Abstract
Objectives
The aim of this review was to investigate the application of artificial intelligence (AI) in maxillofacial computer-assisted surgical planning (CASP) workflows with the discussion of limitations and possible future directions.
Materials and methods
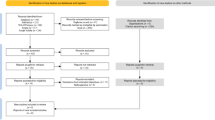
An in-depth search of the literature was undertaken to review articles concerned with the application of AI for segmentation, multimodal image registration, virtual surgical planning (VSP), and three-dimensional (3D) printing steps of the maxillofacial CASP workflows.
Results
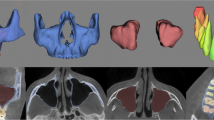
The existing AI models were trained to address individual steps of CASP, and no single intelligent workflow was found encompassing all steps of the planning process. Segmentation of dentomaxillofacial tissue from computed tomography (CT)/cone-beam CT imaging was the most commonly explored area which could be applicable in a clinical setting. Nevertheless, a lack of generalizability was the main issue, as the majority of models were trained with the data derived from a single device and imaging protocol which might not offer similar performance when considering other devices. In relation to registration, VSP and 3D printing, the presence of inadequate heterogeneous data limits the automatization of these tasks.
Conclusion
The synergy between AI and CASP workflows has the potential to improve the planning precision and efficacy. However, there is a need for future studies with big data before the emergent technology finds application in a real clinical setting.
Clinical relevance
The implementation of AI models in maxillofacial CASP workflows could minimize a surgeon’s workload and increase efficiency and consistency of the planning process, meanwhile enhancing the patient-specific predictability.

Similar content being viewed by others
References
Mesko B (2017) The role of artificial intelligence in precision medicine. Expert Rev Precis Med Drug Dev 2:239–241. https://doi.org/10.1080/23808993.2017.1380516
Hopp WJ, Li J, Wang G (2018) Big data and the precision medicine revolution. Prod Oper Manag 27:1647–1664. https://doi.org/10.1111/poms.12891
Kim YJ, Kelley BP, Nasser JS, Chung KC (2019) Implementing precision medicine and artificial intelligence in plastic surgery: concepts and future prospects. Plast Reconstr Surg - Glob Open 7:e2113. https://doi.org/10.1097/GOX.0000000000002113
Joskowicz L (2017) Computer-aided surgery meets predictive, preventive, and personalized medicine. EPMA J 8:1–4. https://doi.org/10.1007/s13167-017-0084-8
Ahmed Z, Mohamed K, Zeeshan S, Dong XQ (2020) Artificial intelligence with multi-functional machine learning platform development for better healthcare and precision medicine. Database (Oxford) 2020: 1–35. https://doi.org/10.1093/database/baaa010
Sharaf B, Levine JP, Hirsch DL et al (2010) Importance of computer-aided design and manufacturing technology in the multidisciplinary approach to head and neck reconstruction. J Craniofac Surg 21:1277–1280. https://doi.org/10.1097/SCS.0b013e3181e1b5d8
Fu X, Qiao J, Girod S et al (2017) Standardized protocol for virtual surgical plan and 3-dimensional surgical template-assisted single-stage mandible contour surgery. Ann Plast Surg 79:236–242. https://doi.org/10.1097/SAP.0000000000001149
Efanov JI, Roy AA, Huang KN, Borsuk DE (2018) Virtual surgical planning: the pearls and pitfalls. Plast Reconstr Surg - Glob Open 6:e1443. https://doi.org/10.1097/GOX.0000000000001443
Stranix JT, Stern CS, Rensberger M et al (2019) A virtual surgical planning algorithm for delayed maxillomandibular reconstruction. Plast Reconstr Surg 143:1197–1206. https://doi.org/10.1097/PRS.0000000000005452
Flügge T, Ludwig U, Hövener JB et al (2020) Virtual implant planning and fully guided implant surgery using magnetic resonance imaging—proof of principle. Clin Oral Implants Res 31:575–583. https://doi.org/10.1111/clr.13592
