Abstract
Objectives
The aim of this study was to characterize polycaprolactone-based nanofiber scaffolds (PCL) incorporated with calcium hydroxide (CH) and evaluate their bioactivity on human dental pulp cells (HDPCs) when loaded with fibronectin (FN).
Materials and methods
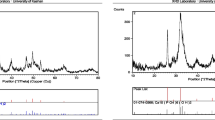
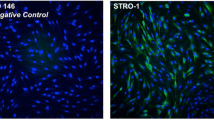
CH (0.1%; 0.2%; 0.4% w/v; or 0%) was incorporated into PCL (10% w/v) scaffolds prepared by electrospinning. Morphology and composition were characterized using SEM/EDS. HDPCs were seeded on the scaffolds and evaluated for viability (alamarBlue; Live/Dead), and adhesion/spreading (F-actin). Next, scaffolds containing 0.4% CH were loaded with FN (20 µg/mL). HDPCs were evaluated for viability, adhesion/spreading, migration (Trans-well), gene expression (RT-qPCR), alkaline phosphatase activity (ALP), and mineralization nodules (Alizarin Red). Data were submitted to ANOVA and post-hoc tests (α = 5%).
Results
Nanofibers with larger diameter were seen as CH concentration increased, while there was no effect on interfibrillar spaces. An increase in cell viability was seen for 0.4% CH, in all periods. Incorporation of CH and FN into the scaffolds increased cellular migration, spread, and viability, all intensified when CH and FN were combined. ALPL and DSPP expression, and ALP activity were not affected by CH and FN. COL1A1 was downregulated in all groups, while DMP1 was upregulated in the presence of CH, with no differences for the groups loaded with FN. CH increased the formation of mineralized matrix, which was not influenced by FN.
Conclusions
In conclusion, the incorporation of CH enhanced the odontogenic potential of HDPCs, irrespective of the presence of FN. The PCL + 0.4% CH formulation may be a useful strategy for use in dentin tissue engineering.
Clinical relevance
A change in the form of presentation of calcium hydroxide-based materials used for direct pulp capping can increase biocompatibility and prolong the vitality of dental pulp.













Similar content being viewed by others
References
Ferracane JL, Cooper PR, Smith AJ (2010) Can interaction of materials with the dentin-pulp complex contribute to dentin regeneration? Odontology 98(1):2–14. https://doi.org/10.1007/s10266-009-0116-5
Ruch JV, Lesot H, Bègue-Kirn C (1995) Odontoblast differentiation. Int J Dev Biol 39(1):51–68
de Souza Costa CA, Teixeira HM, Lopes do Nascimento AB, Hebling J, (2007) Biocompatibility of resin-based dental materials applied as liners in deep cavities prepared in human teeth. J Biomed Mater Res B Appl Biomater 81(1):175–184. https://doi.org/10.1002/jbm.b.30651
Graham L, Cooper PR, Cassidy N, Nor JE, Sloan AJ, Smith AJ (2006) The effect of calcium hydroxide on solubilisation of bio-active dentine matrix components. Biomaterials 27(14):2865–2873. https://doi.org/10.1016/j.biomaterials.2005.12.020
Aeinehchi M, Eslami B, Ghanbariha M, Saffar AS (2003) Mineral trioxide aggregate (MTA) and calcium hydroxide as pulp-capping agents in human teeth: a preliminary report. Int Endod J 36(3):225–231. https://doi.org/10.1046/j.1365-2591.2003.00652.x
de Souza Costa CA, Hebling J, Scheffel DL, Soares DG, Basso FG, Ribeiro AP (2014) Methods to evaluate and strategies to improve the biocompatibility of dental materials and operative techniques. Dent Mater 30(7):769–784. https://doi.org/10.1016/j.dental.2014.04.010
de Souza Costa CA, Duarte PT, de Souza PP, Giro EM, Hebling J (2008) Cytotoxic effects and pulpal response caused by a mineral trioxide aggregate formulation and calcium hydroxide. Am J Dent 21(4):255–261
Ma PX (2008) Biomimetic materials for tissue engineering. Adv Drug Deliv Rev 60(2):184–198. https://doi.org/10.1016/j.addr.2007.08.041
Galler KM, Eidt A, Schmalz G (2014) Cell-free approaches for dental pulp tissue engineering. J Endod 40(4 Suppl):41–45. https://doi.org/10.1016/j.joen.2014.01.014
Jazayeri HE, Lee SM, Kuhn L, Fahimipour F, Tahriri M, Tayebi L (2020) Polymeric scaffolds for dental pulp tissue engineering: a review. Dent Mater 36(2):e47–e58. https://doi.org/10.1016/j.dental.2019.11.005
