van der Zel JM et al (2009) Approach for valuating the influence of laboratory simulation. Dent Mater 25:348–352. https://doi.org/10.1016/j.dental.2008.08.009
Rosentritt M, Siavikis G, Behr M et al (2008) Approach for valuating the significance of laboratory simulation. J Dent 36:1048–1053. https://doi.org/10.1016/j.jdent.2008.09.001
Huettig F, Prutscher A, Goldammer C et al (2016) First clinical experiences with CAD/CAM-fabricated PMMA-based fixed dental prostheses as long-term temporaries. Clin Oral Investig 20:161–168. https://doi.org/10.1007/s00784-015-1475-7
Sari T, Usumez A, Strasser T et al (2020) Temporary materials: comparison of in vivo and in vitro performance. Clin Oral Investig 24:4061–4068. https://doi.org/10.1007/s00784-020-03278-5
Zacher J, Bauer R, Strasser T et al (2020) Laboratory performance and fracture resistance of CAD/CAM implant-supported tooth-coloured anterior FDPs. J Dent 96:103326. https://doi.org/10.1016/j.jdent.2020.103326
Alifui-Segbaya F, Bowman J, White AR et al (2019) Characterization of the double bond conversion of acrylic resins for 3D printing of dental prostheses. Compend Contin Educ Dent 40:e7–e11
Loflin WA, English JD, Borders C et al (2019) Effect of print layer height on the assessment of 3D-printed models. Am J Orthod Dentofacial Orthop 156:283–289. https://doi.org/10.1016/j.ajodo.2019.02.013
Alam M, Chugh A, Kumar A et al (2022) Comparative evaluation of fracture resistance of anterior provisional restorations fabricated using conventional and digital techniques - An in vitro study. J Indian Prosthodont Soc 22:361–367. https://doi.org/10.4103/jips.jips_547_21
Yao J, Li J, Wang Y et al (2014) Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J Prosthet Dent 112:649–657. https://doi.org/10.1016/j.prosdent.2014.01.012
Silva GC, Cornacchia TM, de Magalhães CS et al (2014) Biomechanical evaluation of screw- and cement-retained implant-supported prostheses: a nonlinear finite element analysis. J Prosthet Dent 112:1479–1488. https://doi.org/10.1016/j.prosdent.2014.06.010
Wittneben J-G, Millen C, Brägger U (2014) Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions-a systematic review. Int J Oral Maxillofac Implants 29 Suppl:84–98. https://doi.org/10.11607/jomi.2014suppl.g2.1
Torrado E, Ercoli C, Al Mardini M et al (2004) A comparison of the porcelain fracture resistance of screw-retained and cement-retained implant-supported metal-ceramic crowns. J Prosthet Dent 91:532–537. https://doi.org/10.1016/j.prosdent.2004.03.014
Edmonds HM, Glowacka H (2020) The ontogeny of maximum bite force in humans. J Anat 237:529–542. https://doi.org/10.1111/joa.13218
Trulsson M, Gunne HS (1998) Food-holding and -biting behavior in human subjects lacking periodontal receptors. J Dent Res 77:574–582. https://doi.org/10.1177/00220345980770041001
Acknowledgements
The authors would like to thank individual manufacturers for providing material. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Laila Bein made Conceptualization, Writing, Investigation, Data Evaluation, Visualization, Michael Schmidt and Angelika Rauch editied and Martin Rosentritr made: Conceptualization, Supervision, Writing – Review & Editing.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
Laila Bein declares that she has no conflict of interest.
Dr. Angelika Rauch declares that he has no conflict of interest.
Dr. Michael Schmidt declares that she has no conflict of interest.
Prof. Dr. Martin Rosentritt declares that he has third-party research projects with different dental companies.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bein, L., Rauch, A., Schmidt, M. et al. In vitro fatigue and fracture testing of temporary materials from different manufacturing processes in implant-supported anterior crowns. Clin Oral Invest 27, 4215–4224 (2023). https://doi.org/10.1007/s00784-023-05038-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05038-7