Donaldson CD, Manisali M, Naini FB (2021) Three-dimensional virtual surgical planning (3D-VSP) in orthognathic surgery: advantages, disadvantages and pitfalls. J Orthod 48:52–63. https://doi.org/10.1177/1465312520954871
Steinbacher DM (2015) Three-dimensional analysis and surgical planning in craniomaxillofacial surgery. J Oral Maxillofac Surg 73:S40–S56. https://doi.org/10.1016/j.joms.2015.04.038
Pfaff MJ, Steinbacher DM (2016) Plastic surgery applications using three-dimensional planning and computer-assisted design and manufacturing. Plast Reconstr Surg 137:603e–616e. https://doi.org/10.1097/01.prs.0000479970.22181.53
Steinhuber T, Brunold S, Gärtner C et al (2018) Is virtual surgical planning in orthognathic surgery faster than conventional planning? A time and workflow analysis of an office-based workflow for single- and double-jaw surgery. J Oral Maxillofac Surg 76:397–407. https://doi.org/10.1016/j.joms.2017.07.162
Yuan P, Mai H, Li J et al (2017) Design, development and clinical validation of computer-aided surgical simulation system for streamlined orthognathic surgical planning. Int J Comput Assist Radiol Surg 12:2129–2143. https://doi.org/10.1007/s11548-017-1585-6
Knoops PGM, Papaioannou A, Borghi A et al (2019) A machine learning framework for automated diagnosis and computer-assisted planning in plastic and reconstructive surgery. Sci Rep 9:1–12. https://doi.org/10.1038/s41598-019-49506-1
Murphy DC, Saleh DB (2020) Artificial Intelligence in plastic surgery: What is it? Where are we now? What is on the horizon? Ann R Coll Surg Engl 102:577–580. https://doi.org/10.1308/RCSANN.2020.0158
Hung K, Montalvao C, Tanaka R et al (2019) The use and performance of artificial intelligence applications in dental and maxillofacial radiology: a systematic review. Dentomaxillofacial Radiol 49:20190107. https://doi.org/10.1259/dmfr.20190107
Khanagar SB, Naik S, Al Kheraif AA et al (2021) Application and performance of artificial intelligence technology in oral cancer diagnosis and prediction of prognosis: a systematic review. Diagnostics 11:1004. https://doi.org/10.3390/diagnostics11061004
Yan K-X, Liu L, Li H (2021) Application of machine learning in oral and maxillofacial surgery. Artif Intell Med Imaging 2:104–114. https://doi.org/10.35711/aimi.v2.i6.104
Shujaat S, Bornstein MM, Price JB, Jacobs R (2021) Integration of imaging modalities in digital dental workflows - possibilities, limitations, and potential future developments. Dentomaxillofacial Radiol 50:20210268. https://doi.org/10.1259/dmfr.20210268
Leite AF, Vasconcelos KD, Willems H et al (2020) Radiomics and machine learning in oral healthcare. Proteomics Clin Appl 14(3):e1900040. https://doi.org/10.1002/prca.201900040
Singh GD, Singh M (2021) Virtual surgical planning: modeling from the present to the future. J Clin Med 10(23):5655. https://doi.org/10.3390/jcm10235655
van Eijnatten M, Koivisto J, Karhu K et al (2017) The impact of manual threshold selection in medical additive manufacturing. Int J Comput Assist Radiol Surg 12:607–615. https://doi.org/10.1007/s11548-016-1490-4
Hung K, Yeung AWK, Tanaka R, Bornstein MM (2020) Current applications, opportunities, and limitations of AI for 3D imaging in dental research and practice. Int J Environ Res Public Health 17:1–18. https://doi.org/10.3390/ijerph17124424
Nagarajappa A, Dwivedi N, Tiwari R (2015) Artifacts: the downturn of CBCT image. J Int Soc Prev Community Dent 5:440. https://doi.org/10.4103/2231-0762.170523
Jacobs R, Salmon B, Codari M et al (2018) Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Health 18:88. https://doi.org/10.1186/S12903-018-0523-5
Weiss R, Read-Fuller A (2019) Cone beam computed tomography in oral and maxillofacial surgery: an evidence-based review. Dent J 7:52. https://doi.org/10.3390/dj7020052