Woodruff MA, Hutmacher DW (2010) The return of a forgotten polymer—Polycaprolactone in the 21st century. Prog Polym Sci 35:1217–1256. https://doi.org/10.1016/j.progpolymsci.2010.04.002
Dwivedi R, Kumar S, Pandey R, Mahajan A, Nandana D, Katti DS, Mehrotra D (2020) Polycaprolactone as biomaterial for bone scaffolds: Review of literature. J Oral Biol Craniofac Res 10(1):381–388. https://doi.org/10.1016/j.jobcr.2019.10.003
Pham QP, Sharma U, Mikos AG (2006) Electrospun poly(epsilon-caprolactone) microfiber and multilayer nanofiber/microfiber scaffolds: characterization of scaffolds and measurement of cellular infiltration. Biomacromol 7(10):2796–2805. https://doi.org/10.1021/bm060680j
Bottino MC, Yassen GH, Platt JA, Labban N, Windsor LJ, Spolnik KJ, Bressiani AH (2013) A novel three-dimensional scaffold for regenerative endodontics: materials and biological characterizations. J Tissue Eng Regen Med 9(11):116–123. https://doi.org/10.1002/term.1712
Liu H, Peng H, Wu Y, Zhang C, Cai Y, Xu G, Li Q, Chen X, Ji J, Zhang Y, OuYang HW (2013) The promotion of bone regeneration by nanofibrous hydroxyapatite/chitosan scaffolds by effects on integrin-BMP/Smad signaling pathway in BMSCs. Biomaterials 34(18):4404–1447. https://doi.org/10.1016/j.biomaterials.2013.02.048
Wang P, Zhao L, Chen W, Liu X, Weir MD, Xu HH (2014) Stem cells and calcium phosphate cement scaffolds for bone regeneration. J Dent Res 93(7):618–625. https://doi.org/10.1177/0022034514534689
Roy P, Sailaja RR (2015) Chitosan-nanohydroxyapatite composites: mechanical, thermal and bio-compatibility studies. Int J Biol Macromol 73:170–181. https://doi.org/10.1016/j.ijbiomac.2014.11.023
Soares DG, Rosseto HL, Basso FG, Scheffel DS, Hebling J, Costa CA (2016) Chitosan-collagen biomembrane embedded with calcium-aluminate enhances dentinogenic potential of pulp cells. Braz Oral Res 30(1):e54. https://doi.org/10.1590/1807-3107BOR-2016.vol30.0054
Soares DG, Rosseto HL, Scheffel DS, Basso FG, Huck C, Hebling J, de Souza Costa CA (2017) Odontogenic differentiation potential of human dental pulp cells cultured on a calcium-aluminate enriched chitosan-collagen scaffold. Clin Oral Investig 21(9):2827–2839. https://doi.org/10.1007/s00784-017-2085-3
Okabe T, Sakamoto M, Takeuchi H, Mtsushima K (2006) Effects of pH on mineralization ability of human dental pulp cells. J Endod 32(3):198–201. https://doi.org/10.1016/j.joen.2005.10.041
Yoshiba K, Yoshiba N, Nakamura H, Iwaku M, Ozawa H (1996) Immunolocalization of fibronectin during reparative dentinogenesis in human teeth after pulp capping with calcium hydroxide. J Dent Res 75(8):1590–1597. https://doi.org/10.1177/00220345960750081101
Lawson CD, Burridge K (2014) The on-off relationship of Rho and Rac during integrin-mediated adhesion and cell migration. Small GTPases 5:e27958. https://doi.org/10.4161/sgtp.27958
Howard C, Murray PE, Namerow KN (2010) Dental pulp stem cell migration. J Endod 36(12):1963–1966. https://doi.org/10.1016/j.joen.2010.08.046
Chatakun P, Núñez-Toldrà R, Díaz López EJ, Gil-Recio C, Martínez-Sarrà E, Hernández-Alfaro F, Ferrés-Padró E, Giner-Tarrida L, Atari M (2014) The effect of five proteins on stem cells used for osteoblast differentiation and proliferation: a current review of the literature. Cell Mol Life Sci 71(1):113–142. https://doi.org/10.1007/s00018-013-1326-0
Leite ML, Usberti FR, Ortecho-Zuta U, Bordini EAF, Soares DG, Hebling J, de Souza Costa CA (2019) Synthesis and characterization of nanofibers scaffolds and their biological effects on human pulp cells. Rodyb 1:9–15
Stefani I, Cooper-White JJ (2016) Development of an in-process UV-crosslinked, electrospun PCL/aPLA-co-TMC composite polymer for tubular tissue engineering applications. Acta Biomater 36:231–240. https://doi.org/10.1016/j.actbio.2016.03.013
Soares DG, Basso FG, Hebling J, de Souza Costa CA (2015) Immediate and late analysis of dental pulp stem cells viability after indirect exposition to alternative in-office bleaching strategies. Clin Oral Invest 19(5):1013–1020. https://doi.org/10.1007/s00784-014-1321-3
