Abstract
Objectives
The purpose of this randomized clinical trial (RCT) is to compare xenogeneic collagen matrix (XCM) versus subepithelial connective tissue graft (SCTG) to increase soft tissue thickness at implant site.
Materials and methods
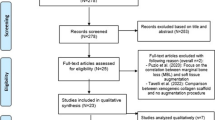
The study was a randomized, parallel-group controlled investigation. Thirty patients underwent buccal soft tissue thickness augmentation at the stage of implant placement by two different methods: SCTG (control group) and XCM (test group). Primary outcome was the amount of buccal soft tissue thickness gain, 3 months after the intervention. Secondary outcomes were the operation time, the amount of keratinized mucosa (KM), pain syndrome (PS), and patients’ quality of life (QL). Histologic evaluation was also performed.
Results
The amount of soft tissue thickness gain was 1.55±0.11 mm in SCTG group, and 1.18±0.11mm in XCM group. The difference between the SCTG and XCM was −0.366 (−0.66 to −0.07; p=0.016). Operation time with XCM was 8.4 (3.737 to 13.06) min shorter than that with the SCTG (p=0.001). KT, PS, and QL for both groups were not statistically significantly different at any time point (p>0.05). At histological examination, the general picture in both groups was similar. No significant differences between the studied groups in most indices, except for the average and maximum formation thickness, cellularity of the basal, mitotic activity and also maximum length of rete ridges.
Conclusion
Within limitations, this study demonstrates that the use of SCTG provides a statistically significant superior soft tissue thickness gain than XCM for soft tissue augmentation procedures around implants.
Clinical relevance
XCM can be used as the method of choice for increasing the thickness of soft tissues.

















Similar content being viewed by others
References
Tarasenko S, Ashurko I, Taschieri S, Repina S, Esaya NA, Corbella S (2020) Comparative analysis of methods to increase the amount of keratinized mucosa before stage-two surgery: a randomized controlled study. Quintessence Int 51(5):374–387. https://doi.org/10.3290/j.qi.a44216
Avila-Ortiz G, Gonzalez-Martin O, Couso-Queiruga E, Wang HL (2020) The peri-implant phenotype. J Periodontol 91(3):283–288. https://doi.org/10.1002/JPER.19-0566
Schroeder A, van der Zypen E, Stich H, Sutter F (1981) The reactions of bone, connective tissue, and epithelium to endosteal implants with titanium-sprayed surfaces. J Maxillofac Surg 9(1):15–25. https://doi.org/10.1016/s0301-0503(81)80007-0
Warrer K, Buser D, Lang NP, Karring T (1995) Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res 6(3):131–138. https://doi.org/10.1034/j.1600-0501.1995.060301.x
Strub JR, Gaberthüel TW, Grunder U (1991) The role of attached gingiva in the health of peri-implant tissue in dogs. 1. Clinical findings. Int J Periodontics Restorative Dent 11(4):317–333
Schrott AR, Jimenez M, Hwang JW, Fiorellini J, Weber HP (2009) Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res 20(10):1170–1177. https://doi.org/10.1111/j.1600-0501.2009.01795.x
Zigdon H, Machtei EE (2008) The dimensions of keratinized mucosa around implants affect clinical and immunological parameters. Clin Oral Implants Res 19(4):387–392. https://doi.org/10.1111/j.1600-0501.2007.01492.x
Chung DM, Oh TJ, Shotwell J, Misch CE, Wang HL (2006) Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol 77(8):1410–1420. https://doi.org/10.1902/jop.2006.050393
Roccuzzo M, De Angelis N, Bonino L, Aglietta M (2010) Ten-year results of a three-arm prospective cohort study on implants in periodontally compromised patients. Part 1: Implant loss and radiographic bone loss. Clin Oral Implants Res 21(5):490–496. https://doi.org/10.1111/j.1600-0501.2009.01886.x
Roccuzzo M, Grasso G, Dalmasso P (2016) Keratinized mucosa around implants in partially edentulous posterior mandible: 10-year results of a prospective comparative study. Clin Oral Implants Res 27(4):491–496. https://doi.org/10.1111/clr.12563
Yeung SC (2008) Biological basis for soft tissue management in implant dentistry. Aust Dent J. 53(Suppl 1):S39–S42. https://doi.org/10.1111/j.1834-7819.2008.00040.x
Thoma DS, Naenni N, Figuero E, Hämmerle C, Schwarz F, Jung RE, Sanz-Sánchez I (2018) Effects of soft tissue augmentation procedures on peri-implant health or disease: a systematic review and meta-analysis. Clin Oral Implants Res 29(Suppl 15):32–49. https://doi.org/10.1111/clr.13114