Gaêta-Araujo H, Alzoubi T, de Faria VK et al (2020) Cone beam computed tomography in dentomaxillofacial radiology: a two-decade overview. Dentomaxillofacial Radiol 49:20200145. https://doi.org/10.1259/DMFR.20200145
Luo D, Zeng W, Chen J, Tang W (2021) Deep learning for automatic image segmentation in stomatology and its clinical application. Front Med Technol 3:68. https://doi.org/10.3389/fmedt.2021.767836
Dot G, Schouman T, Dubois G et al (2022) Fully automatic segmentation of craniomaxillofacial CT scans for computer-assisted orthognathic surgery planning using the nnU-Net framework. Eur Radiol 32:3639–3648. https://doi.org/10.1007/s00330-021-08455-y
Leonardi R, Giudice AL, Farronato M et al (2021) Fully automatic segmentation of sinonasal cavity and pharyngeal airway based on convolutional neural networks. Am J Orthod Dentofacial Orthop 159:824-835.e1. https://doi.org/10.1016/j.ajodo.2020.05.017
Shujaat S, Jazil O, Willems H et al (2021) Automatic segmentation of the pharyngeal airway space with convolutional neural network. J Dent 111:103705. https://doi.org/10.1016/j.jdent.2021.103705
Lo Giudice A, Ronsivalle V, Spampinato C et al (2021) Fully automatic segmentation of the mandible based on convolutional neural networks (CNNs). Orthod Craniofac Res 2:100–107. https://doi.org/10.1111/ocr.12536
Morgan N, Van Gerven A, Smolders A et al (2022) Convolutional neural network for automatic maxillary sinus segmentation on cone-beam computed tomographic images. Sci Rep 12:7523. https://doi.org/10.1038/s41598-022-11483-3
Wang H, Minnema J, Batenburg KJ et al (2021) Multiclass CBCT image segmentation for orthodontics with deep learning. J Dent Res 100:943–949. https://doi.org/10.1177/00220345211005338
Cui Z, Fang Y, Mei L et al (2022) A fully automatic AI system for tooth and alveolar bone segmentation from cone-beam CT images. Nat Commun 13:2096. https://doi.org/10.1038/s41467-022-29637-2
Lahoud P, EzEldeen M, Beznik T et al (2021) Artificial intelligence for fast and accurate 3-dimensional tooth segmentation on cone-beam computed tomography. J Endod 47:827–835. https://doi.org/10.1016/j.joen.2020.12.020
Yang fa W, Su YX (2021) Artificial intelligence-enabled automatic segmentation of skull CT facilitates computer-assisted craniomaxillofacial surgery. Oral Oncol 118:105360. https://doi.org/10.1016/j.oraloncology.2021.105360
Verhelst PJ, Smolders A, Beznik T et al (2021) Layered deep learning for automatic mandibular segmentation in cone-beam computed tomography. J Dent 114:103786. https://doi.org/10.1016/j.jdent.2021.103786
Shaheen E, Leite A, Alqahtani KA et al (2021) A novel deep learning system for multi-class tooth segmentation and classification on cone beam computed tomography A validation study: deep learning for teeth segmentation and classification. J Dent 115:103865. https://doi.org/10.1016/j.jdent.2021.103865
Lahoud P, Diels S, Niclaes L et al (2022) Development and validation of a novel artificial intelligence driven tool for accurate mandibular canal segmentation on CBCT. J Dent 116:103891. https://doi.org/10.1016/j.jdent.2021.103891
Kearney V, Chan JW, Valdes G et al (2018) The application of artificial intelligence in the IMRT planning process for head and neck cancer. Oral Oncol 87:111–116. https://doi.org/10.1016/j.oraloncology.2018.10.026
Minnema J, van Eijnatten M, Hendriksen AA et al (2019) Segmentation of dental cone-beam CT scans affected by metal artifacts using a mixed-scale dense convolutional neural network. Med Phys 46:5027–5035. https://doi.org/10.1002/mp.13793
Fontenele RC, do Nascimento Gerhardt M, Pinto JC, et al (2022) Influence of dental fillings and tooth type on the performance of a novel artificial intelligence-driven tool for automatic tooth segmentation on CBCT images–a validation study. J Dent 119:104069. https://doi.org/10.1016/j.jdent.2022.104069