Leite ML, Soares DG, Anovazzi G, Mendes Soares IP, Hebling J, de Souza Costa CA (2020) Development of fibronectin-loaded nanofiber scaffolds for guided pulp tissue regeneration. J Biomed Mater Res B Appl Biomater 31:e34785. https://doi.org/10.1002/jbm.b.34785
Leite MLAS, Soares DG, Basso FG, Hebling J, de Souza CC (2017) Biostimulatory effects of simvastatin on MDPC-23 odontoblast-like cells. Braz Oral Res 31:e104. https://doi.org/10.1590/1807-3107BOR-2017.vol31.0104
Wang J, Ma H, Jin X, Hu J, Liu X, Ni L, Ma PX (2011) The effect of scaffold architecture on odontogenic differentiation of human dental pulp stem cells. Biomaterials 32(31):7822–7830. https://doi.org/10.1016/j.biomaterials.2011.04.034
Gupte MJ, Ma PX (2012) Nanofibrous scaffolds for dental and craniofacial applications. J Dent Res 91(3):227–234. https://doi.org/10.1177/0022034511417441
Kostopoulos V, Kotrotsos A, Fouriki K, Kalarakis A, Portan D (2020) Fabrication and characterization of polyetherimide electrospun scaffolds modified with graphene nano-platelets and hydroxyapatite nano-particles. Int J Mol Sci 21(2):583. https://doi.org/10.3390/ijms21020583
Farhadian N, Godiny M, Moradi S, Hemati Azandaryani A, Shahlaei M (2018) Chitosan/gelatin as a new nano-carrier system for calcium hydroxide delivery in endodontic applications: development, characterization and process optimization. Mater Sci Eng C Mater Biol Appl 92:540–546. https://doi.org/10.1016/j.msec.2018.07.002
Soares DG, Bordini EAF, Cassiano FB, Bronze-Uhle ES, Pacheco LE, Zabeo G, Hebling J, Lisboa-Filho PN, Bottino MC, de Souza Costa CA (2020) Characterization of novel calcium hydroxide-mediated highly porous chitosan-calcium scaffolds for potential application in dentin tissue engineering. J Biomed Mater Res B Appl Biomater 108(6):2546–2559. https://doi.org/10.1002/jbm.b.34586
Johannsen K, Rademacher S (1999) Modelling the kinetics of calcium hydroxide dissolution in water. Acta hydrochim hydrobiol 27:72–78. https://doi.org/10.1002/(SICI)1521-401X(199902)27:2%3c72::AID-AHEH72%3e3.0.CO;2-H
Liang D, Hsiao BS, Chu B (2007) Functional electrospun nanofibrous scaffolds for biomedical applications. Adv Drug Deliv Rev 59(14):1392–1412. https://doi.org/10.1016/j.addr.2007.04.021
Gorodzha SN, Muslimov AR, Syromotina DS, Timin AS, Tcvetkov NY, Lepik KV, Petrova AV, Surmeneva MA, Gorin DA, Sukhorukov GB, Surmenev RA (2017) A comparison study between electrospun polycaprolactone and piezoelectric poly(3-hydroxybutyrate-co-3-hydroxyvalerate) scaffolds for bone tissue engineering. Colloids Surf B Biointerfaces 160:48–59. https://doi.org/10.1016/j.colsurfb.2017.09.004
Hebling J, Giro EM, Costa CA (1999) Biocompatibility of an adhesive system applied to exposed human dental pulp. J Endod 25(10):676–682. https://doi.org/10.1016/s0099-2399(99)80354-9
Grover C, Shetty N (2014) Evaluation of calcium ion release and change in pH on combining calcium hydroxide with different vehicles. Contemp Clin Dent 5(4):434–439. https://doi.org/10.4103/0976-237X.142803
Hirose Y, Yamaguchi M, Kawabata S, Murakami M, Nakashima M, Gotoh M, Yamamoto T (2016) Effects of extracellular pH on dental pulp cells in vitro. J Endod 42(5):735–741. https://doi.org/10.1016/j.joen.2016.01.019
Sciaky I, Pisanti S (1960) Localization of calcium placed over amputated pulps in dogs’ teeth. J Dent Res 39:1128–1132. https://doi.org/10.1177/00220345600390060601
Kanaya S, Xiao B, Sakisaka Y, Suto M, Maruyama K, Saito M, Nemoto E (2018) Extracellular calcium increases fibroblast growth factor 2 gene expression via extracellular signal-regulated kinase 1/2 and protein kinase A signaling in mouse dental papilla cells. J Appl Oral Sci 14(26):e20170231. https://doi.org/10.1590/1678-7757-2017-0231
Kim JJ, Bae WJ, Kim JM, Kim JJ, Lee EJ, Kim HW, Kim EC (2014) Mineralized polycaprolactone nanofibrous matrix for odontogenesis of human dental pulp cells. J Biomater Appl 28(7):1069–1078. https://doi.org/10.1177/0885328213495903