Berglundh T, Lindhe J (1996) Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol 23(10):971–973. https://doi.org/10.1111/j.1600-051x.1996.tb00520.x
Longoni S, Tinto M, Pacifico C, Sartori M, Andreano A (2019) Effect of peri-implant keratinized tissue width on tissue health and stability: systematic review and meta-analysis. Int J Oral Maxillofac Implants 34(6):1307–1317. https://doi.org/10.11607/jomi.7622
Monje A, Blasi G (2019) Significance of keratinized mucosa/gingiva on peri-implant and adjacent periodontal conditions in erratic maintenance compliers. J Periodontol 90(5):445–453. https://doi.org/10.1002/JPER.18-0471
Lorenzo R, García V, Orsini M, Martin C, Sanz M (2012) Clinical efficacy of a xenogeneic collagen matrix in augmenting keratinized mucosa around implants: a randomized controlled prospective clinical trial. Clin Oral Implants Res 23(3):316–324. https://doi.org/10.1111/j.1600-0501.2011.02260.x
Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M (2009) Clinical evaluation of a new collagen matrix (Mucograft® prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 36(10):868–876. https://doi.org/10.1111/j.1600-051X.2009.01460.x
Jung RE, Sailer I, Hämmerle CH, Attin T, Schmidlin P (2007) In vitro color changes of soft tissues caused by restorative materials. Int J Periodontics Restorative Dent 27(3):251–257
Linkevicius T, Linkevicius R, Alkimavicius J, Linkeviciene L, Andrijauskas P, Puisys A (2018) Influence of titanium base, lithium disilicate restoration and vertical soft tissue thickness on bone stability around triangular-shaped implants: a prospective clinical trial. Clin Oral Implants Res 29(7):716–724. https://doi.org/10.1111/clr.13263
Thoma DS, Gil A, Hämmerle CHF, Jung RE (2000) Management and prevention of soft tissue complications in implant dentistry. Periodontol 88(1):116–129. https://doi.org/10.1111/prd.12415
Schwarz F, Ramanauskaite A (2022) It is all about peri-implant tissue health. Periodontol 2000 88(1):9–12. https://doi.org/10.1111/prd.12407
Frost NA, Mealey BL, Jones AA, Huynh-Ba G (2015) Periodontal biotype: gingival thickness as it relates to probe visibility and buccal plate thickness. J Periodontol. 86(10):1141–1149. https://doi.org/10.1902/jop.2015.140394
van Eekeren P, van Elsas P, Tahmaseb A, Wismeijer D (2017) The influence of initial mucosal thickness on crestal bone change in similar macrogeometrical implants: a prospective randomized clinical trial. Clin Oral Implants Res 28(2):214–218. https://doi.org/10.1111/clr.12784
Linkevicius T, Apse P, Grybauskas S, Puisys A (2009) The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants 24(4):712–719. http://www.ncbi.nlm.nih.gov/pubmed/19885413
Linkevicius T, Apse P, Grybauskas S, Puisys A (2010) Influence of thin mucosal tissues on crestal bone stability around implants with platform switching: a 1-year pilot study. J Oral Maxillofac Surg 68(9):2272–2277. https://doi.org/10.1016/j.joms.2009.08.018
Suárez-López Del Amo F, Lin GH, Monje A, Galindo-Moreno P, Wang HL (2016) Influence of soft tissue thickness on peri-implant marginal bone loss: a systematic review and meta-analysis. J Periodontol 87(6):690–699. https://doi.org/10.1902/jop.2016.150571
Giannobile WV, Jung RE, Schwarz F, Groups of the 2nd Osteology Foundation Consensus Meeting (2018) Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology Foundation Consensus Report Part 1-Effects of soft tissue augmentation procedures on the maintenance of peri-implant soft tissue health. Clin Oral Implants Res 29(Suppl 15):7–10. https://doi.org/10.1111/clr.13110
Baldi N, Buti J, Mensi M, Alfonsi F, Cinquini C, Tonelli P, Barone A (2020) Xenogeneic dermal matrix versus autologous connective tissue graft versus no graft at abutment connection for improving aesthetics: 6 month outcomes of a randomised controlled trial. Clin Trials Dent 2(2):49–62. https://doi.org/10.36130/ctd.03.2020.05
Cairo F, Barbato L, Tonelli P, Batalocco G, Pagavino G, Nieri M (2017) Xenogeneic collagen matrix versus connective tissue graft for buccal soft tissue augmentation at implant site. A randomized, controlled clinical trial. J Clin Periodontol 44(7):769–776. https://doi.org/10.1111/jcpe.12750