Wang L, Gao Y, Shi F et al (2016) Automated segmentation of dental CBCT image with prior-guided sequential random forests. Med Phys 43:336–346. https://doi.org/10.1118/1.4938267
Liu Z, Liu X, Xiao B et al (2020) Segmentation of organs-at-risk in cervical cancer CT images with a convolutional neural network. Phys Medica 69:184–191. https://doi.org/10.1016/j.ejmp.2019.12.008
El-Gamal FEZA, Elmogy M, Atwan A (2016) Current trends in medical image registration and fusion. Egypt Informatics J 17:99–124. https://doi.org/10.1016/j.eij.2015.09.002
Qin C, Mai Y, Chen X (2021) Registration in oral and maxillofacial surgery. In: Egger J, Chen X (eds) Computer-aided oral and maxillofacial surgery: developments, applications, and future perspectives, 1st edn. Elsevier Science Publishing, Academic Press, San Diego, p 29–54. https://doi.org/10.1016/b978-0-12-823299-6.00002-x
Dai J, Wang X, Dong Y et al (2012) Two- and three-dimensional models for the visualization of jaw tumors based on CT-MRI image fusion. J Craniofac Surg 23:502–508. https://doi.org/10.1097/SCS.0b013e31824cd433
Jang TJ, Yun HS, Kim J-E, et al (2021) Fully automatic integration of dental CBCT images and full-arch intraoral impressions with stitching error correction via individual tooth segmentation and identification. arXiv preprint. https://arxiv.org/abs/2112.01784
Loeffelbein DJ, Kesting MR, Mielke E et al (2007) Bildfusion von SPECT und CT als präzisierende Diagnostik von malignen Tumoren im Mund-Kiefer-Gesichtsbereich. Mund - Kiefer - und Gesichtschirurgie 11:33–41. https://doi.org/10.1007/s10006-006-0039-z
Ayoub AF, Xiao Y, Khambay B et al (2007) Towards building a photo-realistic virtual human face for craniomaxillofacial diagnosis and treatment planning. Int J Oral Maxillofac Surg 36:423–428. https://doi.org/10.1016/j.ijom.2007.02.003
Maal TJJ, Plooij JM, Rangel FA et al (2008) The accuracy of matching three-dimensional photographs with skin surfaces derived from cone-beam computed tomography. Int J Oral Maxillofac Surg 37:641–646. https://doi.org/10.1016/J.IJOM.2008.04.012
Baan F, Bruggink R, Nijsink J et al (2020) Fusion of intra-oral scans in cone-beam computed tomography scans. Clin Oral Investig 25:77–85. https://doi.org/10.1007/s00784-020-03336-y
Chung M, Lee J, Song W et al (2020) Automatic registration between dental cone-beam CT and scanned surface via deep pose regression neural networks and clustered similarities. IEEE Trans Med Imaging 39:3900–3909. https://doi.org/10.1109/TMI.2020.3007520
Flügge T, Derksen W, te Poel J et al (2017) Registration of cone beam computed tomography data and intraoral surface scans – a prerequisite for guided implant surgery with CAD/CAM drilling guides. Clin Oral Implants Res 28:1113. https://doi.org/10.1111/CLR.12925
Li J, Wang Y, Wang S et al (2021) Landmark-guided rigid registration for temporomandibular joint MRI-CBCT images with large field-of-view difference. Lect Notes Comput Sci 12966(LNCS):527–536. https://doi.org/10.1007/978-3-030-87589-3_54
Chen Z, Mo S, Fan X et al (2021) A meta-analysis and systematic review comparing the effectiveness of traditional and virtual surgical planning for orthognathic surgery: based on randomized clinical trials. J Oral Maxillofac Surg 79:471.e1-471.e19. https://doi.org/10.1016/j.joms.2020.09.005
Vannier MW, Marsh JL, Warren JO (1984) Three dimensional CT reconstruction images for reconstruction images for craniofacial surgical planning and evaluation. Radiology 150:179–184. https://doi.org/10.1148/radiology.150.1.6689758
De Riu G, Virdis PI, Meloni SM et al (2018) Accuracy of computer-assisted orthognathic surgery. J Cranio-Maxillofacial Surg 46:293–298. https://doi.org/10.1016/j.jcms.2017.11.023
ter Horst R, van Weert H, Loonen T et al (2021) Three-dimensional virtual planning in mandibular advancement surgery: soft tissue prediction based on deep learning. J Cranio-Maxillofacial Surg 49:775–782. https://doi.org/10.1016/j.jcms.2021.04.001