Jung GY, Park YJ, Han JS (2010) Effects of HA released calcium ion on osteoblast differentiation. J Mater Sci Mater Med 21(5):1649–1654. https://doi.org/10.1007/s10856-010-4011-y
Khoshniat S, Bourgine A, Julien M, Petit M, Pilet P, Rouillon T, Masson M, Gatius M, Weiss P, Guicheux J, Beck L (2011) Phosphate-dependent stimulation of MGP and OPN expression in osteoblasts via the ERK1/2 pathway is modulated by calcium. Bone 48(4):894–902. https://doi.org/10.1016/j.bone.2010.12.002
An S, Gao Y, Ling J, Wei X, Xiao Y (2012) Calcium ions promote osteogenic differentiation and mineralization of human dental pulp cells: implications for pulp capping materials. J Mater Sci Mater Med 23(3):789–795. https://doi.org/10.1007/s10856-011-4531-0
Apáti Á, Berecz T, Sarkadi B (2016) Calcium signaling in human pluripotent stem cells. Cell Calcium 59(2–3):117–123. https://doi.org/10.1016/j.ceca.2016.01.005
Han B, Wang X, Gao X, Liu J, Liang F, Qu X, Yang Z (2011) Synthesis and characterization of biodegradable microcapsules for the controlled delivery of calcium hydroxide. J Biomed Mater Res B Appl Biomater 99B(1):120–126. https://doi.org/10.1002/jbm.b.31878
Takita T, Hayashi M, Takeichi O, Ogiso B, Suzuki N, Otsuka K, Ito K (2006) Effect of mineral trioxide aggregate on proliferation of cultured human dental pulp cells. Int Endod J 39(5):415–422. https://doi.org/10.1111/j.1365-2591.2006.01097.x
Wang X, Jong G, Lin LM, Shimizu E (2013) EphB-EphrinB interaction controls odontogenic/osteogenic differentiation with calcium hydroxide. J Endod 39(10):1256–1260. https://doi.org/10.1016/j.joen.2013.06.016
Mizuno M, Banzai Y (2008) Calcium ion release from calcium hydroxide stimulated fibronectin gene expression in dental pulp cells and the differentiation of dental pulp cells to mineralized tissue forming cells by fibronectin. Int Endod J 41(11):933–938. https://doi.org/10.1111/j.1365-2591.2008.01420.x
Asghari Sana F, Çapkın Yurtsever M, Kaynak Bayrak G, Tunçay EÖ, Kiremitçi AS, Gümüşderelioğlu M (2017) Spreading, proliferation and differentiation of human dental pulp stem cells on chitosan scaffolds immobilized with RGD or fibronectin. Cytotechnology 69(4):617–630. https://doi.org/10.1007/s10616-017-0072-9
Martinez EF, Silva LAH, Furuse C, Araújo NS, Araújo VC (2009) Dentin matrix protein 1 (DMP1) expression in developing human teeth. Braz Dent J 20(5):365–369. https://doi.org/10.1590/s0103-64402009000500002
Omer A, Al-Sharabi N, Qiu Y, Xue Y, Li Y, Fujio M, Mustafa K, Xing Z (2020) Biological responses of dental pulp cells to surfaces modified by collagen 1 and fibronectin. J Biomed Mater Res Part A 108(6):1369–1379. https://doi.org/10.1002/jbm.a.36908
Yeo A, Rai B, Sju E, Cheong JJ, Teoh SH (2008) The degradation profile of novel, bioresorbable PCL-TCP scaffolds: an in vitro and in vivo study. J Biomed Mater Res A 84(1):208–218. https://doi.org/10.1002/jbm.a.31454
Funding
The work was supported by financial support from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (grant 001), the Fundação de Amparo à Pesquisa do Estado de São Paulo (grants 2019/11192–4 and 2019/16473–1) and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (grant 303391/2019–7).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Caroline Ansemi, Igor Paulino Mendes Soares, Maria Luísa Leite, and Fernanda Ali Kitagawa. Founding acquisition, resources, and supervision were performed by Carlos Alberto de Souza Costa and Josimeri Hebling. The first draft of the manuscript was written by Caroline Anselmi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study approval was obtained from the ethics committee of School of Dentistry of Araraquara (CAAE: 18119319.9.0000.5416).
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Anselmi, C., Mendes Soares, I.P., Leite, M.L. et al. Cytocompatibility and bioactivity of calcium hydroxide-containing nanofiber scaffolds loaded with fibronectin for dentin tissue engineering. Clin Oral Invest 26, 4031–4047 (2022). https://doi.org/10.1007/s00784-022-04372-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04372-6