Schmitt CM, Brückbauer P, Schlegel KA, Buchbender M, Adler W, Matta RE (2021) Volumetric soft tissue alterations in the early healing phase after peri- implant soft tissue contour augmentation with a porcine collagen matrix versus the autologous connective tissue graft: a controlled clinical trial. J Clin Periodontol 48(1):145–162. https://doi.org/10.1111/jcpe.13387
Roccuzzo M, Dalmasso P, Pittoni D, Roccuzzo A (2019) Treatment of buccal soft tissue dehiscence around single implant: 5-year results from a prospective study. Clin Oral Investig. 23(4):1977–1983. https://doi.org/10.1007/s00784-018-2634-4
Sanz-Martín I, Rojo E, Maldonado E, Stroppa G, Nart J, Sanz M (2019) Structural and histological differences between connective tissue grafts harvested from the lateral palatal mucosa or from the tuberosity area. Clin Oral Investig 23(2):957–964. https://doi.org/10.1007/s00784-018-2516-9
Gargallo-Albiol J, Barootchi S, Tavelli L, Wang HL (2019) Efficacy of xenogeneic collagen matrix to augment peri-implant soft tissue thickness compared with autogenous connective tissue graft: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 34(5):1059–1069. https://doi.org/10.11607/jomi.7497
Thoma DS, Gasser T, Jung RE, Hämmerle C (2020) Randomized controlled clinical trial comparing implant sites augmented with a volume-stable collagen matrix or an autogenous connective tissue graft: 3-year data after insertion of reconstructions. J Clin Periodontol 47(5):630–639. https://doi.org/10.1111/jcpe.13271
Vallecillo C, Toledano-Osorio M, Vallecillo-Rivas M, Toledano M, Rodriguez-Archilla A, Osorio R (2021) Collagen matrix vs. autogenous connective tissue graft for soft tissue augmentation: a systematic review and meta-analysis. Polymers (Basel) 13(11):1810. https://doi.org/10.3390/polym13111810
De Angelis P, De Angelis S, Passarelli PC, Liguori MG, Pompa G, Papi P, Manicone PF, D’Addona A (2021) Clinical comparison of a xenogeneic collagen matrix versus subepithelial autogenous connective tissue graft for augmentation of soft tissue around implants. Int J Oral Maxillofac Surg 50(7):956–963. https://doi.org/10.1016/j.ijom.2020.11.014
Sasagawa A, Igarashi K, Ueda K, Hiroyasu K, Watanabe F (2022) Peri-implant tissue augmentation by volume-stable collagen matrix transplantation: a study of dog mandibles. Odontology 10(1):81–91. https://doi.org/10.1007/s10266-021-00639-8
Huber S, Zeltner M, Hämmerle C, Jung RE, Thoma DS (2018) Non-interventional 1-year follow-up study of peri-implant soft tissues following previous soft tissue augmentation and crown insertion in single-tooth gaps. J Clin Periodontol 45(4):504–512. https://doi.org/10.1111/jcpe.12865
Zeltner M, Jung RE, Hämmerle CH, Hüsler J, Thoma DS (2017) Randomized controlled clinical study comparing a volume-stable collagen matrix to autogenous connective tissue grafts for soft tissue augmentation at implant sites: linear volumetric soft tissue changes up to 3 months. J Clin Periodontol 44(4):446–453. https://doi.org/10.1111/jcpe.12697
Thoma DS, Zeltner M, Hilbe M, Hämmerle CH, Hüsler J, Jung RE (2016) Randomized controlled clinical study evaluating effectiveness and safety of a volume-stable collagen matrix compared to autogenous connective tissue grafts for soft tissue augmentation at implant sites. J Clin Periodontol 43(10):874–885. https://doi.org/10.1111/jcpe.12588
Wiesner G, Esposito M, Worthington H, Schlee M (2010) Connective tissue grafts for thickening peri-implant tissues at implant placement. One-year results from an explanatory split-mouth randomised controlled clinical trial. Eur. J Oral Implantol. 3(1):27–35
General Assembly of the World Medical Association (2014) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent 81(3):14–18. https://doi.org/10.1093/acprof:oso/9780199241323.003.0025
Rojo E, Stroppa G, Sanz-Martin I, Gonzalez-Martín O, Alemany AS, Nart J (2018) Soft tissue volume gain around dental implants using autogenous subepithelial connective tissue grafts harvested from the lateral palate or tuberosity area. A randomized controlled clinical study. J Clin Periodontol. 45(4):495–503. https://doi.org/10.1111/jcpe.12869
Gaston-Johansson F, Albert M, Fagan E, Zimmerman L (1990) Similarities in pain descriptions of four different ethnic-culture groups. J Pain Symptom Manage 5(2):94–100. https://doi.org/10.1016/s0885-3924(05)80022-3