Wu J, Heike C, Birgfeld C et al (2016) Measuring symmetry in children with unrepaired cleft lip: defining a standard for the three-dimensional midfacial reference plane. Cleft Palate-Craniofacial J 53:695–704. https://doi.org/10.1597/15-053
da Silva RDC, Jenkyn TR, Carranza VA (2021) Convolutional neural networks and geometric moments to identify the bilateral symmetric midplane in facial skeletons from CT scans. Biology (Basel) 10:1–15. https://doi.org/10.3390/biology10030182
Wang C, Zhu X, Hong JC, Zheng D (2019) Artificial intelligence in radiotherapy treatment planning: present and future. Technol Cancer Res Treat 18: 1–11. https://doi.org/10.1177/1533033819873922
Lee S, Yang J, Han J (2012) Development of a decision making system for selection of dental implant abutments based on the fuzzy cognitive map. Expert Syst Appl 39:11564–11575. https://doi.org/10.1016/j.eswa.2012.04.032
Polášková A, Feberová J, Dostálová T, et al (2013) Clinical decision support system in dental implant planning. Mefanet J 1:11–14. https://mj.mefanet.cz/mj-01130312
Szejka AL, Rudek M, Canciglieri Jr O (2013) A reasoning system to support the dental implant planning process. In: Stjepandić J, Rock G, Bil C (eds) Concurrent engineering approaches for sustainable product development in a multi-disciplinary environment. Proceedings of the 19th ISPE International Conference on Concurrent Engineering, 1st edn. Springer, London, pp 909–919. https://doi.org/10.1007/978-1-4471-4426-7_77
Sadighpour L, Rezaei S, Paknejad M et al (2014) The application of an artificial neural network to support decision making in edentulous maxillary implant prostheses. J Res Pract Dent 2014:i1–i10. https://doi.org/10.5171/2014.369025
Bayrakdar SK, Orhan K, Bayrakdar IS et al (2021) A deep learning approach for dental implant planning in cone-beam computed tomography images. BMC Med Imaging 21:1–9. https://doi.org/10.1186/s12880-021-00618-z
Alsomali M, Alghamdi S, Alotaibi S et al (2022) Development of a deep learning model for automatic localization of radiographic markers of proposed dental implant site locations. Saudi Dent J 34:220–225. https://doi.org/10.1016/j.sdentj.2022.01.002
Teizer J, Blickle A, King T, et al (2018) BIM for 3D printing in construction. In: Borrmann A, König M, Koch C, Beetz J (eds) Building information modeling: technology foundations and industry practice, 1st edn, Springer, Switzerland, pp 421–446. https://doi.org/10.1007/978-3-319-92862-3_26
Shilo D, Emodi O, Blanc O et al (2018) Printing the future—updates in 3D printing for surgical applications. Rambam Maimonides Med J 9:e0020. https://doi.org/10.5041/RMMJ.10343
Li J, Gsaxner C, Pepe A et al (2021) Synthetic skull bone defects for automatic patient-specific craniofacial implant design. Sci Data 8:1–8. https://doi.org/10.1038/s41597-021-00806-0
Kodym O, Španěl M, Herout A (2021) Deep learning for cranioplasty in clinical practice: going from synthetic to real patient data. Comput Biol Med 137:104766. https://doi.org/10.1016/j.compbiomed.2021.104766
Mine Y, Suzuki S, Eguchi T, Murayama T (2020) Applying deep artificial neural network approach to maxillofacial prostheses coloration. J Prosthodont Res 64:296–300. https://doi.org/10.1016/j.jpor.2019.08.006
Baumann FW, Sekulla A, Hassler M et al (2018) Trends of machine learning in additive manufacturing. Int J Rapid Manuf 7:310. https://doi.org/10.1504/ijrapidm.2018.095788
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shujaat, S., Riaz, M. & Jacobs, R. Synergy between artificial intelligence and precision medicine for computer-assisted oral and maxillofacial surgical planning. Clin Oral Invest 27, 897–906 (2023). https://doi.org/10.1007/s00784-022-04706-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04706-4