Puisys A, Linkevicius T (2015) The influence of mucosal tissue thickening on crestal bone stability around bone-level implants. A prospective controlled clinical trial. Clin Oral Implants Res 26(2):123–129. https://doi.org/10.1111/clr.12301
Froum SJ, Khouly I, Tarnow DP, Froum S, Rosenberg E, Corby P, Kye W, Elian N, Schoor R, Cho SC (2015) The use of a xenogeneic collagen matrix at the time of implant placement to increase the volume of buccal soft tissue. Int J Periodontics Restor Dent 35(2):179–189. https://doi.org/10.11607/prd.2226
Naenni N, Walter P, Hämmerle CHF, Jung RE, Thoma DS (2021) Augmentation of soft tissue volume at pontic sites: a comparison between a cross-linked and a non-cross-linked collagen matrix. Clin Oral Investig 25(3):1535–1545. https://doi.org/10.1007/s00784-020-03461-8
Verardi S, Orsini M, Lombardi T, Ausenda F, Testori T, Pulici A, Oreglia F, Valente NA, Stacchi C (2020) Comparison between two different techniques for peri-implant soft tissue augmentation: porcine dermal matrix graft versus tenting screw. J Periodontol. 91(8):1011–1017. https://doi.org/10.1002/JPER.19-0447
Schallhorn R, McClain P, Charles A, Clem D, Newman M (2015) Evaluation of a porcine collagen matrix used to augment keratinized tissue and increase soft tissue thickness around existing dental implants. Int J Periodontics Restor Dent. 35(1):99–103. https://doi.org/10.11607/prd.1888
Cosyn J, Eeckhout C, Younes F, Christiaens V, Eghbali A, Vervaeke S, Younes F, De Bruyckere T (2021) A multi-centre randomized controlled trial comparing connective tissue graft with collagen matrix to increase soft tissue thickness at the buccal aspect of single implants : 3-month results. J Clin Periodontol. 48(12):1502–1515. https://doi.org/10.1111/jcpe.13560
Eeckhout C, Bouckaert E, Verleyen D, De Bruyckere T, Cosyn J (2020) A 3-year prospective study on a porcine-derived acellular collagen matrix to re-establish convexity at the buccal aspect of single implants in the molar area: a volumetric analysis. J Clin Med. 9(5):1568. https://doi.org/10.3390/jcm9051568
Puzio M, Błaszczyszyn A, Hadzik J, Dominiak M (2018) Ultrasound assessment of soft tissue augmentation around implants in the aesthetic zone using a connective tissue graft and xenogeneic collagen matrix – 1-year randomised follow-up. Ann Anat. 217:129–141. https://doi.org/10.1016/j.aanat.2017.11.003
Puisys A, Auzbikaviciute V, Vindasiute-Narbute E, Zukauskas S, Razukevicus D, Dard MM (2021) Full versus partial thickness flap to determine differentiation and over keratinization of non-keratinized mucosa. A 3-year split mouth randomized pilot study. Clin Exp Dent Res 7(6):1061–1068. https://doi.org/10.1002/cre2.468
Hélio M, Daiane P, Elizabeth M, Marcelo N, Ana B, Julio J (2019) Peri-implant soft tissue augmentation with palate subepitelial connective tissue graft compared to porcine collagen matrix: A randomized controlled clinical study and histomorphometric analysis. 319. Int J Appl Dent Sci 5(3):319–325
Schmitt CM, Schlegel KA, Gammel L, Moest T (2019) Gingiva thickening with a porcine collagen matrix in a preclinical dog model: histological outcomes. J Clin Periodontol 46(12):1273–1281. https://doi.org/10.1111/jcpe.13196
Author information
Authors and Affiliations
Contributions
Igor Ashurko: conceptualization; methodology; data curation; investigation; writing—original draft; writing—review and editing.
Svetlana Tarasenko: data curation; project administration; supervision.
Aleksandr Esayan: investigation.
Alexandr Kurkov: investigation; visualization; writing—original draft.
Karen Mikaelyan: investigation.
Maxim Balyasin: formal analysis; visualization.
Anna Galyas: writing—review and editing.
Julia Kustova: writing—review and editing.
Silvio Taschieri: data curation; project administration; supervision; writing—review and editing.
Stefano Corbella: data curation; project administration; supervision; writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ashurko, I., Tarasenko, S., Esayan, A. et al. Connective tissue graft versus xenogeneic collagen matrix for soft tissue augmentation at implant sites: a randomized-controlled clinical trial. Clin Oral Invest 26, 7191–7208 (2022). https://doi.org/10.1007/s00784-022-04680-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04680-x